Introduction
Dual pathology (DP) is defined as the coexistence of a substance use disorder (SUD) with another psychiatric disorder and may present in different ways, simultaneously, in the same individual over a specific period of time 1)(2)(3.
Aguilar et al. 4 state that neuropsychological vulnerability occurs mainly due to problems with self-control, self-monitoring, and anticipating consequences, thus favoring impulsive behavior and, as adolescents are in the process of developing into adults, making them more vulnerable to addiction 4. It is possible that a brain-system deficit, either inherited or acquired, could explain addictive behaviors and the concurrence of other psychiatric symptoms, which manifest at the same time that “drugs of abuse hijack the brain reward system, interrupting response behaviors to natural rewards” 5.
Although the etiological relationship that underlies this pathology is not entirely clear, it is believed that genetic, neurobiological, and epigenetic factors as well as the environment in which the individual is immersed are involved in its appearance 5)(6.
Barea et al. 7 state that, among the environmental factors, family influence plays an important role, with family conflicts related to increases in substance use and the development of behavioral problems. Serious conflicts with one’s mother go hand in hand with the development of psychoactive substance use and psychiatric disorders. This is the case with borderline personality disorder, which presents mainly in alcohol consumers, while its onset is closely related to family history (parental alcohol consumption) and problematic family dynamics, which can later become a serious problem for the affected person and trigger DP. In addition, an early age of onset in the consumption of these substances is often related to a family history of drug dependence.
As DP is not currently described in the DSM-V, it is possible that, if current classification systems for psychiatric disorders are followed, there is a high risk of its underdiagnosis. Therefore, diagnosis becomes somewhat complicated, as the manifestations of psychiatric disorders and substance use disorders must be considered simultaneously and both disorders be treated side by side 5.
It should be noted that patients with a mental or psychiatric disorder receive care from mental health networks, while drug addicts usually receive care from networks of drug addiction centers. However, those who require treatment for both disorders do not receive comprehensive care from either of these two networks 8.
Today, it is known that at least 70% of people with SUD 9 also have a psychiatric disorder, with epidemiological studies showing that the coexistence of both disorders can reach to up to 50% of the general population and up to 80% of the clinical population 10. Unfortunately, at a national level, DP is very little studied and it is unknown whether those who consume psychoactive substances develop the disorder, meaning that ascertaining whether this situation is the same all over the country is of the utmost importance. In addition, with the Pan-American Health Organization stating that the age at which the consumption of psychoactive substances begins is 13 years old 11, the early onset of consumption has become an alarming public health problem.
Material and methods
The present study comprised the observational, cross-sectional, heterodemic, unicentric, descriptive, non-experimental, and statistical scrutiny and review of the clinical records pertaining to a population of psychoactive substance consumers at the Puebla JIC, from 2019 to 2020. Informed consent was obtained from all patients for being included in the study. The research protocol was reviewed and approved by the Research Committee and Bioethics Committee at the Tepeaca Center for Advanced Study, Puebla, Mexico.
The sampling conducted was non-probabilistic, while the inclusion criteria were as follows: being between 10 and 24 years old; the consumption of more than two psychoactive substances; the presence of a possible psychiatric disorder; and, a complete clinical history. The exclusion criteria were as follows: being aged over 24 years; the consumption of a psychoactive substance, but with an incomplete clinical record and/or; failure to sign the informed consent form; and, the presence of infectious diseases such as HIV (human immunodeficiency virus), HBV (hepatitis B virus), HCV (hepatitis C virus), due to the fact that these pathologies can affect the central nervous system and cause false positives.
The data was obtained by reviewing clinical files and applying the dual diagnostic screening interview (DDSI), which determines the possible existence of psychiatric comorbidity in consumers of psychoactive substances. The adult patients with polydrug use who participated voluntarily in the research signed an informed consent form, while, in the case of minor patients, the informed consent form was signed by their parents or guardians. The interview consists of 66 questions which evaluate five different disorders: anxiety disorders (phobias, agoraphobia, and panic attacks); mood disorders (depression and dysthymia); psychosis; ADHD (Attention Deficit Hyperactivity Disorder), and, post-traumatic stress 12.
The qualitative variables were analyzed as percentages, while age (a single continuous variable) was described as both a mean and standard deviation. The results were plotted in the Microsoft Excel® program ver. 2010 and the statistical package GraphPad Prism® ver.7.0. was used for the analysis conducted for any association between the variables, itself performed using the Fisher's exact test, with a confidence interval (CI) of 95% and a statistical significance of *p<0.05.
Results
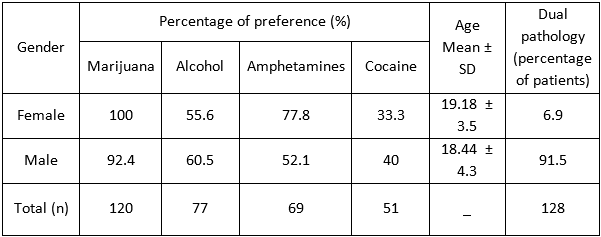
One hundred and thirty case files from various JIC treatment programs were reviewed. The female patients who met all of the inclusion criteria had an average age of 19.18 ± 3.5 years. %, while the male group’s mean age was 18.44 years ± 4.30. The present study found that marijuana (n = 120), alcohol (n = 77), amphetamines (n = 69), and cocaine (n = 51) were the most popular psychoactive substances consumed as shown in Table I.
Psychoactive substance of preference for the population studied
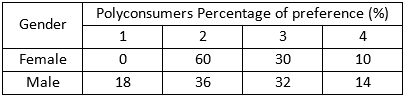
The number of and preference for psychoactive substances consumed were evaluated in this study, by gender, as shown in Table I, which shows that both genders have a preference for at least two psychoactive substances. For the female subjects, marijuana (100%) and amphetamines (77.8%) were preferred, while, for the male subjects, marijuana (92.4%) and alcohol (60.5%) were preferred.
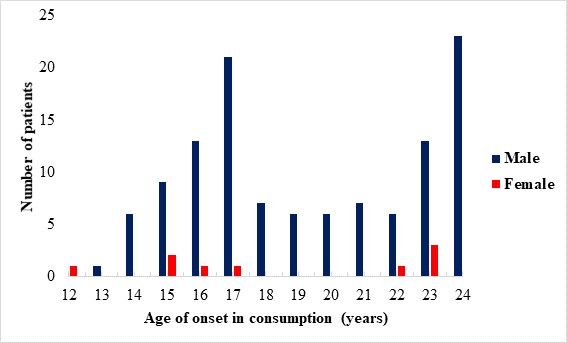
Age of onset in the consumption of psychoactive substances and number of users by age
Figure 1 shows, for both genders, the age at which subjects first used psychoactive substances, which was 12 years for both male and female subjects. The figure also sets out the age groups at which a substantial impact of the consumption of these substances is observed. In the case of male patients, the age of greatest impact is observed at 24 years, followed by 17, 23, and 16 years, while for the female gender, the age of greatest impact is 23 years, followed by 15 years.
Common psychiatric disorders in polyconsumers of psychoactive substances at the JIC
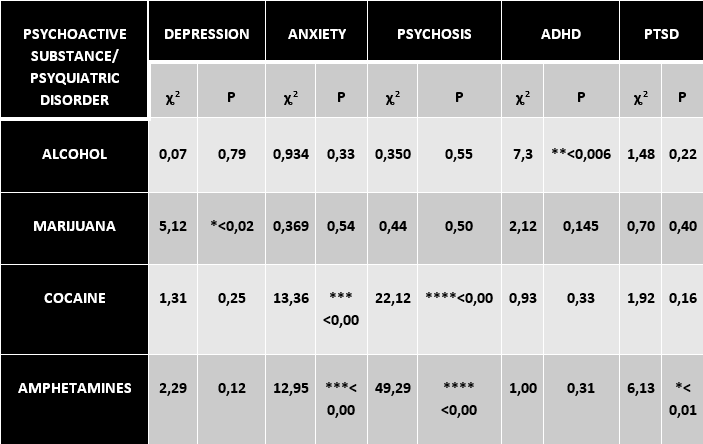
The present study found that 128 of the 130 patients presented DP, the most common psychiatric disorders like depression, anxiety, psychosis, ADHD, PTSD shown in Figure 2, found to be associated with the consumption of the psychoactive substances.
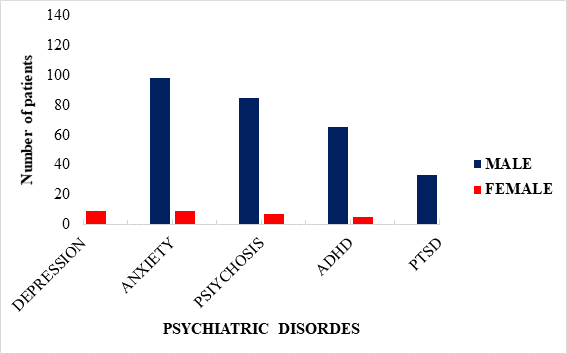
Figure 2 Common psychiatric disorders in polyconsumers of psychoactive substances at the JIC ADHD (attention deficit hyperactivity disorder) PTSD (post-traumatic stress disorder)
Nine subjects from (6.9%) the female population presented a possible dual pathology, meanwhile 119 (91.5%) patients from the male sample group presented dual pathology (see table I).
As shown in Table III, the most statistically significant associations found were marijuana with depression (*p<0.0236), cocaine and amphetamines with anxiety and psychosis (***p<0.0003 and ***p<0.0001, respectively), and amphetamines and post-traumatic stress disorder (PTSD) (*p<0.0132). The least expected finding of the present study was the association between alcohol and attention deficit hyperactivity disorder (ADHD) (**p<0.0067). No other significant association was found for the other psychiatric disorders of interest.
Discussion
Population with dual pathology and the age of onset for the consumption of psychoactive substances
As mentioned above, very few studies have been conducted in Mexico that evaluate the association between the use of psychoactive substances and the presence of psychiatric disorders, commonly known as DP. Recent studies conducted in Spain define DP as the simultaneous presentation of psychiatric and addictive pathologies, which interact with each other and modify their course and evolution. The British Royal College of Psychiatrists has defined drug abuse as "any drug use that damages or threatens to damage the physical, mental or social well-being of an individual, of various individuals or society in general" 13. The present research considered the use of psychoactive substances such as marijuana, alcohol, cocaine, and amphetamines, as shown in Figure 1, as they are the legal and, mainly, illegal substances that are best known and easiest to obtain in Mexico today.
According to the inclusion criteria, the study population was composed of patients between the ages of 10 and 24 years old, as this was the patient age group that consumed more psychoactive substances and presented dual pathologies. In this work was identified whether there is an association between the consumption of these substances and the appearance of psychiatric disorders that would give rise to the presence of DP, as shown in Table III.
A higher percentage of men (91.5%) with the presence of DP was observed (see table II). Despite the greater reported presence of DP in women, the lower percentage for women could be explained by a lower prevalence or the fact that the social stigma attached limits their attendance of treatment sessions 14.
The biological process of human development involves a period in adolescence when individuals are more vulnerable and, thus, predisposed to begin using psychoactive substances 11. This is why the adolescent and young adult population of the JIC was evaluated by the present study. Figure 1 shows that the age at which the consumption of the psychoactive substances has a pronounced impact is between 15 and 24 years, while the age of onset in the consumption of these substances is 12 years for both sexes. The consumption of these psychoactive substances also leads to people looking for an easy way to obtain them, resulting in actions that violate the law.
Psychosis and anxiety disorders are linked to cocaine and amphetamine use
Cocaine and amphetamines, such as the variant known as crystal methamphetamine, are associated with anxiety disorders and psychosis, respectively, see Table III, as these substances cause the release of dopamine (DA), which plays an imperative role in the addiction process as the common pathway in the initiation of pathological consumption. The mesolimbic and mesocortical pathways have been described as participating in behavioral disorders such as addictions. In addition, the shell region of the nucleus accumbens (NAcc) presents the most significant response to the effects of cocaine and amphetamines 15.
The increase in DA is relevant for reinforcement, just as the activation of the receptors to which it binds is critical for this phenomenon to occur. The specific increase in DA in the NAcc has been strongly related to the reinforcing effect of cocaine, in addition to enhancing its bioavailability by blocking its reuptake through the dopaminergic transporter (DAT). On the other hand, the pre-frontal cortex (PFC) receives dopaminergic projections from the VTA (ventral tegmental area) and noradrenergic projections from the LC (locus coereleus), increasing the release of DA (dopamine) in the PFC. Substances such as amphetamines block NA (noradrenaline) reuptake through the Nat noradrenaline transporter), thus increasing NA levels extracellularly 16)(17.
A long-term decrease in dopamine D2 receptors in the orbitofrontal cortex and cingulate gyrus was found in the brains of cocaine and amphetamine users by analyzing the availability of dopamine receptors and transporters, which could be interpreted as a predisposing trait that is selective for addiction. However, a significant decrease in the level of DAT has been reported in specific regions of the brains of amphetamine addicts, such as the orbitofrontal and dorsolateral frontal regions and the amygdala 18, thus explaining why these substances are specifically among the most addictive in the present day. In addition, patients with problematic amphetamine use are reported to develop post-traumatic stress disorder.
The present study found that the depression and anxiety disorders frequently found in both genders are due to the polydrug use which is common in this population at an early age and which affects the areas of greatest dopaminergic transmission. This effect on the brain results in the compulsive search for and problematic use of psychoactive substances such as marijuana, cocaine, and amphetamines. As these substances tend to cause a higher risk of the user developing these disorders, it is wise for awareness to be raised about their use.
Attention deficit hyperactivity disorder is associated with alcohol consumption
A surprising finding of the present study was the association observed between alcohol consumption and ADHD in the study population (Table III), given that references to this specific association do not appear in the existing literature. Experts explain that people use alcohol, the most preferred psychoactive substance, due to the depressant effect (caused by the release of DA and norepinephrine) triggered by its consumption. In this way, there is a decrease of the cardinal symptoms (attention deficit, hyperactivity, and impulsivity) of ADHD, so that, upon consumption of alcohol in high amounts, this disorder would result. Dopamine release is also indirectly affected by alcohol through the release of endogenous opioids, which inhibit GABAergic neurons in the ventral tegmental area, thus reducing GABA activity and increasing DA release 16. Those suffering from ADHD often consume a variety of substances (alcohol, marijuana, cocaine, stimulants, opiates, and tobacco). Wielens et al. 19 and Molina et al. 20 both found that, on average, children with ADHD start smoking approximately twice as early as their peers without ADHD.
There is evidence that alcohol consumption most affects the prefrontal cortex, inhibiting impulses such as the subject’s appetite for sex and food. This impact on the refrontal cortex inhibits the arousal mediated by NMDA receptors at a cellular level 21)(22 in addition to modulating decision-making, impulse control, adherence to norms and rules, working memory, planning, and attention.
The use of marijuana is associated with depression
The present research demonstrated the association between marijuana use and depression, see Table III, which is associated with a reduction in and deficit of the neurotransmission of serotonin, dopamine, and norepinephrine in the CNS, thus involving areas such as the basal ganglia and hippocampus. As a result of the withdrawn substance an unexpected manner, people in the population studied presented symptoms of depression, which led them to use marijuana, one of the easiest drugs to obtain, in order to achieve a sense of well-being. The use of marijuana for medicinal purposes was legalized at the beginning of 2021, with its distribution and consumption heavily regulated.
According to Amelunge 23, marijuana use is associated with such disorders as brief psychotic disorder, schizophrenia, depression, and anxiety disorder, with users also presenting psychic symptoms such as euphoria, anxiety, distrust, and paranoia, as well as disorganized, aggressive, and violent behavior 24)(25. The World Health Organization (WHO) declares that the persistent consumption of this substance predisposes the user to schizophrenia and psychosis, especially if consumption begins before the age of 18, although the present study did not observe psychotic-type disorders. The male gender is more likely to suffer from any of the above disorders when alcohol is regularly consumed, while females are more likely to attempt suicide when alcohol is frequently consumed. Finally, the consumption of the psychoactive substances of interest is influenced by a number of intrapersonal factors, which include sensation seeking and emotional instability, as well as the family environment in which the subject has been raised.
Due to the size of the sample and the conditions under which the study was conducted at the JIC, a significantly higher number of male patients were interviewed, because males are specifically involved in a much higher number of delinquent situations on a daily basis. Once apprehended and taken to the state prosecutor's office, some male young offenders are referred to the JIC for behavioral therapy, given that they sometimes commit criminal acts while under the influence of drugs, which, if the case, would have led to them being selected for participation in the present study. Female subjects are often influenced by the fact that their partners are consumers of psychotropic substances and exert pressure on them, thus initiating problematic consumption.
As the present study does not include an estimated latency time (the time in which a patient begins to present DP), future research should consider both this and the other substances that may be associated with DP and, furthermore, explore the association between alcohol and ADHD.
Conclusion
Previous studies have reported that females consume the highest quantities of the substances of interest. However, the present study determined that males consume the highest amounts of psychoactive substances and, moreover, that the age of onset in the consumption of psychoactive substances was 12 years old for both males and females, a finding which correlates with data reported by the WHO. In addition, the present study found that the psychoactive substance with the highest level of consumption in both genders in the Puebla JIC was marijuana, followed by alcohol, amphetamines, and cocaine for males and amphetamines, alcohol, and cocaine for females.
A statistically significant association between the consumption of certain psychoactive substances and the appearance of some psychiatric disorders was found, such as the association between marijuana and depression and anxiety. Meanwhile, cocaine and amphetamines were associated with psychosis and alcohol with ADHD. These findings are consistent with reports detailed in various research bibliographies in this area.