Introduction
The cardiac ultrasonography is a basic imaging exam, which is useful for evaluating cardiac patients who come to the ER. This exam is advantageous for showing the condition of the hemodynamic status or the presence of any cardiac lesions. All of them could be performed in real time to get information for the prognosis and follow-up procedures. In Colombia, it is believed that the ultrasonography is an exclusive tool for the radiologist or other specialists; therefore, general practitioners have been unable to interpret it. However, in the ER of developed countries, this tool has surpassed the stethoscope and also played a crucial role in medical student education.
From 2015 to 2018 the prevalence of risk factors of suffering from cardiovascular disease was 49.2% in adults over 20 years old. Then, the highest cause of death by cardiovascular disease was the Coronary Artery Disease with an incidence of 42.1%, followed by the Stroke with 17.0%, and Heart Failure with 9.6%. Among the Hispanics in the United States, Cardiovascular Disease was the first cause of death in nearly 30% of males and females 1.
In Colombia, according to the National Institute of Health, heart diseases were the first cause of mortality until 2015, with ischemic coronary disease as the first cause with 41.8% 2. Besides, at least 10% of the thoracic trauma is associated with the cardiac trauma 3, and its mortality is estimated around 76% 4. The reason for this variability of the rate could be that the patients coming to ER cannot know the specific state of the damage to the heart.
The importance of knowing the myocardial function could help the physician to make a correct management, and reduce the high mortality presented due to conditions such as pericardial tamponade, dysfunction of the cardiac wall motion, and hypovolemia. Furthermore, the European Resuscitation Council (ERC) guidelines for resuscitation 2005, recommended the intermittent application of cardiac evaluation by ultrasonography during the cardiopulmonary arrest (CPA). The recognition of the causes of CPA and the quick resolution actions of these lead to a better result of return of spontaneous circulation 5)(6. For all hemodynamically critical patients, transthoracic echocardiogram (TTE) can identify the causes of shock, and those key findings often change the treatment to be followed 7)(8.
To conduct TTE screening, it is not necessary for general doctors to have the same training as sonographers 9. General practitioners need to complete a couple of required techniques and receive eye training to decide to treat the patients. In developed countries, the medical students already have close contact with the ultrasonography. However, in this country where the health system is poor, they do not have enough budget and opportunity to receive the training.
In this review, we will describe the minimal technique to get proper images of TTE and the way to analyze obtained data to make proper decisions in ER.
1.Clinical Application
a. Thoracic Trauma
The objective of using ultrasonography is to determine the presence of an active bleeding in pericardial space after trauma. It will be seen as pericardial effusion, but such effusion does not imply to be cardiac tamponade. The cardiac tamponade is a status in which the abnormality of blood or other fluid circulation is determined. The pericardial effusion that follows the rupture of the myocardial muscle will disturb the dilatation of the wall motion, resulting in the deterioration of vital signs.
b. Cardio-Pulmonary Arrest (CPA)
The ultrasonography in CPA is so useful that it can change the prognosis of victims. It can show the situation of the heart in real time, evaluate intravascular volume, and find the etiology of the CPA. Based on all this data, the life support team can effectuate a better job.
c. Hypovolemic Shock
Cardiac ultrasonography can help the case of unknown hypotension on critical scenes, mainly by evaluating if the hypotension is caused by cardiogenic shock or not. In addition, it can repeatedly evaluate the levels of severity.
d. Chest Pain
Doctors at ER often consult patients with chest pain. Here, the performance of ultrasonography is not only to evaluate the heart function since it has an essential role in detecting the presence of high mortality diseases such as aortic dissection or pulmonary embolism. If doctors do not find any severe etiologies, they will start to perform routine cardiac screening in detail.
2. Technique
Doctors should choose TTE as a part of the cardiac evaluation at ER as well as knowing medical history and conducting other physical and laboratory exams. There are three points to check: global wall motion, the size of the cardiac chambers and the presence of pericardial effusion. TTE has many windows, but the basic ones are the long axis (LAX), short axis (SAX), four chamber (4Ch), and subxiphoid acoustic window. Finally, it is also necessary for doctors to understand the anatomical position of the heart.
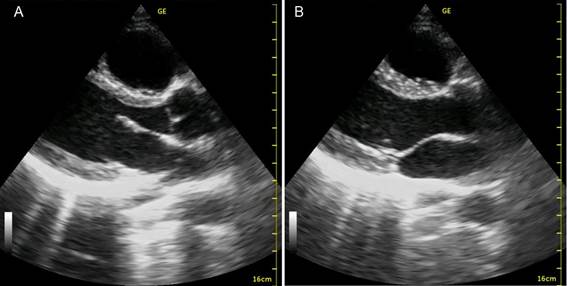
a. Long axis view (LAX)
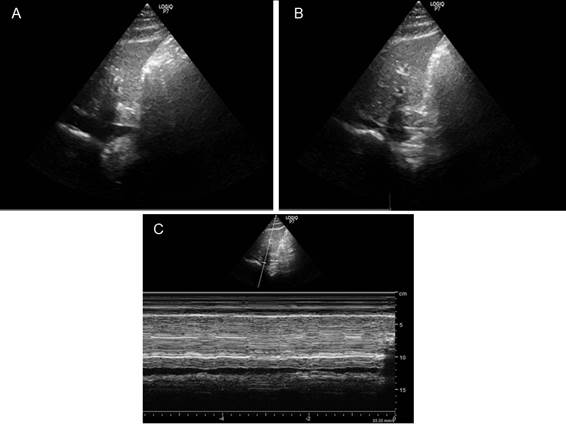
This window is between the 3rd to 5th intercostal space with the left parasternal line. The marker of the transducer will be pointed at 10 o’clock or the right shoulder. Examiners can observe the right ventricle, the aorta, and the left atrium and ventricle. At the same time, they can evaluate the wall motion, chamber sizes and presence of pericardial effusion. The chambers can be measured with the measuring tool in the machine, but they must not spend a long time in an emergency. In this view, the left ventricle should not be bigger than the right ventricle. (Figure 1.)
b. Short axis view (SAX)
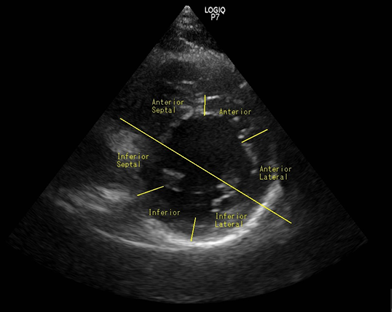
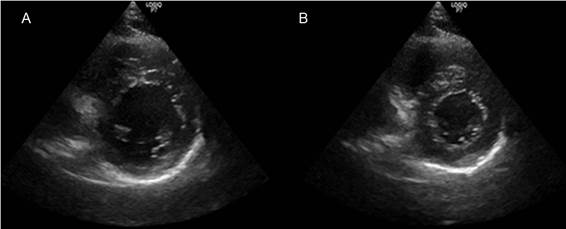
The second window is SAX. From LAX, the examiners rotate the probe at 90 degrees in a clockwise direction at the same parasternal point. From this view, they can see both the ventricles at the transverse plane. The left ventricle appears as a circle while the right ventricle seems as a crescent moon. The key point of this view is to evaluate at the level of papillary muscles since examiners can get a clear image for the evaluation of wall motion. Based on that, it is important to comprehend the orientation of the heart, and to know which wall portion is damaged. (Figure 2. And Figure 3.)
The evaluation points are the same as in LAX: the wall motion, chamber sizes, and presence of pericardial effusion.
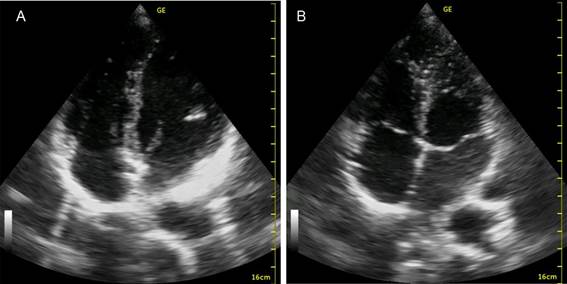
c. Apical 4 chamber
The third window is the apical 4 chamber. Here, the examiners will approach the probe from the sixth intercostal space in the left axillary line. The image shows the apex at the top of the screen, including the whole heart with its 4 chambers. The ventricles appear on the upper side of the screen and the left heart will be seen at the right side of the screen. The crucial structure in this view is the moderator band inside the right ventricle. It is important to confirm the laterality of the heart too. The main points are the same as LAX and SAX: wall motion, chamber sizes and presence of pericardial effusion. In suspected cases of intraventricular thrombus, this view can identify it especially at apical portion. (Figure 4.)
d. Subxiphoid view
Ultrasonography at cardiac arrest situations can improve the result in the return of spontaneous circulation (ROSC). Using that, the life support provider has more available information for making a decision 10. Although the approach should be performed from the epigastric window, the evaluation during cardiac arrest is not easy. When using subxiphoid view, examiners do not interfere with the chest space for chest compression. This view is the same as the four chambers' and the evaluation points are the same as in the other views: wall motion, chamber sizes and presence of pericardial effusion. Needless to say, to rule out the treatable causes of CPA is the most important aspect.
e. Inferior Vena Cava (IVC)
The approach to the IVC is made through the same window of subxiphoid view. Examiners should rotate the probe to the sagittal plane. If there is no appearance of IVC, they tilt the probe to the left side in many cases. In this window, it is important to show the right atrium continuing to the IVC. The examiners ask the patient to inspire deeply to obtain a proper image. The IVC view is useful to indirectly evaluate the volume condition. If IVC collapses to the half in the beginning, it means a normal intravascular volume. If the IVC collapses completely or maintains expanded during the inspiration, it could alert a volume alteration and the physician should reconsider the fluid therapy. (Figure 5.)
Key sentence
Ultrasonography is a modern and indispensable tool for physicians who work in the emergency room or manage critical care patients.
TTE should be used to determine etiologies and evaluate the prognosis in any critical care scenes.
The emergency ultrasonography should be performed for future medical treatments for a short time. Physicians never take a long time to perform ultrasonography for the diagnosis.
General practitioners at ER need to complete a couple of required techniques of TTE and receive eye training for hours. The TTE is not for specialists but general practitioners.