1. Introduction
Chronic noncommunicable diseases such as type 2 diabetes mellitus 1, systemic arterial hypertension 2, and dyslipidemias 3 are now a major health problem, due not only to the financial burden of treatment, but also to the high cost of polypharmacy. Several drug interactions associated with polypharmacy, self-medication, and a lack of drug surveillance make chronic-degenerative disease management a challenge for any health institution, especially primary care physicians. In the elderly, there are many conditions that require multiple medications, self-medication, inappropriate prescriptions, and visits to multiple specialists, which all contribute to polymedicated patients 4)(5.
The first studies carried out on polypharmacy focused on the simultaneous use of two, three or four drugs, for the year 1997 minor polypharmacy was defined as the use of 2 to 4 drugs and more than 5 as polypharmacy, this in turn had modifications later, until defined as 4:
Between zero and 5 drugs as no polypharmacy.
Between 5 to 10 as polypharmacy.
More than 10 as excessive polypharmacy.
Currently, the World Health Organization (WHO) defines it as the concomitant consumption of three drugs simultaneously, classifying it as lower when two to four drugs are consumed and higher when there are more than five 6)(7.
Studies carried out in 2017 mention that polypharmacy is the daily consumption of three or more medications, either for the same pathology or added in the same patient in a minimum time of 60 days to less than 240 days 8)(9.
The term polypharmacy only means "many medications" and is defined as present when a patient takes two or more medications 10. The most updated studies in 2019 determined that polypharmacy is the consumption of 5 or more drugs and hyperpolypharmacy is the use of 10 or more drugs. 11)(12.
In chronic degenerative diseases, polypharmacy is related to age. Approximately 40% of adults 65 and older use five or more medications, and 12% use ten or more medications 13.
Medication errors generate drug interactions, adverse reactions and a poor quality of life. Drug-drug interaction increases exponentially with polypharmacy, so for 5 drugs there are 10 possible interactions, for 10 drugs there are 45 possible interactions and for 15 drugs there are almost 105 possible interactions 4.
It was observed that polypharmacy due to the physiological, psychological and social changes experienced by older adults in the Urban Health Center of Juan Aldama, Zacatecas, México 8, the geriatric population is more sensitive, and the predominant sex was female and the age group between 60 and 77 years 8 60-69 years 14. In major adult patients the most predominant disease was arterial hypertension followed by diabetes mellitus 14. Polypharmacy occurred in approximately one of every three older adults in the National Health Survey of Spain. The magnitude of polypharmacy in older adults is considerable and a growing practice over time. It is necessary to know this practice in greater depth, identifying those older adults with a high risk of consuming multiple drugs simultaneously 15.
On a global scale, polypharmacy is a major problem that affects mainly the first level of medical care, it has caused high drug costs because patients do not adhere to treatment, as well as the drug interactions that occur. Furthermore, there is a high prevalence of chronic-degenerative diseases in our country; 12 million people have diabetes, 22.4 million people have hypertension, 2.63 million people have dyslipidemia, these diseases are common in the Huajoyuca de Palacios Center for Health. Also, there are no reports on how many patients with chronic degenerative diseases may take more than three medications, resulting in the lack of effectiveness of treatment.
Objective
The main purpose of this work was to address the issue of polypharmacy in patients with chronic-degenerative diseases aged 50-90 years at the Huajoyuca de Palacios Health Center since June 2018 to June 2019, and it represents the first polypharmacy study conducted in a highly marginalized community with chronic-degenerative patients.
2. Material and methods
The following research work was descriptive, observational, non-experimental, statistical, with a review of existing documents, retrospective, cross-sectional, homodemic, uni-centric; this was made in a public health center of Huajoyuca de Palacios, Tepexi de Rodríguez Puebla, from June 2018-June 2019.
The sample was non-probabilistic, patients with chronic degenerative diseases with an intake of> 3 drugs per day were selected. The selected sample consisted of 56 clinical files according to the inclusion criteria.
Descriptive statistics, frequency histograms, tables and measures of central tendency were used in the Microsoft Excel® program ver. 2010. The results are presented as the mean ± SD with a 95% confidence interval.
3. Results
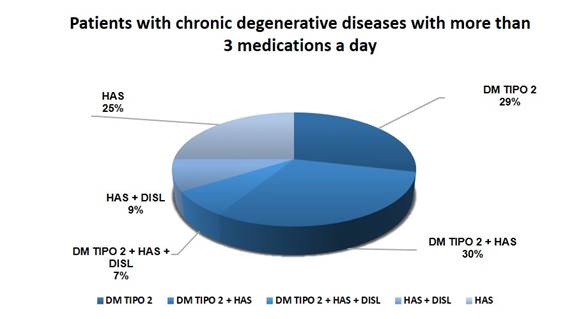
This study examined 56 clinical records of patients with chronic-degenerative diseases at the Huajoyuca de Palacios Health Center with an average age of 67.11 ± 9.6 years. Figure 1 shows a selection of patients with chronic degenerative conditions who were prescribed over three drugs per day. Among patients with chronic-degenerative diseases, the most common pathologies were Type 2 Diabetes Mellitus + Arterial Hypertension, followed by Type 2 Diabetes Mellitus, then Systemic Arterial Hypertension, and at the end there were more than one comorbidity, indicating that the medication is increasing as comorbidities appear. Figure 1
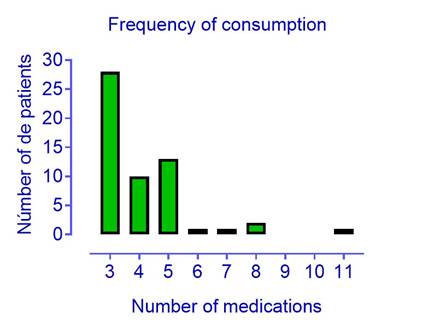
In other hand, figure 2 illustrates how often drugs are consumed in general. There are 56 patients, 28 of whom consume 3 medications per day, 10 take 4 medications, 1 takes 6 medications, 1 takes 7 medications, 2 take 8 medications, only one takes 10 medications. Based on the review of clinical records, the results show that three drugs are consumed more frequently, however, 11 drugs were found consumed by one patient.
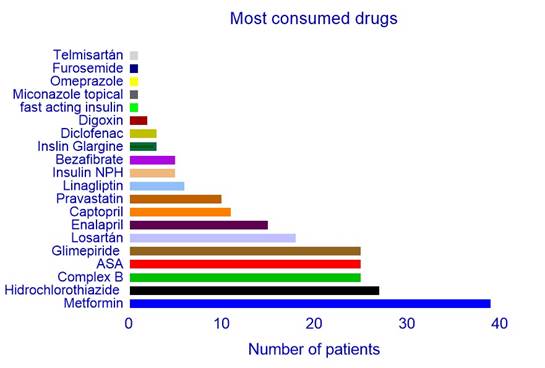
Regarding the treatment frequently used by patients with chronic degenerative diseases such as Type 2 Diabetes Mellitus, Systemic Arterial Hypertension and Dyslipidemia, are summarized inFigure 3. The graphs present frequency of use as follows metformin (17.41%), hydrochlorothiazide (12.05%), B vitamin (complex B), acetyl salicylic acid, glibenclamide with (11.16%), losartan (8.03%), enalapril (6.69%), captopril (4.91%), pravastatin (4.46%), linagliptin (2.67%), NPH insulin and bezafibrate with (2.23%), Insulin glargine and diclofenac with (1.33%), digoxin (0.89%), rapid-acting insulin, topical miconazole, omeprazole, furosemide and telmisartan with the (0.44%) are the most consumed.
(The graph shows the drugs with the highest consumption, we observe that metformin is in first place, hydrochlorothiazide in second place and in black, B complex in green, acetylsalicylic, in red, glimepiride in coffee, losartan in lilac, enalapril in purple, captopril in orange, pravastatin in mustard, linagliptin in color light blue. Those drugs with less consumption are telmisartan in gray, in royal blue furosemide, yellow omeprazole gray topical miconazole, green rapid-acting insulin.
Minor polypharmacy was observed in 38 patients with 68%, major polypharmacy was observed in 17 patients with 30%, and excessive polypharmacy was observed in 1 patient with 2% overall as presented in Fig. 4.
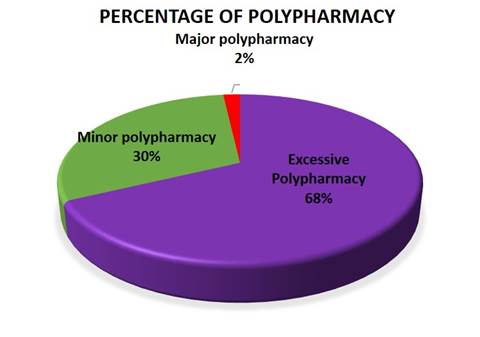
Figure 4 Classification of minor, major and excess polypharmacy in patients with chronic degenerative diseases.
((The polypharmacy is observed in purple in purple with 68%, in orange the higher polypharmacy with 30% and in red the excessive polypharmacy with 2%.
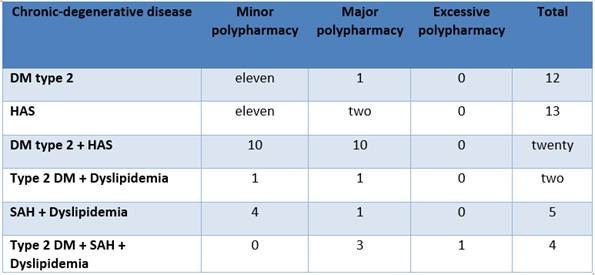
Table 1 indicates the patients for each disease and the presence of polypharmacy, so that patients with 2 or more comorbidities tend to consume more drugs, thus increasing polypharmacy. It was observed that patients with type 2 DM, with SAH and type 2 + SAH are the most affected with minor and major polypharmacy, however it is observed that there is a patient with the 3 comorbidities that has generated excessive polypharmacy.
Table 1. Classification as minor, major, and excessive polypharmacy of patients with type 2 diabetes mellitus, systemic arterial hypertension, and dyslipidemia.
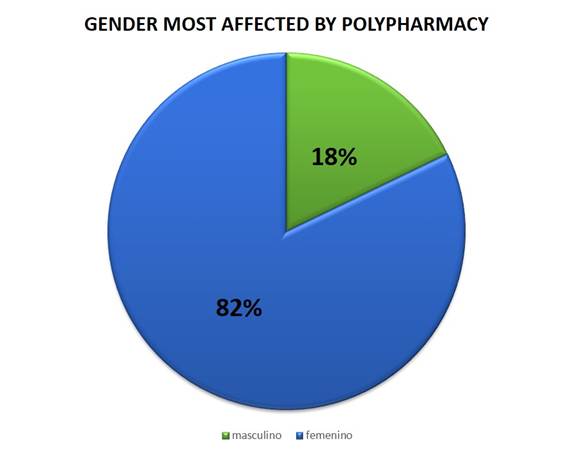
The female gender is the most affected by chronic degenerative diseases and excessive medication use, within 46 women representing (82%), followed by 10 men representing (18%), these data can be seen in Fig. 5
Our data provides information that the prevalence of minor polypharmacy occurred in patients with type 2 DM, type 2 DM + SAH representing the female gender, and patients with SAH + Dyslipidemia represented by men, in the major polypharmacy patients with type 2 DM + SAH represented by women and patients with type 2 DM + SAH + Dyslipidemia represented by men and excessive polypharmacy occurred in a single patient with type 2 DM + SAH + Dyslipidemia, as listed in Table 2.
Table 2. Minor, major, and excessive polypharmacy according to gender in patients with degenerative chronic - disease.
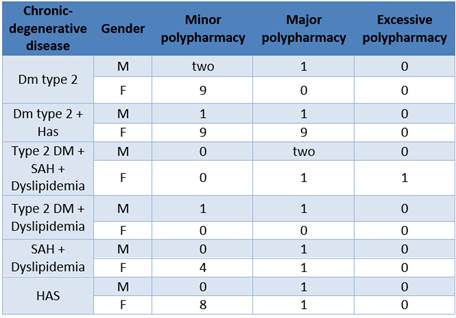
((((The table shows by disease age and with the highest prevalence of polypharmacy in patients those with type 2 DM + Has, SAH, type 2 DM with a higher prevalence in polypharmacy, but patients with more comorbidities, only 1 patient was observed with excessive polypharmacy with type 2 DM + SAH + Dyslipidemia.
The table 3, shows that minor polypharmacy was present in the age range of 70-79 years, however, major polypharmacy was present in patients 60-69 years old and excessive polypharmacy was present in a 50-year-old patient.
Table 3 Polypharmacy by age range
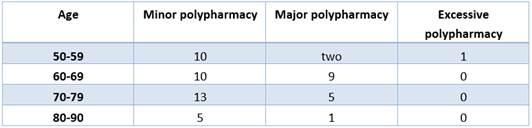
(((((It was observed that in aged 50-59 we have 10 patients with minor polypharmacy, 2 with polypharmacy, major and 1 patient with excessive polypharmacy, aged 60-69 10 patients with minor polypharmacy and 9 with Polypharmacy major, aged 70-79 years 13 patients with polypharmacy minor and 5 with polypharmacy major and aged 80-90 years, 5 with polypharmacy minor and 1 with polypharmacy major.
Discussion
The prevalence of polypharmacy is higher in patients with chronic-degenerative disorders than in others, this is demonstrated in countries like Spain, Cuba even in México; however in the remote communities, no in-depth studies have been performed, such is the case of the Huajoyuca de Palacios de Tepexi de Rodríguez Health Center, Puebla, in this study, we determined the existence of Polypharmacy in patients with chronic degenerative diseases, Systemic Arterial Hypertension (SAH), Type 2 Diabetes Mellitus (DM2) and Dyslipidemia.
Aging is a stage of life since of the biological process that generates changes in the body, thus increasing the severity of each of the chronic-degenerative diseases 18)(19. It was found that the average age of older adults is 67.11 ± 9.6 years, as described before. It is evident that the results obtained here are in exceptionally good agreement with the reported in other investigations 6)(8)(14)(20. In addition chronic degenerative non-communicable diseases are a heterogeneous group of diseases that contribute to mortality; nationwide, there are 12 million people with type 2 diabetes mellitus, 22.4 million people with high blood pressure, it is estimated that 2.63 million people have dyslipidemia 21, this as consequence of a deterioration in the physiological and biological process, increased health problems, as a result of environmental, demographic, economic, socio-cultural changes, lifestyle, genetic factors and the presence of some diseases 19)(13, our results provide compelling evidence for the predominant chronic-degenerative diseases are: Type 2 Diabetes Mellitus + Arterial Hypertension in first place, in second place Type 2 Diabetes Mellitus, in third place Systemic Arterial Hypertension, in fourth place Systemic Arterial Hypertension + Dyslipidemia and the last. Type 2 Diabetes Mellitus + Systemic Arterial Hypertension + Dyslipidemia, as can be seen in figure 1, these results correlate well with some others like the García Chairez, et al. 8, who reported the most predominant diseases are arterial hypertension, diabetes mellitus and dyslipidemia.
Most notably, this is the first study to our knowledge to investigate the number of drugs consumed in this population, it was observed that the number of drugs consumed is from 3 to a maximum of 11, (see figure 2), is in line with Robles et al. 6 and García Chairez et al. 8, who reported an average of 4 ± 3 medications. In their research work, they observed that there are some cases with consumption of up to 10 medications a day. Older adults are the main population and age group in having excessive consumption of various medications, some of the reasons are because they suffer from various pathologies, due to self-medication and due to receiving inappropriate treatment.
Administering the best possible therapy is a great obligation of each of the physicians, however, this entails the prescription of a high number of drugs. As described by Wallece et al. 21, drug interactions are frequently increased in older people due to decreased metabolism and incorrect drug elimination. The patients can easily administer the drugs together, but drug interactions can occur which are unknown to them and even to health care professionals, which can lead to severe complications of chronic degenerative diseases. The risk-benefit is the balance of the various treatments, including the option of not using any pharmacological treatment and trying to keep patients under control with first-choice prevention measures like monitoring capillary glycemia, taking care of the consumption of foods rich in sugars, fats, salts, carbohydrates, performing physical activity at least 30 minutes every third day, teaching the patients as well as they learn to eat properly.
The pathophysiological changes in older adults cause the mechanisms of action of each drug to be affected and at the same time cause problems for the patient: such as inadequate control of blood glucose, abnormal parameters in blood pressure and in blood fat levels due to changes in the systems 22)(23, at the endocrine system patients experience a decrease in insulin secretion and insulin sensitivity, leading to decreased tolerance and resistance to glucose; complicating the management of type 2 diabetes mellitus.
Older people commonly have cardiovascular diseases and require medications for this organ system, mainly those who have systemic arterial hypertension; therefore, they have decreased cardiac reserve, increased blood pressure partly due to the decrease in the vasculature, the loss of myocardial contractility in general, decreased vagal tone and left ventricular hypertrophy, decreasing sensitivity to catecholamines. In the urinary system the kidneys are the main means for the elimination of drugs, with age, the renal mass decreases and the glomerular filtration rate decreases for several reasons including decreased blood flow, decreased vascular compliance and decreased mass. muscle that complicates the assessment of kidney function, since serum creatinine cannot be as reliable a measure of kidney dysfunction, as it reflects muscle mass, which is often decreased in older patients. It seems paradoxical that in order to achieve adequate control of blood glucose levels, blood pressure, and body fat, multiple medications are sometimes needed, thus increasing the consequences of polypharmacy such as: risk of adverse drug reactions in the elderly patients 19)(23 because they are more susceptible to disorders caused such as: hypoglycemia, arterial hypotension, kidney failure, fluid and electrolyte disorders, over anticoagulation, falls, fractures, confusion and cognitive impairment.
Conclusion
Patients with chronic degenerative diseases at the Huajoyuca de Palacios Health Center present minor, major, and excessive polypharmacy. Patients with chronic degenerative diseases at the Huajoyuca de Palacios Health Center consume from 3 to 11 medications a day, with patients who have more than one comorbidity consuming more medications. In order from highest to lowest, patients with type 2 diabetes mellitus have minor polypharmacy, unlike hypertensive and dyslipidemic patients. The gender most affected by polypharmacy is the female with 82% vs. 18% the male gender of the population studied.
This research gives rise to deep study of prescription, drug interaction, adverse reactions, and pharmacovigilance, opening multiple possibilities for analysis. Future work should therefore include: Study the potentially inappropriate prescription in patients with chronic degenerative diseases, since it is the step prior to polypharmacy and drug interactions, analyze now, the possible drug interactions at the hospital level in geriatric patients, analyze whether adverse reactions in remote communities are constantly reported to COFEPRIS (Federal Commission for the Protection of Sanitary Risks), evaluate if the pharmacovigilance process is carried out in geriatric patients in remote communities, use the different analysis tools: STOP / START, Beers Criteria among others for prescription analysis.