Introduction
Sodium Fluoroacetate poisoning poses a diagnostic challenge for healthcare personnel caring for patients with signs and symptoms secondary to toxicity from this compound. Despite being a prohibited substance in Colombia, it is widely used for rodenticidal purposes in the country. There are few reviews on the subject, so it is necessary to know fundamental aspects of the substance, mechanism of action, determination methods in the clinical laboratory, and management of these patients 1.
Case report
A 14-year-old patient with no significant personal or family history was admitted into the emergency department. The patient was referred from the local unit because of the clinical condition of seven hours of evolution consisting of voluntary intake of sodium fluoroacetate for suicidal purposes. In the first level of attention, gastric lavage and oral doses of activated carbon were administered; It evolved inadequately with increased dyspnea and desaturation; given this, the patient is transferred to the third level of care.
The patient entered the third level of attention in quite feeble general conditions, desaturated, sialorrhea, and with a Glasgow coma scale of eight, fasciculations, and hypotension. It was decided to secure the airway to avoid the risk of the patient's bronchoaspiration and the alteration of the state of consciousness. Treatment with ethanol, calcium gluconate was started on the patient and transferred to the ICU.
Upon admission to the intensive care unit, the patient with unfavorable conditions presented Blood Pressure: 69/40 mmHg, Average Blood Pressure: 50 mmHg, Heart Rate: 116 per minute, Temperature: 36 °C, diaphoretic; thus, vasopressor support with Norepinephrine was started although the blood pressure goals were not achieved. In view of this, the patient required vasopressin to reach the goal during the first 24 hours of evolution. Mechanical ventilation assisted mode volume control, PEEP 6 FIO2 100%, glucometry: 137 mg/dL. Physical examinations showed hypochromic conjunctiva, normoreactive isocoric pupils, dry oral mucosa, mobile neck, thorax: rhythmic heart sounds without murmurs, tachycardia, decreased vesicular murmur in both fields with bibal crepitus, depressible soft pain without peritoneal irritation, extremities without edema, capillary refill in four seconds neurological RASS -5
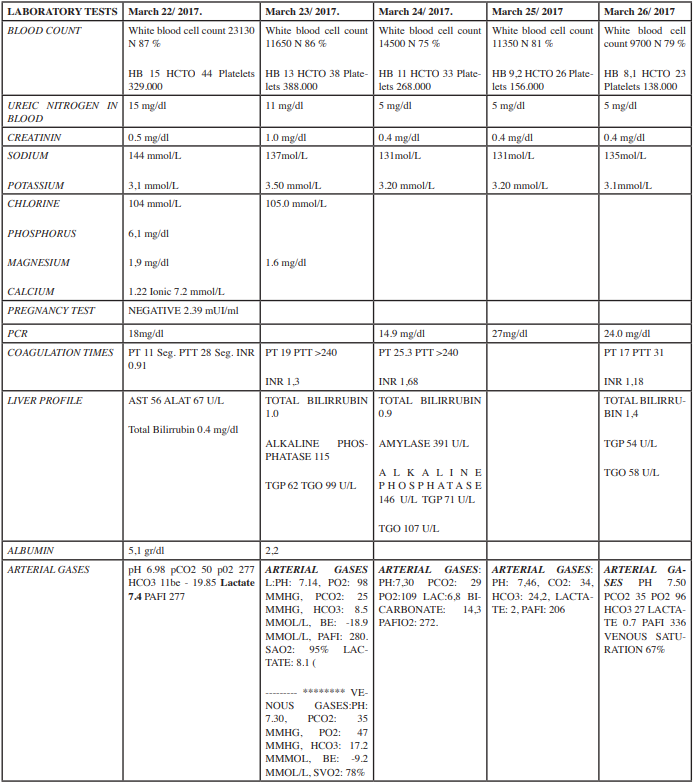
The patient behaved anuric during the first 12 hours of the stay in the ICU, with levels of nitrogen containing compounds within normal limits, with persistent hyperlactatemia metabolic acidosis, multifactorial, secondary to intoxication per se. The use of ethanol was established as medical management; kidney injury rapidly progressed to KDIGO III acute kidney injury, the reason why it was decided to start renal replacement therapy with continuous venovenous hemodiafiltration. In the Table 1 you can see the laboratory report:
As a management protocol was established with a dose of ethanol of 0.1 gr / kg, / hour, calcium infusion of 3 mg / k / h, hydric resuscitation, and vasoactive support for a target of mean arterial pressure greater than 65 mph in relation with distributional shock. The patient presented clinical evolution towards improvement after 72 hours of renal replacement therapy in terms of diuresis parameters and the resolution of metabolic acidosis with lactate clearance to normal levels; in view of this, the renal replacement therapy was discontinued. Clinically, vasoactive supports were withdrawn at the same time of evolution and towards the seven day of the patients’ hospital stay, attempts were made to release mechanical ventilation, without any success. Synchronously, there were found febrile episodes and microbiological reports of staphylococcus aureus growth which was attributed to a pneumonic process that was covered with an antibiotic scheme treatment. After 10 days of management, the patient was discharged from the intensive care unit with a satisfactory evolution.
Discussion
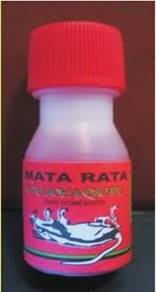
The sodium fluoroacetate is known in Colombia as “Guayaquil” liquid , you can see it in Figure 1:
In the United States, it is known as compound 1080. This poison was developed in 1940 by Marais when observing the effects that it produced in the goats such as the paralysis of the animal's posterior; consequently, it was called the "rear bankruptcy". It was later used as a rodenticide that was considered one of the most toxic substances in the world 1, its distribution and use in Colombia is prohibited 2.
The sodium fluoroacetate is a substance widely used in Colombia as a rodenticide and in some cases also as a way of committing suicide. In its 100% pure form it is a white powder that, when dissolved in water, forms an odorless, colorless and tasteless solution, it is generally found on the market mixed with a blue dye to differentiate it from other substances. The lethal dose for humans is between 2 and 10 mg / kg. Due to its illegality, the concentrations in commercial products are irregular and therefore it is very difficult to determine the exact dose that the intoxicated people ingested. It is a fat-soluble substance with good oral absorption and with rapid distribution to the tissues after ingestion. The highest concentrations are found in plasma followed by kidney and muscle and the lowest concentration in the liver 3.
After the intake of the sodium fluoroacetate, it requires the metabolic conversion of fluoroacetate to fluorocitrate, obtaining increased levels thirty minutes after the ingestion of it, and with a maximum peak at four or six hours, and returning to basal concentrations at 40 hours. Its excretion is renal and takes between one and four days.
Sir John Peters in 1963 described the main effect of the sodium fluoroacetate consisting of ATP depletion, by inhibition of the tricarboxylic acid cycle or Krebs cycle (KC) 4. Sodium fluoroacetate reacts with the enzyme citrate synthase to form monofluoroacetate instead of citrate, a substance that is not a useful substrate for the enzyme aconitase in the Krebs cycle and therefore blocks it. The reduction in the oxidative metabolism contributes to lactic acidosis, which added to the accumulation of ketone bodies and the non-oxidation of fatty acids, brings an increase in acidosis 1. Despite its high metabolism, it accumulates less citrate and frequently affects the brain, heart, kidney, spleen, and liver.
The accumulation of citrate generates an electrolyte and acid-base imbalance, which leads to metabolic acidosis. The accumulation of lactate and cerebral citrate has been considered a cause of coma and seizure in the patient poisoned by fluoroacetate. Hypocalcemia is related to the chelating effect of fluorine, citrate, and fluoroacetate ions on calcium 1.
Initially, most patients are asymptomatic, but in a few hours they will present nausea, vomiting, sialorrhea, mydriasis, and electrolyte imbalances (especially hypocalcemia due to the chelating properties of calcium in sodium fluoroacetate), as occurred in the clinical case described. Central nervous system compromise occurs frequently as a diverse manifestation from drowsiness, vertigo, fasciculations, tremor, seizures and respiratory failure of central origin as occurred in this case. However, the cause of respiratory failure due to community-acquired pneumonia or initial shock is not ruled out. At the cardiovascular level, it was manifested in the patient with arrhythmias, prolongation of the QTc segment and less frequently myocarditis 5,6 hypotension that could be due to the blockage of the tricarboxylic acid cycle, and acidosis in the vascular epithelium. Death is generally caused by cardiopulmonary abnormalities. The diagnosis is made based on a clinical history that confirms the ingestion of substances containing sodium fluoroacetate and the presence of symptoms and signs described by various authors for this toxicosis 2,7,8.
Treatment
In the case of sodium fluoroacetate poisoning, the initial approach should be carried out as in all intoxicated patients; it is essential to take into account the initial ABCD, determining the need to obtain a definitive airway, correcting hemodynamic instability, and determining the oxygen and glucose supply of these patients 9. Management of support and correction of hypokalemia is essential. Different antidotes have been studied; however, the progress in humans is limited 10,13. The management of seizures should be done with benzodiazepines, of which diazepam is the most recommended. In the case that the crisis does not stop, barbiturates such as thiopental should be used, which would additionally act as a brain protector, reducing the risk of cerebral edema and local ischemia 3. In the initial decontamination, the removal of contaminated clothing and external washing with soap and water is essential, as well as gastric lavage if the patient is admitted with less than one hour of oral exposure. Activated carbon has been shown to adsorb fluoroacetate; nonetheless, there is no data on the impact of the clinical outcome of these patients. Hemodynamic management should be performed with intravenous fluids, followed by vasopressors (norepinephrine) in cases where hypotension is not treated. The presence of hypotension, acidemia, and creatinine elevation is correlated with high mortality; therefore, these disorders must be managed promptly 14,15. The most important electrolyte disorder is hypocalcaemia, which must be properly determined and treated in these patients. Improvement in survival has been found in animals when calcium chloride supplements are administered, although the results are not conclusive. Calcium has been reported to be useful in improving muscular activity (tetanic convulsive movements) and in cardiac arrhythmias 11.
Antidotes
The use of antidotes in sodium fluoroacetate poisoning is based on the need to prevent the production of fluorocitrate and inhibition of aconitase while achieving mitochondrial citrate output. In this order of ideas, acetate donors such as ethanol and glycerol monoacetate are the most widely used antidotes in the management of this poisoning. Ethanol has shown the best results and is the most used, its oxidation produces elevation of acetate levels, which competes in the formation of fluorocitrate 1,(16),3,9.
Several protocols have been proposed for the management with ethanol, it has been described that after the acute administration of fluoroacetate, 40 - 60 cc of 96% ethanol should be administered, followed by 1.0 - 1.5 g / kg of ethanol 5-10% intravenous in the first hour and subsequently 0.1 g / kg every hour for 6 - 8 hours 3. The exact dose of ethanol has not been determined, the most logical possibility is to achieve a serum ethanol concentration of 100 mg / dl, administering the same doses used in ethylene glycol and methanol poisoning 8.
Ethanol does not only block the production of fluorocitrate, but also decreases hyperglycemia and increases GABA levels in the central nervous system 3. In animal studies, the best results in methanol management are obtained after 10 min of fluoroacetate poisoning 7. Glycerol monoacetate and acetamide have been proposed as antidotes, animal studies that have been developed demonstrate the effectiveness in decreasing ketone body levels, decreasing citrate in the brain, kidney and heart, and improving neurological and cardiac effects. However, in humans an increase in hyperglycemia, worsening of metabolic acidosis, damage to capillaries and erythrocyte hemolysis are noted. Therefore, some reviews do not recommend the use of glycerol monoacetate or acetamide in the management of fluoroacetate poisoning in humans 3.
Other antidotes have been tried to develop in order to produce energy by supplying intermediates of the tricarboxylic acid cycle while blocking the production of fluorocitrate. The use of calcium salts (calcium gluconate), sodium succinate, and α-ketoglutarate have been evaluated, which have shown benefit as long as calcium is administered simultaneously, which shows the importance of stabilization of hypocalcemia in these patients 3,11. The most effective regimen appears when administering 240 mg / kg sodium succinate and 130 mg / kg calcium gluconate fifteen minutes after administration of fluoroacetate 7,16.
Renal replacement therapy
There are three techniques for eliminating toxins: hemodialysis, hemofiltration, and hemoperfusion 17,18. Nevertheless, hemodialysis is the most adequate to eliminate low molecular weight and water-soluble toxins, which was used to treat this patient. Given the persistence of symptoms such as anuria for 12 hours, severe metabolic acidosis that was associated with the ingestion of the poison, a timely initiation of renal replacement therapy was decided 18,19. The decision to start this therapy to treat the acute kidney injury and the presence of intoxication with severe clinical manifestations of the toxin was made due to the unavailability of a specific antidote and its specification of the renal route; additionally for the anuric condition of the patient that would have perpetuated the symptoms of poisoning.
Conclusions
Sodium fluoroacetate poisoning is relatively rare and can cause acute kidney injury and multi-organ failure with a high rate of complications and death. A case of self-inflicted poisoning that received early continuous renal replacement therapy with a favorable outcome in terms of ICU survival was presented. The favorable outcome of the patient was possible in view of the low dose of the toxin, to the implementation of initial decontamination measures, and to a timely management in the intensive care unit with renal replacement therapy. Long-term clinical outcomes are unknown since there was not a follow-up to this case.