INTRODUCTION
In the European context, the mobility of patients looking for medical care in countries that can offer better healthcare services (from now on called receiving countries) within the continent is categorized in four trends. The first is the mobility of a patient member of the European Union seeking treatments outside the Union, the second is for patients from non-EU (European Union) member countries who seek medical procedures within the Union, while the third is for patients from the EU who demand procedures inside the EU. The fourth trend is patients from European countries not members of the EU that seek medical procedures outside the Union. The third trend is the one with the greatest dynamism as a result of the acquired rights of citizens' members of the EU who receive medical attention with fewer bureaucratic procedures in both public and private clinics, and other health institutions. This is due to the implementation of the Directive on patients' Rights in Cross-border Healthcare adopted by the European Parliament in 2011 (from now on called only Directive) (European Parliament, 2011). The regulation was introduced in response to confusion among patients, healthcare providers and regulatory bodies about the limits on medical supply to citizens of other member countries of the EU.
The Directive codifies existing rights for national patients and does not waive them in other locations within the EU as well as serves as an instrument to facilitate the decision of patients on the demand for medical services outside their country of origin. The Directive is based on regulation 1408/71 offering temporary coverage in members of the EU whether it is in the country of destination or origin with advanced treatment and authorization of its insurance/health entity, in addition to explicit permission of the specialized professional.
However, there are doubts about the implementation of the Directive for patients who are members of the European Union that are subject to procedures outside any member States, since, although it is not within their jurisdiction, there are medical care agreements or non-EU patients in which the Directive would be partially implemented1.
This article analyzes the implication of the decision of the EU patients who search for medical procedures in other member countries or those with health agreements covered by the Directive and patients who are not covered with the Directive in the dynamic of health mobility, specifically the medical insurance market, and the role of the agents involved in the phenomena.
Thus, patient mobility from and to Europe is not a new trend as individuals have searched health improvements for a long time. In the nineteenth century there was an increase in the movement of 25% of people seeking thalassotherapy and thermal treatment as a tourist activity, whereas in the twentieth century, individuals with higher monetary income demanded medical services in Europe. However, at the end of 2016 the outflow of patients who seek medical procedures in other non-EU country due to multiple causes had increased due to restrictions on certain internal procedures and the shortage of specialized physicians (De la Puente, 2015). The growing number of people searching for medical procedures abroad has consolidated the regional market for medical and wellness tourism, generating the need to study the growing dynamic of patient's mobility. The market of health mobility and its implications for the public health sector financing reconfigures the role of patient not only as an agent benefiting from intra-community rights, but also as a consumer willing to disburse monetary resources, thus providing and creating the opportunity for the expansion of medical tourism.
This article also examines the inflow and outflow of patients from the EU, the regional trend of the sector, implications for the organization as a destination for patients seeking better quality at competitive prices, ethical-legal concerns regarding the quality of medical procedures and the legal framework defined so far. A mixed method was used which combined with a qualitative analysis of secondary data found on the demand for medical services in the European Union and in the region, with previous studies carried out on the subject in order to answer whether the regulation on health services of the European Union had a different impact on different segments of the health mobility dynamics including health insurance, patient recruitment, and the medical risks that patients incur when using medical procedures outside Europe. Thus, the general objective is to analyze the impact of the European Union health rights legislation on the dynamics of health mobility, represented in the Directive of 2004. The specific objectives are to analyze the impact of Directive 883/2004 on the consolidation of European medical tourism and to study the role of health insurers, intermediaries and health risks in an environment of partial uncertainty. The hypothesis of this research is that the Directive 883/2004 is the beginning of a greater regulation of health mobility in response to legal gaps generated by a rapidly growing market.
EUROPE AND THE MEDICAL TOURISM MARKET
According to Lunt and Carrera (2011), the arrival of patients to Europe from Middle East and Asia Pacific countries, and the United States increased by 12% due to multiple factors. The first is the availability of high complexity procedures at low cost through subsidies from local governments members of the EU, which lowers the cost of the service to be demanded (either for the patient who covers his expenses with their own resources or foreign governments members of the EU that have an expenditure budget through public offices to care for national patients abroad). Subsidies are often differentiated depending on the political perspective of the local government. This is the case of Spain which, due to its welfare State focus, subsidies procedures of medium and high complexity up to 15% for national, EU and foreign patients.
According to Reisman (2010), health mobility is segmented depending on the type of medical service. In the case of the curative and preventive care countries such as Germany, France, Belgium and Spain, it covers 76% of all patients who search for procedures to cure a preexisting health condition. The most sought after procedures are cardiovascular ones with different purposes, orthopedic interventions, and treatments for long-term diseases, interventions in the urology area, oncologic treatments and low-complexity trauma, representing 73% of the total demanded and consumed (Cortez, 2008). In the aesthetic segment, Spain, Portugal and Italy absorb 65% of the total demand through procedures such as rhinoplasty, liposuction, and treatment of the dermis for aesthetic purposes and removal of minor anomalies in the skin. In the wellness segment Germany, France and Poland represent 75% of the regional consumption through the demand of termal treatment (use of thermal waters for medical purposes and relaxation), and spa (relaxing centers of slight or non-invasive procedures) (Erbeck, 2015). The German case stands out due to a high expenditure per capita representing 21% more than other EU member States. However, despite these consumption patterns, there is insufficient information on the status of in-patient and out-patient consumption dynamics.
There is no consensus at a European level on the identification of health tourism and health mobility patterns since some authors such as Blouin, Drager and Smith (2010) define health tourism as one in which patients voluntarily search medical procedures regardless of the length of stay, while Boffin and Baeten (2005) specifie that health tourism should be based on the length of stay of a patient due to be havioral changes in consumption of medical and tourism services. Without an accepted global definition, it is not possible to determine the number of health tourists arriving in Europe, or the opportunities and risks it represents for local health systems. However, it is accepted that despite lacking a definition, the arrival of patients from other EU Member States is known. Slovenia, Romania, Hungary, Bulgaria and Greece are the ones that send more patients to other medical destinations, mainly for curative and wellness purposes. Approximately 15-23% during the period 2009-2014 (Smith et al, 2014).
Since 2012, Spain is the most sought after place for the demand of medical services due to the low comparative costs versus Germany and France (around 23%) (Smith, et al. 2014) implying a monetary saving of patients for a high-quality health care system and cost deductions (graph 1).
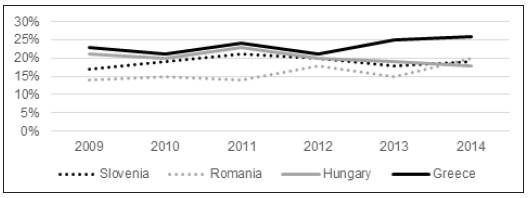
Source: Smith, R. D., Rupa, C., Viroj. (2014). Trade in health-related services. The Lancet, 373, 593.
Graphic 1 countries with the highest percentage of outflow patients outside their borders: 2009-2014
The countries analyzed in graph 1 were selected due to high level of outflow patients looking for medical services of high quality in selected procedures to developed health systems (Germany, Spain, France) mainly searching procedures of oncology, cardiology and neurology. In 2015, Latvia, Lithuania and Estonia have increased their market share of outflow patients demanding treatments against cancer, detachment of the pelvic floor, stem cells procedures and fertility treatments (Cohen, 2015) (graph 2).
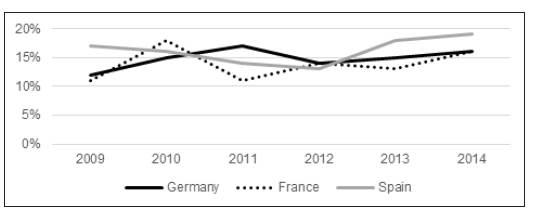
Source: Smith, R. D., Rupa, C., Viroj. (2014). Trade in health-related services. The Lancet, 373, 593.
Graphic 2 Countries with the highest percentage of inflow patients in the European Union: 2009-2014
Other countries such as Malta, Croatia, and Cyprus are attractive for medical procedures in the wellness segment with a high tourism component, sometimes increasing tourism spending more than medical procedures (Cheung, Wilson, 2015).
Regarding the arrival of patients from non-EU member States, Albania and Moldova have the highest participation of outflow patients searching for cardiovascular procedures, highly complex trauma treatments and oncological treatments to Greece, Poland and Austria. Due to the low purchasing power and average per capita spending of these patients, Germany, France and Spain are not the first option (in addition to mobility restrictions to avoid massive arrival of immigrants from Eastern Europe and the Middle East). The following graphs show the percentage of national patients that choose to go to another country to receive medical treatments.
Source: Cheung, I., Wilson, A. (2015). Anthroplasty tourism. Med J Aust. 187, 11-12.
Graphic 3 Percentage of national patients that choose to go to another country to receive medical treatment.
Note that the drop in patient's reception is due to various political crises, as well as internal social conflicts that have limited patient mobility to the EU and opt for other destinations within their own borders. This situation is deepened in former European colonies where, despite having fewer arrival restrictions (bureaucratic visa reduction or exemption, alliances in mobility for educational and health purposes), the patient arrival fell 19% during 2009-2014 (note the case of India where the arrival of patients represented 13% of the total admitted in 2013 and 8% in 2014) (Cormany, Baloglu, 2010).
Lunt, Hardey and Mannion (2010) outline that EU patients who search procedures in other member States also consume around a fourth of their monetary budget in complementary medical goods. Another mobility factor is the decrease in the time of attention offered by the receiving countries.
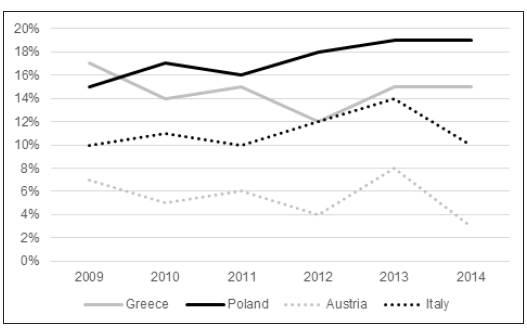
Source: Cheung, I., Wilson, A. (2015). Anthroplasty Tourism. Med J Aust. 187, 11-12.
Graphic 4 EU Member States with the largest number of receiving patients as a percentage of the total patients in European countries outside the EU: 2009-2014.
Another element that Lunt, Hardey and Mannion point out from the profile of EU patients is that the demand for procedures is often volatile (mainly for patients under 35 years of age) as they seek demand different segments of medical services and do not tend to be repetitive in the services demanded. This behavior is different from older patients (older than 35 years old) which are seen as potential clients by the operators of the sector. As for non-EU patients, the authors emphasize that in the last five years patient inflow has increased by 60% representing 78% of the total medical services demanded during the period 2012-2013. It is important to establish that the other 22% belonging to EU and non-EU patients demand medical services on an occasional basis through aesthetic medical procedures such as breast implants, rhinoplasty, liposuction, as well as various procedures in curative medicine.
In that sense, the Directive 883/2004 has facilitated the transfer of EU patients both to internal and external destinations, clarifying information to operators on the division of costs in procedures, and type of remuneration to professionals in the area. Thus, with the regulations, a patient who has a medical condition certified by national authorities in the country of origin and who has restrictions on supply due to shortage of equipment, specialized professionals added to the urgency of medical intervention, can demand the procedure of interest in another EU country that has the necessary elements for the service.
However, there are cases in which countries have bilateral and multilateral partnerships, which ease medical procedures for patients regarding total costs, bureaucratic processes and tax deductions within the Directive framework. It should be noted that when bilateral alliances do not exist and the sending country does not have the resources to pay for medical services to be consumed by the patient, that patients look for ways to receive medical services by entering in Emergency Units, obtaining the receiving country's nationality, thus increasing the public expenditure of the health sector in the long term (De la Puente, 2017).
Despite the above, the Directive seeks to combat this behavior through the European Referential Connection System (Martin, 2012) which, in addition to identifying patient mobility between sending and receiving states, focuses on the global characterization of patients with rare diseases. The possibility of obtaining information on the dynamics of mobility, per capita expenditure, type of procedure demanded and patient profiles has increased the number of operators (clinics, public hospitals, insurance companies, brokers, travel agencies, passenger transportation companies) offering health care packages through vertical alliances (in which a company has divisions in several market segments that combine the offer into one operator) and horizontal alliances (independent companies join forces to offer medical tourism packages).
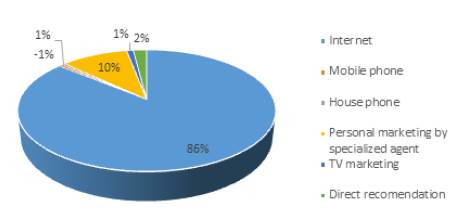
According to Vick (2010), these alliances (mainly the horizontal) increased the number of inflow patients by 23% thanks to collaborative actions in finding complementary services. Internet represents 86% of the instruments for attracting patients due to the direct advertising who seek certain services in specific destinations highlighting the medical procedures in clinics with which they have alliances, the particular accreditations of each clinic or hospital, the specialized professionals, and the medical associations that support the supply. However, there is a dilemma regarding the intermediaries during the process of getting patients, since their operations are financed in many cases by clinics that expect to receive the patients do not know the dilemma.
The following chart shows patient attraction vehicles. Unfortunately, due to data scarcity, there is no segmentation of vehicle of attraction by age, per capita income, and type of procedure to demand, which implies an opportunity to deepen future research. The growth of internet direct marketing is due to the fact that through web platforms there is more access to particular information of potential foreign patients, besides being a vehicle of immediate reception of directed publicity.
The number of specialized marketing personnel or sales agents grew 10% due to the ease and reliability in clarifying doubts against potential risks (De la Puente, 2015a). It is necessary to emphasize that the graph below shows the first contact with potential patients who ended up demanding medical procedures with operators according to various vehicles.
Source: Vick, L. (2010). Medical Tourism: Legal Issues. Destination Health Medical Tourism Conference, Olympia: Michelmorers Solicitors.
Graphic 5 Percentage of growth in medical and health tourists during the period 2004-2010.
Medical and legal implications of the existing legislation in patient mobility
There are several negative implications for patient mobility both within the EU and between the EU and non-EU countries. The first is the regulatory differentiation that could result in legal action of patients for a delay in medical attention because each health system has its own protocols of healthcare services. That is, flexibility in care protocols and medical procedures can result in long-term complications for patients in target locations, which in turn can lead to litigation where the patient is the primary victim. This is not often the case on EU borders since Directive 883/2004 seeks to homogenize the bases of quality and care protocols in low, medium and high-complexity medical institutions with shared regulations (even though the technology and availability of space for invasive/non-invasive interventions supposes a limitation on their compliance).
In the relationship between EU countries and non-EU countries, regulatory gaps are much greater since the Directive does not extend to patient receiving locations to non-EU countries. In addition, the lack of understanding of coverage and quality standards in medical procedures (endorsed by international insurers) increases the risk of non-response or incomplete response to complaints from patients who are not satisfied with the procedures they consumed. However, the guidelines for physical and mental health care according to the World Health Organization (Gallup Organization, 2006) call for the coordination of health systems as opposed to non-homogenization in health care standards and procedural protocols.
The guidelines, however, are only a general framework that countries must implement according to their restrictions on physical, budgetary and human capital resources, which creates an inherent risk for patients who have preexisting medical conditions. This can lead to procedures with undesired results and even serious complications for patients. As a result, many healthcare systems in developing countries do not have legislation to consolidate medical care protocols.
Buffin and Baeten (2005) specify that patient's decisions are based (without differentiating age range or per capita income) on the budget constraint, which implies a general patient's ignorance of postoperative risks that are not directly related to the identification of preexisting medical conditions.
This situation becomes more evident in procedures such as organ transplants that can result in infections or rejection of the organ with a probability of poor or no response beyond private care; that is to say, in case of patient complications and a lack of satisfactory response by the specialist in charge, the host country may take a long time to guarantee the right, while the issuing country often only has diplomatic vehicles as an instrument of pressure. This is the case of Spanish patients who had undergone aesthetic procedures with negative results in clinics without accreditation or permission to operate. (De la Puente, 2015). According to Terzi et al, (2008) 37% of patients from EU member countries have complained to the health authorities in their home country about complications in aesthetic procedures in non-EU countries. Asia Pacific, Latin America and Eastern Europe have the highest percentage of claims with 24%, 19% and 13% respectively (Cormany y Baloglu, 2010).
A way to reduce the patient's own uncertainties lies in the increase of communication between both specialists through the inclusion of this element in international patient care protocols such as the purchase of medical insurance for foreign medical treatments. According to Blouin, Drager and Smith (2010), the growth of medical insurance for extraterritorial medical procedures with premium conditions is greater than 200% compared to inner European insurance premiums (2016).
Graphic 6. shows the percentage variation in international medical insurance with a premium of 200% greater than EU insurance.
Source: Ledger, W., Anumba, D. (2016). The costs of health insurance and life birth. Journal of Plastic, Reconstructive and Aesthetic Surgery, 1, 8.
Graphic 6 Change in extraterritorial medical insurance with premiums above 200% compared to of inter-territorial insurance premiums: 2010-2015
The fall showed in the year 2012 and 2013 is a consequence of the negative impact on demand and insurance due to negative economic conditions according to Ledger and Anumba (2016), where the assurance does not arise as an option of consumption in the short term due to the perception of insurance as a cost added against a questionable materialization or claim. This perspective moves away from the idea that the agent knowing the conditions of assurance and the benefit in the short and long term opts for a known benefit against a context of asymmetric information.
The emphasis on the variation of the monthly health insurance payment premium with changes of 200% compared to complementary insurance in EU territory is mentioned in order to determine the product variable versus its immediately direct comparison. In other words, the price of the premium implies the assumption of greater risks for the purposes of insurance in the event of execution by the patient (usually through intermediary operators in the service consumption operation in the target locality).
The conditions of insurance for patients consuming non-European goods and services are that the medical institution should have international accreditations (preferably from the Journal of Clinical Investigation, McKinsey or Deloitte) in areas of interest of the patient with a validity of no more than two years, compatible protocol with medical institutions of the country of origin, the validation of medical examinations that would be requested in the country of destination, in addition to validations of specialists).
This means a great difficulty in assuring patients who search procedures outside their borders in developing countries with operative deficits mentioned above even when comparative costs are lower. The result is the inherent risk in patient's traveling to other locations with supplementary minimum insurance coverage and limitation in coverage's execution and also lack of effective response in the country of destination.
SCENARIOS FOR EUROPEAN INSURANCE SYSTEMS
The implications are differentiated for both the country of origin and destination. For the first ones the increasing in the insurance market has risen by 30% between 2012-2016 (Ledger and Anumba, 2016). This means that the insurance services in non-European health services emerges as an option for industrial growth against falls in other types of insurance including residential claims and insurance in financial products, which dropped 24.5% during 2012-2016 (De la Puente, 2017). Another positive impact is the increase in alliances between medical institutions through the creation of international offices for the patient's attention headed mainly by private clinics. According to the Federation of Insurance Association (2016) strategic alliances are resulting in a decrease in market failures (asymmetric information and incomplete information) and have reduced the average expenditure on highly complex procedures in outflow patients by 19.2% during 2012-2016 or approximately USD $ 456.9 million.
On the other hand, as show in graph 4, this dynamic has alleviated the budgetary pressure and capacity of attention of countries that send patients, with Poland and Italy being the most profitable with 11.1% and 9.6% decrease in waiting time for high complexity procedures mentioned above (De la Puente, 2015b).
The possibility that patients who have difficulties for procedures within their country of origin can move to a more accessible (mainly in the public sector) health care system has improved the quality perception of both patients and professionals involved (physicians, nurses, physiotherapists, administrative and operators).
However, the current dynamic of patient mobility also suggests difficulties in the long-term investment in high complexity clinical infrastructure, as well as lower costs of transportation and care in locations with lower prices in selected procedures. Even if data on this element are not available, it is possible to determine that since health mobility has become a viable option for European patients both internally and externally, growth in clinical infrastructure has slowed in all countries of the European Union by 5.3% (Bertinato et al. 2015).
Although the transfer of patients to other countries cannot be related to a deceleration of investment in health infrastructures, it is interesting that the correlation is inversely proportional. Medical tourism and health mobility growth represent risks and opportunities for localities where the private sector is the main player. The current market trend exposes conditions for the generation of capital gains that can be directly related to the regional situation of the medical and tourist market.
For the receiving countries, the patient's arrival represents an opportunity for expansion of the healthcare sector in the curative segment. However, there are inherent difficulties in medical travel such as organ trafficking due to sectoral deregulation, and lack of coercive capacity against populations that, not taking into account all available information, decide to sell their organs for prices that are much lower than the international average (approximately 23% lower) (De la Puente, 201a).
Another is the mobility of physicians from the public sector to the private sector due to higher income which generates a shortage of physicians and nurses. A case of great interest is the one in southern Italy where there has been a growing phenomenon of clandestine sale of organs for other EU citizens who are in waiting lists in their countries of origin with low chance of accessing these (kidney, lung, heart, are the most demanded) and opt for the clandestine purchase and transplant in authorized medical centers. This situation is even worse in non-EU poor countries where transplants are usually made in medical centers without the correct medical equipment or even clandestinely with very negative consequences for the health of both the donor and of the receiver.
CONCLUSION
Health mobility in the four segments represents the consolidation of a market with growth perspectives characterized by supply constraints for highly complex procedures. It represents an opportunity for a market consolidation for destination countries that find in the arrival of patients an additional generation of constant income where private clinics are the main agents.
Directive 883/2004 is a start for a sectoral organization in transnational health services and promotion of the protection of patients of the EU in both member and non-member countries from the generation of alliances where homologation in healthcare protocols can impulse confidence both to regional authorities and patients. Although there are no consolidated data on the health mobility dynamic, there are indicators that should be highlighted. For example, total patients' emission due to supply shortages in the country of origin, the increase in the extraterritorial healthcare insurance and the increase in legal actions of foreign patients in external healthcare system. With all of the above, there is a based study in which future research can reveal more data about the implications of intra-European regulation to health mobility beyond descriptive reports.














