Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista MVZ Córdoba
Print version ISSN 0122-0268On-line version ISSN 1909-0544
Rev.MVZ Cordoba vol.24 no.3 Córdoba Sep./Dec. 2019 Epub June 01, 2020
https://doi.org/10.21897/rmvz.1777
Editorial
Reemerging zoonoses with “One Health” approach
1 ISGlobal, Hospital Clínic - Universitat de Barcelona, Barcelona, Spain.
2 Coeditor Revista MVZ Córdoba, Universidad de Córdoba, Montería, Colombia.
3 Editor in Chief Revista MVZ Córdoba, Universidad de Córdoba, Montería, Colombia.
In 2004, the World Health Organization (WHO) defined emerging zoonoses as those “newly recognized or newly evolved, or that have occurred previously but show an increase in incidence or expansion in geographical, host or vector range” 1. Approximately 60% of infectious diseases affecting humans are of zoonotic origin 2, and vectors transmit almost 20% of all of them. It emphasizes the connection between human, animal, and environmental health, and the need to study these diseases in their biological, ecological, medical, and economic context to promote and guarantee health globally.
Emerging and reemerging zoonotic diseases might be better understood with a “One health” perspective defined by the WHO as “an approach to designing and implementing programs, policies, legislation, and research in which multiple sectors communicate and work together to achieve better public health outcomes” 3. Moreover, they highlight that “One Health” key areas correspond to three of the significant global health challenges: i. Food security, ii. Zoonoses control and iii. Antimicrobial resistance 4.
Zoonoses can be direct, when the pathogen is directly transmitted from animals to humans, or indirect when a vector is needed to carry the pathogen. These last ones, also known as vector-borne diseases (VBDs) have increasingly attracted attention due to its natural expansion, as it recently occurred in the American region during 2014 and 2015 with Chikungunya and Zika virus respectively. Emerging and reemerging zoonoses have been responsible for the significant epidemics of the last decades (Table 1). This situation has evidenced a general concern for the lack of international security to control these pathogens; and also, the unavoidable necessity to continually work in multidisciplinary teams oriented to safeguard health for all populations at a global scale.
For instance, West Nile virus was introduced to the United States in 1999. It was disseminated among North-America and later to South America, evidencing the facility of vector-borne viruses to travel among continents 5. This fact suggested the need to join international forces to combat reemerging diseases. Nevertheless, when the United Nations presented the millennium development goals, these diseases were not prioritized. Objective number 6, related to health, was centered in the two significant infectious diseases that most morbidity and mortality cause in sub-Saharan Africa: HIV/AIDS and malaria. At that time, little attention was paid to emerging zoonoses, that unfortunately have caused thousands of deaths in the last decade.
The first epidemic outbreak of the XXI century arose in 2003. Then, a coronavirus causing Severe Acute Respiratory Syndrome (SARS) was identified, with small mammals in China acting as their reservoirs 6. Speedily, it spread to 30 countries in Asia, Europe, North, and South America, causing 8439 episodes, of which 812 were lethal.
The following emerging virus appeared in 2009. The H1N1 virus caused the pandemic with the domestic pig involved. In 2012, the Middle East respiratory syndrome (MERS) emerged, from another coronavirus. It was found in camels from Saudi Arabia and spread to other Middle Eastern and Asian countries.
However, indeed, the outbreak with the most significant impact was the one occurring in West Africa from 2014 to 2016 due to the high lethality of Ebola virus (approximately 50%). It was also considered to have been the largest and most challenging outbreak to be handled since its discovery in 1976. Consequences were devastating: 28.000 infected people, 11.300 deaths, weakened health systems, and thousands of additional deaths for indirect causes due to other infections 22. Unfortunately, the international response to contain Ebola arrived uncoordinated and five months late, after multiple alarm notifications from the NGO MSF. The response was boosted by the Security Council of the United Nations after considering a threat for global security and possible spread to western countries. Even work was done to control epidemics; risk continues for millions of people from endemic areas. In 2017, a small Ebola outbreak emerged in the Democratic Republic of Congo (DRC), and another one last August 2018. Currently, the outbreak has reached Uganda with high lethality. Up to 11 of June 2019, 2084 cases have been reported 23, of which 1405 have died (67.4%), evidencing a public health problem still to be solved.
The increasing incidence of diseases spread among continents shows the necessity to address health from one perspective with global efforts in all the fields. Translational medicine tries to generate solutions from basic research to clinical research and policy-makers and vice versa.
Sustainable development goals, presented by the United Nations in 2015, showed the complexity and interconnection of health and development. Nevertheless, zoonotic diseases were not explicitly mentioned among the nine goals of health-related objective number three. As a consequence, the United Nations Development Program request actions to act in emerging priorities in global health not detailed within the objectives as mentioned earlier. It also emphasizes unequal progress achieved in the past years and the importance of using a multisectoral gender-based approach, based on rights, to diminish inequities and to guarantee good health for all.
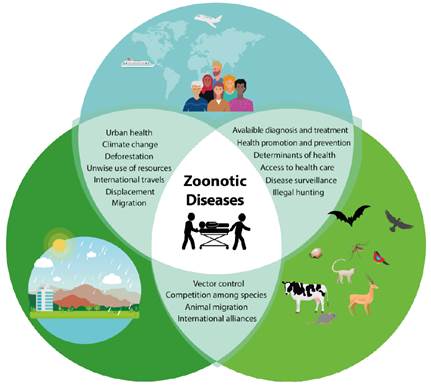
For all these reasons, “One Health” management to preserve human, animal and environmental health is a matter of priority. To address it, we need coordinated and collaborative multidisciplinary efforts (Figure 1). “One Health Global Network” emerged to join all associations and databases related to “One Health.” It has acquired a character of social movement based on collaborations among different fields, all kind of science from purely biological to social ones. International bodies are already promoting their integration in new research strategies. It is an opportunity to include groups of people from all knowledge fields to work together in the same path with the ultimate goal to understand the factors affecting the health of all living beings and to preserve it.
More than one-third of the human population lives in areas at risk of acquiring mosquito-borne diseases 24. An excellent example of them are reemerging arboviruses such as Yellow Fever, Dengue, Chikungunya, West Nile Virus, and Zika, all of them show almost a global distribution 25. To address them, we need to understand the impact of environmental determinants, social determinants of health, lifestyle, and economic determinants of affected populations. Among them, the socio-economic determinants are the ones having a significant impact on health. Mainly, gender, socio-economic status, work, education, wealth, and place of residence, among others. It was observed with the recent epidemic of Zika virus 25. People suffering the worst consequences were those living in houses and towns with least resources, less educational level, precarious working conditions, and less income; what perpetuates the already known cycle of poverty-disease. Hence, it is crucial to create multidisciplinary health research teams, including professionals in the field of medicine, veterinary, anthropology, biology, ecology, economics, psychology, among others.
From 2015, the WHO annually updates a list of infectious diseases and pathogens to be prioritized for research purposes. Currently, it includes Crimean-Congo haemorrhagic fever, Ebola virus disease, Marburg virus disease, Lassa fever, MERS, SARS, Nipah, Rift Valley fever, and in another severity level Chikungunya, severe fever with thrombocytopenia syndrome and Zika 26. On the other hand, the threat of a possible upcoming reemerging viral epidemic already exists in Colombia, now Mayaro virus is present in Peru and Ecuador 27,28, thus, the virus can be spread throughout Colombia as it happened with Chikungunya and Zika, as competent vectors are predominant in the area.
To conclude, reemerging zoonotic diseases are responsible for approximately 75% of all human infections. It is urgent to manage “One Health” approach while training students at the university level, research centers, research groups, and international bodies to achieve a real integration of multidisciplinary and multisectoral teams to control and manage zoonoses. Various groups of experts will try to predict which will be the upcoming reemerging virus to spread globally, which will be challenging due to the complexity of factors above mentioned. What is certain is that the international community must be alert to handle future epidemics, implementing lessons learned from previous outbreaks.
REFERENCES
1. WHO. Emerging zoonoses. [en linea]. World Health Organization: Geneva; 2004. [accessed 25.05.19]. URL Available in: Available in: https://www.who.int/zoonoses/emerging_zoonoses/en/ [ Links ]
2. Asokan GV, Asokan V. Bradford Hill’s criteria, emerging zoonoses, and One Health. J Epidemiol Glob Health. 2016; 6(3):125-129. https://doi.org/10.1016/j.jegh.2015.10.002 [ Links ]
3. OMS. El enfoque multisectorial de la OMS «Una salud». Organización Mundial de la Salud: Suiza; 2017. URL Disponible en: https://www.who.int/features/qa/one-health/es/ [ Links ]
4. Ryu S, Kim BI, Lim J-S, Tan CS, Chun BC. One Health Perspectives on Emerging Public Health Threats. J Prev Med Public Health. 2017; 50(6):411-414. https://dx.doi.org/10.3961%2Fjpmph.17.097 [ Links ]
5. Di Giallonardo F, Geoghegan JL, Docherty DE, McLean RG, Zody MC, Qu J, et al. Fluid Spatial Dynamics of West Nile Virus in the United States: Rapid Spread in a Permissive Host Environment. J Virol. 2016 Jan;90(2):862-72. https://jvi.asm.org/content/90/2/862 [ Links ]
6. OMS. Alerta y Respuesta Mundiales (GAR): De cómo los cuatro mayores brotes del siglo echan por tierra algunos mitos de gran arraigo. Organización Mundial de la Salud: Suiza ; 2014. https://www.who.int/csr/disease/ebola/ebola-6-months/myths/es/ [ Links ]
7. WHO. Middle East respiratory syndrome coronavirus (MERS-CoV). World Health Organization: Geneva; 2019. https://www.who.int/emergencies/mers-cov/en/ [ Links ]
8. WHO. Emergencies preparedness, response: MERS-CoV. World Health Organization: Geneva ; 2019. https://www.who.int/csr/don/archive/disease/coronavirus_infections/en/ [ Links ]
9. Chancey C, Grinev A, Volkova E, Rios M. The Global Ecology and Epidemiology of West Nile Virus. BioMed Research International. 2015; Article ID 376230. http://dx.doi.org/10.1155/2015/376230 [ Links ]
10. WHO. Emergencies preparedness, response: Severe Acute Respiratory Syndrome (SARS). World Health Organization: Geneva ; 2003. https://www.who.int/csr/sars/en/ [ Links ]
11. Zhiqi Song, Yanfeng Xu, Linlin Bao, Ling Zhang, Pin Yu, Yajin Qu, et al. From SARS to MERS, Thrusting Coronaviruses into the Spotlight. Viruses. 2019; 11(1):59; https://doi.org/10.3390/v11010059 [ Links ]
12. Cheng VC, To KK, Tse H, Hung IF, Yuen KY. Two years after pandemic influenza A/2009/H1N1: what have we learned?. Clin Microbiol Rev. 2012; 25(2):223-263. https://doi.org/10.1128/CMR.05012-11 [ Links ]
13. WHO. Emergencies preparedness, response. World Health Organization: Geneva ; 2019. https://www.who.int/csr/don/archive/year/2019/en/ [ Links ]
14. WHO. Emergencies. Chikungunya. World Health Organization: Geneva ; 2018. https://www.who.int/emergencies/diseases/chikungunya/en/ [ Links ]
15. Vu DM, Jungkind D, Desiree LaBeaud A. Chikungunya Virus. Clin Lab Med. 2017; 37(2):371-382. https://doi.org/10.1016/j.cll.2017.01.008 [ Links ]
16. WHO. Zika virus disease. World Health Organization: Geneva ; 2017. https://www.who.int/emergencies/diseases/zika/en/ [ Links ]
17. PAHO. Zika virus infection. Pan American Health Organization: Washington, D.C; 2016. https://www.paho.org/hq/index.php?option=com_topics&view=article&id=427&Itemid=41484&lang=en [ Links ]
18. WHO. Ebola virus disease. World Health Organization: Geneva ; 2019. https://www.who.int/ebola/en/ [ Links ]
19. OMS. Fiebre hemorrágica de Crimea-Congo. Organización Mundial de la Salud; Washington, D.C; 2013. https://www.who.int/es/news-room/fact-sheets/detail/crimean-congo-haemorrhagic-fever [ Links ]
20. WHO. Emergencies preparedness, response. Yellow fever. World Health Organization: Geneva ; 2019. https://www.who.int/csr/disease/yellowfev/en/ [ Links ]
21. PAHO. Yellow Fever. Pan American Health Organization: Washington, D.C ; 2016. https://www.paho.org/hq/index.php?option=com_topics&view=article&id=69&Itemid=40784&lang=en [ Links ]
22. Sarukhan A. Ébola: dos años y 11.300 muertes después: Lecciones de una epidemia para la salud global. [Accessed: 25/05/2019]. ISGlobal; 2016. https://www.isglobal.org/ebola# [ Links ]
23. WHO. Ebola Situation Report: Democratic Republic of the Congo. [Accessed 13 June 2019]. World Health Organization: Geneva ; 2019. https://www.who.int/ebola/situation-reports/drc-2018/en/ [ Links ]
24. Liu LE, Dehning M, Phipps A, Swienton RE, Harris CA, Klein KR. Clinical Update on Dengue, Chikungunya, and Zika: What We Know at the Time of Article Submission. Disaster Med Public Health Prep. 2017 Jun;11(3):290-9. https://doi.org/10.1017/dmp.2016.144 [ Links ]
25. Gould E, Pettersson J, Higgs S, Charrel R, de Lamballerie X. Emerging arboviruses: Why today? One Heal. 2017; 4:1-13. https://dx.doi.org/10.1016%2Fj.onehlt.2017.06.001 [ Links ]
26. WHO. WHO publishes list of top emerging diseases likely to cause major epidemics. [Accessed 13 June 2019]. World Health Organization: Geneva ; 2015. https://www.who.int/medicines/ebola-treatment/WHO-list-of-top-emerging-diseases/en/ [ Links ]
27. Mattar VS, González TM. Mayaro and Chikungunya; two alphaviruses with clinical and epidemiological similarities. Rev MVZ Córdoba. 2015; 20:4861-4863. https://doi.org/10.21897/rmvz.1 [ Links ]
28. OPS, OMS. Alerta Epidemiológica: Fiebre de Mayaro. 1 de mayo de 2019. Organización Panamericana de la Salud / Organización Mundial de la Salud; Washington, D.C; 2019. https://www.paho.org/hq/index.php?option=com_docman&view=download&category_slug=fiebre-mayaro-2322&alias=48377-1-de-mayo-de-2019-fiebre-de-mayaro-alerta-epidemiologica-1&Itemid=270&lang=es [ Links ]
How to cite (Vancouver) Marbán-Castro E, Mattar S, González TM. Reemerging zoonoses with “One Health” approach. Rev MVZ Cordoba. 2019; 24(3):7280-7284. DOI: https://doi.org/10.21897/rmvz.1777











 text in
text in