Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Ingeniería y Desarrollo
Print version ISSN 0122-3461On-line version ISSN 2145-9371
Ing. Desarro. no.26 Barranquilla July/Dec. 2009
ARTÍCULO CIENTÍFICO / RESEARCH ARTICLE
Manufacture and characterization of a mixture of Bone Powder and Bio-ceramic: A 3D-printing method process
Manufactura y caracterización de una mezcla de polvo de hueso y biocerámico procesada por impresión en 3D
Luis Carlos Parra Calvache* Fabio Arturo Rojas Mora** Diana Narváez*** Luis Miguel Méndez Moreno****
* Ingeniero Mecánico. investigador Departamento de Ingeniería Mecánica, Universidad de los Andes, Bogotá (Colombia). l-parra@uniandes.edu.co
** Doctor en Ingeniería Mecánica. Profesor Asociado, Laboratorio de Técnicas Modernas en Manufactura LATEMM, Departamento de Ingeniería Mecánica, Universidad de los Andes, Bogotá (Colombia). farojas@uniandes.edu.co
Correspondencia: Departamento de Ingeniería Mecánica, Universidad de los Andes, Cra. 1 Este No 19A-40 Edificio Mario Laserna, Bogotá D.C. (Colombia). Tel. (57 1) 3394949, ext. 2906, FAX (57 1) 3324323.
*** MSc en Biología. Investigadora Laboratorio de Genética Humana, Universidad de los Andes, Bogotá (Colombia). dmnn@hotmail.com
**** MSc en Ingeniería Mecánica. Profesor Jefe de la Sección de Automatización, Departamento de Ingeniería Mecánica y Mecatrónica, Universidad Nacional, Bogotá (Colombia). lmmendezm@unal.edu.co
Acknowledgments: it is important to acknowledge the contribution of IMOCOM S.A., which permitted the use of its 3D printing machine. The use of this machine was vital for the development of this work. It is important to acknowledge also the contribution of the Laboratory of Genetics of the Universidad de los Andes, for its support on the biological tests.
Fecha de recepción: 29 de enero de 2009
Fecha de aceptación: 2 de septiembre de 2009
Abstract
Currently, time there is a high interest in biomaterials and the way they help to improve human quality of life. This study has as objective the production of dental and orthopedic implants. These implants when used into the body of the patient would reduce the impact on a patient during and after surgery. The main purpose was to find a process to produce a compound based on bone powder and bio-ceramic capable of being absorbed by the body, and at the same time, to facilitate the body to generate a new bone structure. In this article, the production process of the bone powder is presented. Also the mixture of bone powder and bio-ceramic, processed by rapid prototyping (3D printing), is evaluated. The processed mixture products are then evaluated in its mechanical and cytotoxic behaviors in order to know its viability in the future. The biological cytotoxic test is encouraging and futures studies with the compound used are recommended.
Keywords: Bone powder, bio-ceramic, 3D printing, biomechanical and cytotoxic properties.
Resumen
En la actualidad existe un constante interés en el mundo de los biomateriales y en cómo éstos mejoran la calidad de vida de la humanidad. Este estudio surgió como un intento de producir implantes capaces de ser introducidos en el cuerpo de manera que la operación y recuperación de un potencial paciente se pudiera dar de una manera menos traumática. De esta forma se presentará el proceso para producir un compuesto a base de polvo de hueso y un biocerámico capaz de ser absorbido por el cuerpo, de manera tal que el injerto induzca el crecimiento de nuevo hueso. Se describirá cómo se produjo el polvo y cómo se realiza la mezcla con el biocerámico. La mezcla resultante fue procesada por medio de prototipaje rápido (impresión en 3D), para luego proceder a caracterizar el material en sus propiedades mecánicas y su comportamiento citotóxico con la finalidad de conocer cómo se comportaría en un ambiente in vivo. Las pruebas biológicas fueron alentadoras, lo cual puede impulsar otros estudios con el compuesto utilizado.
Palabras clave: Polvo de hueso, biocerámico, impresión 3D, propiedades mecánicas y citotóxicas.
1. INTRODUCTION
An orthopedic or dental implant is evaluated on criteria such as the recovery time of the patient and the amount of live material necessary for the implant versus the material available. When an implant is placed, the recovery of the person takes days or weeks depending on how invasive the implant is. To illustrate this point, consider the case of dental implants made of Titanium, due to one or more teeth loss [1], which demonstrates how painful a dental procedure could be. This procedure is composed of different stages. First, a base of Titanium is strongly attached to the jaw. Then, with the base properly placed, the new teeth are attached with screws. This procedure does not work well in all cases. The body could rq'ect the Titanium implant or the healing process could take a longer period than expected. In the case the healing process is successful, the histological evolution should allow a new solid tissue structure to grow between bone and the implant [2].
The length of the healing process is related to the reaction of the body to the implant, taking into account that in some cases the body rejects it. When the graft is not compatible with the immune system of the patient, it is desired that an implant be as less invasive as possible. So that, if the body of the patient rejects the graft, there is not an overly stressful period in the post operational condition.
Some implants that are to be in the body for a long period of time are usually of a considerable volume. These implants are in most cases made from bone. In some cases the volume needed is higher than the bone used as core material. Bone powder is used in some of these cases to fill gaps. Bone powder contains Hidroxyapatite (HA), Collagen and integration proteins; these proteins induce osteoinduction (new bone growth). Cements that agglutinate bone powder are used in orthopedic cases. However the agglutinated bone powder has to be given a shape to fill the bone-implant gap [3]. Hidroxyapatite, a calcium sulfate is the main compound of bone, which is brittle and along with collagen and integration proteins need to be agglutinated to form a defined shape [4]. A defined shape is given by 3D printing to medical implants in [5], but these implants need a sintering process after being printed. The high temperatures involved in the sintering process could be harmful to the integration proteins decreasing the quality of the implant.
Rojas [6] developed a method to obtain bone powders by machining. The bone powder was then intended to be processed by different methods. Rodriguez [7] described a first approach to 3D printing, obtaining an overly brittle material that in some cases cracked after being processed.
Quevedo [8] mixed the bone powder with a biopolymer. However the mechanical properties achieved were not the ones expected.
Penaloza and Rojas [9] started to develop a material composed of bone powder and a bio-ceramic, which could solve the problems mentioned before. The material obtained proved to be non-toxic, with properties good enough to believe that it can be used in medical applications. This material was based on Calcium Sulfate and Bone Powder. The material was named SCPH after its initials in Spanish (Sulfato de Calcio que aglutina Polvo de Hueso). SCPH has 80% in weight of Calcium Sulfate and 20% of Bone Powder. With the chosen material, the main goal is to find a process capable of producing any kind of geometry with a good surface quality. The process has to assure that the properties of the material are not affected, so that it can be used successfully in the future. In past work, the material was processed by injection [9], obtaining low IT qualities in the order of 11 to 13. IT refers to International Tolerance Grade; the quality varies from 01 to 18, being a tolerance of 01 the best quality and 18 the worst [10]. Keeping in mind the idea of [5] the material is going to be processed by 3D-prototyping to evaluate the effects of the process on the material properties. This article intends to work with a different powder than the one used by Rodriguez [7], having as an advantage that this 3D printing process does not need a sintering post-process period, therefore the bone integration proteins will not be affected due to high temperatures.
In order to evaluate the mechanical properties of the specimens made by prototyping the following test were held:
a) Apparent Porosity
b) Three Point Flexural test
c) Compression test
2. MATERIALS AND METHODS
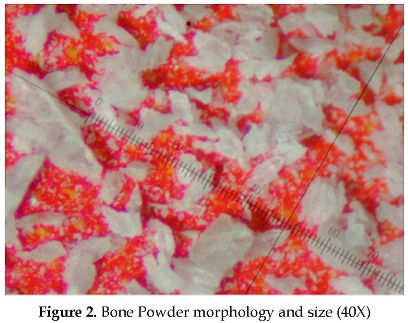
Bovine bone is similar in properties and structure to human bone. Bovine bone was used in previous studies [7], [9]. The bone powder production follows the method implemented by Rojas [6] in order to obtain a defined shape in the bone powder particles. To characterize the bone powder particles the Shape Factor is defined (SF). The Shape Factor is determined by tracing two circles in a powder particle. The outer circle is the smallest circle that contains the whole particle (BD), and the inner circle is the biggest circle that can be made inside the particle (SD). Then:

Bone powder has a volumetric, elongated, with sharp ends geometry. The mixture used has Calcium Sulfate and the previously described bone powder. This mixture was first introduced by Penaloza [9] in order to obtain a material capable of being absorbed by the body, and at the same time a material that will be an appropriate basis for the body to create a new bone structure. Calcium Sulfate is properly absorbed by the body, but it is not capable to induce bone growth [11]. Bone powder was then introduced into the material, so that it could induce a new bone structure to grow.
Calcium Sulfate is a relatively cheap ceramic material, with a Resistance to Compression of 96 MPa. When it is mixed with bone powder its mechanical properties are decreased [9]. The more bone powder the material has, the weaker the mechanical properties of the mixture and the higher its apparent porosity. The composition determined by Penaloza achieved similar properties to those of cancellous bone. In conclusion, a greater quantity of bone powder will make the bone weaker, making it useless for future implants. A too small quantity of bone powder will affect the new bone growth.
Bone Production
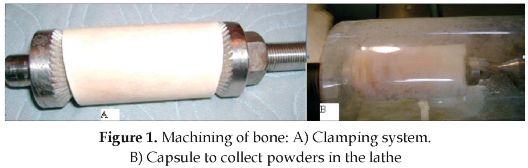
Bovine bone was selected to produce the powder. The bone was first lyophilized. The pieces were cut through its extremes and then the inner medulla (marrow) was removed. The bone was cleaned of all smooth tissue. The cleaned bone was then submerged in Hydrogen Peroxide during two days and was completely covered in salt during two weeks. After this, the bone was ready to be machined. In figure 1A it is shown the way the bone was mounted into a fixing system in order to machine it. The fixture was then mounted into the lathe as shown in figure 1B. The rig has a capsule that collects the bone powder and protects the powder from contaminants.
Cutting Parameters
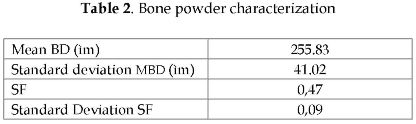
Rojas [6] made a series of experiments. Every experiment has its own parameters of work. Each experiment produced a different bone powder. In this article, the work is focused on bone powder 91. Table 2 and 3 show the parameters needed to produce such powder.
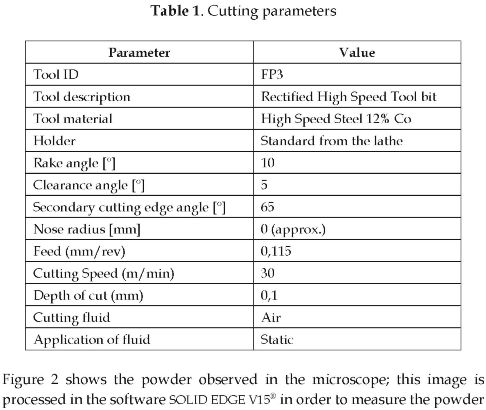
particle diameters. A total of 30 measurements were made to obtain the morphology. Table 2 presents the properties of the bone powder obtained in this study.
Mixture
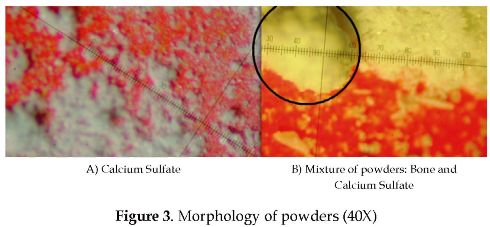
The mixture is 20% in weight of bone powder, and 80 % of bio-ceramic. It was made by taking the two components and shaking them together until there was no evidence of bone particles. The process makes the mixture as homogenous as possible and it took approximately 5 minutes to obtain the final mixture. Previous to the mixing process, the Calcium Sulfate was observed in the microscope, too. The Calcium Sulfate particles are around 25 µm in diameter. The particles tend to stay together and are easily attached to any surface. In Figure 3A the Calcium Sulfate particles are shown with no other element around. Meanwhile, in figure 3B, the Calcium Sulfate particles agglutinate around flakes of bone (see detail inside the circle), showing how the bio-ceramic adheres perfectly to the bone powder.
Prototyping
Once the SCPH mixture was obtained the powder was processed with a 3D printing machine. In figure 4 the results of a 3D printing can be seen. The screws obtained do not have a defined geometry. The properties of the processed material were then evaluated with a series of tests. These tests evaluate mechanical properties and cytotoxicity.
Apparent Porosity
The apparent porosity is determined with the following equation [12]:
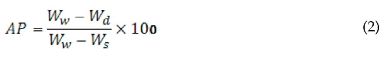
WW WW Weight of the wet specimen Wd Wd Weight of the dry specimen WS WS Weight of the specimen suspended in water
Three point Flexural and Compression tests
Following [13], specimens of 13X15X64 mm were made by prototyping in order to obtain samples to evaluate the Flexural Stress of the material. The velocity used for this test was 0.4 mm/min. And then following [14], specimens of 12.7 mm in diameter and 25.4 mm height were made in order to determine the compression stress. The velocity for this test was of 1.3 mm/min. Both tests needed a universal testing machine.
Chronic cytotoxicity
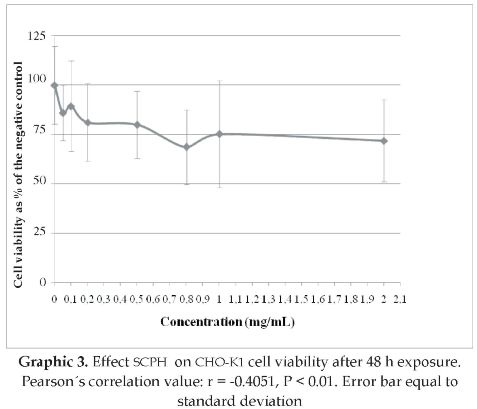
Cytotoxicity was measured by a colorimetric method using 3-[4,5-dime-thylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) [15]. It was performed in Chinese hamster ovary K1 cells (CHO-K1) exposed to the different concentrations of the SCPH. The CHO-K1 cells were grown as monolayer in Roswell Park Memorial Institute (RPMI) 1640 medium (Sigma) supplemented with 10% fetal bovine serum (FBS), 1% penicillin/ streptomycin (Gibco) and 2% glutamine (Gibco). First the SCPH was left in U.V. for 10 min in order to sterilize it. Later, in a 96 well flat bottomed plates, 3x105 cells per well were grown with eight replicate wells for each treatment (except in column 9). After 24 h. of incubation cells were treated. The ninth column was the blank consisting of 100 µl of culture medium only. The first column was the negative control which consisted of 100 µl of culture medium. The remaining wells contained 100 µl of medium with a known concentration of the SCPH (0.05, 0.1, 0.2, 0.5, 0.8, 1 and 2 mg/ml). The plate was then incubated at 37°C in a humidified 5% CO2 atmosphere for 48 h. After this time, MTT (5 mg/ml) was added to each well. Cells were incubated for further 4 h. Then, dimethylsulfoxide was added to dissolve Formazan crystals. After 5 min each well was analyzed in a BioRad micro plate reader at 595 nm, and a reference wavelength of 655 nm. The results were expressed as the percentage of living cells as calculated from absorbance detected, assuming the absorbance of negative control as 100%.
Statistical analysis
The Chronic cytotoxicity experiment was repeated two times. A Two-sample T test was performed to test differences between experiments, and a Pearson's correlation test was performed to look for correlation among cell viability and the concentrations with the statistical program Statistix 8®.
3. RESULTS
The results tend to reply the geometries made in CAD documents, but the screws do not have a shape that could be used as a future implant.
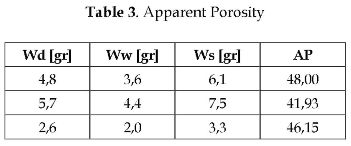
Apparent Porosity
The apparent porosity previously obtained was of 12 % [9]. In this study, after measuring 3 specimens, the apparent porosity is around 45 %. The values of each measurement are listed in table 3.
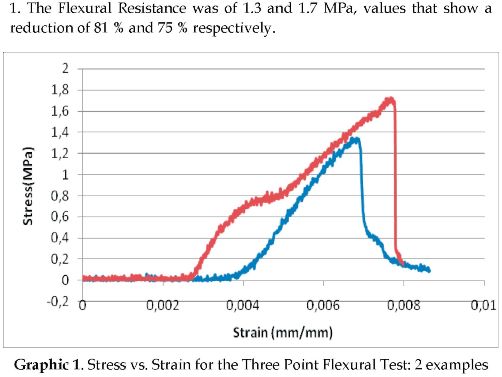
Three Point flexural test
Penaloza [9] obtained a Flexural Resistance of around 6.93 MPa. In this study, after processing the data obtained with the universal testing machine, the results obtained for two specimens are depicted in Graphic
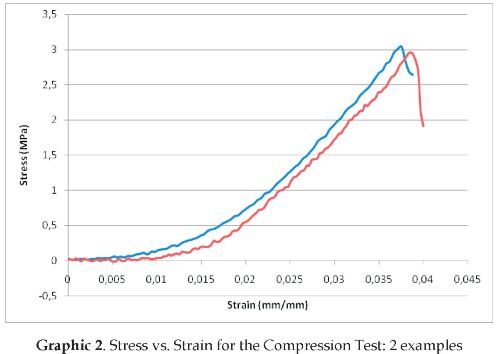
Compression Test
Penaloza [9] obtained a Compression Resistance of 7.54 MPa. In this study after processing the data obtained with the INSTRON® machine, the results obtained for two specimens can be seen in Graphic 2. The Compression Resistance was of 2.9 and 3.1 MPa, values that show a reduction of 61 % and 58 % respectively. These values are much lower than the cancellous bone Compression Resistance of 6 MPa.
Chronic cytotoxicity
After 72 h exposure to the different concentrations of the SCPH (0.05, 0.1, 0.2, 0.5, 0.8, 1 and 2 mg/ ml), CHO-K1 cells exhibit a dose-dependant viability decrease (Graphic 3). The Pearson's Correlation (r = -0.4051; P < 0.01) suggests that the increase in the concentration is significantly correlated with a decrease in cell viability. All the concentrations evaluated exhibited viability above 60%, meaning that the SCPH does not have a deadly effect over this cell line after a long period of exposure at concentrations lower than 2 mg/ml.
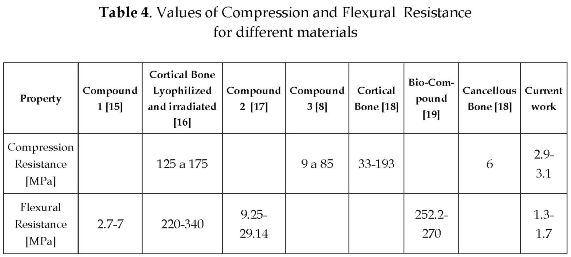
4. DISCUSSION AND CONCLUSIONS
Table 4 lists some of the results of different studies, this in order to compare the characteristics obtained in this study. The machine that processed the material was optimized for a different powder; this machine could be manipulated in order to obtain a better quality in the tests and specimens. The powder as well could be manipulated to better approximate the characteristics of the powder used in 3D printing. In the same line of thinking the binder used could be replaced to obtain a better and more compact structure of the specimens.
The main conclusions that can be made from the results observed in this study are the following. First of all, the material has an apparent porosity that could be good for the blood to flow through the implant, and could induce the growth of new bone; considering this work as a first trial, a value of AP=45% involves interconnected porosity and could involve better flooding of blood in the implant, a fact that is desirable in order to induce absorption of the implant and new bone growth.
Second, SCPH processed by 3D printing has a final shape that approximates to that of a screw. Furthermore, the material could be processed, in order to replicate different shapes. Those shapes made by 3D printing could be introduced in the body in places where the forces applied are not high, so that, the structural integrity of the implant is not in affected.
As a third observation, as mentioned before, the cytotoxic behavior of the material is promising. Another method to process SCPH has to be found and evaluated in order to produce a material that could be used successfully as an implant.
References
[I] B. Ratner, A. Hoffman, F. Schoen and J. Lemons, Biomaterial Science: Anintroduction to materials in medicine, Amsterdam: Elsevier Academic Press, 1997. [ Links ]
[2] T. Hin, Engineering materials for biomedical applications, Hackensack, NJ; Singapore: World Scientific Pub., 2004. [ Links ]
[3] S.B. Kima, Y.J. Kima, T.L. Yoonb, S.A. Parka, I.H. Choa, E.J. Kima, I.A. Kima, J-W. Shina, "The characteristics of a hydroxyapatite-chitosan-PMMA bone cement", Biomaterials, vol. 25, No 26, pp. 5715-572S, 2004. [ Links ]
[4] O. Gunduz, E.M. Erkan, S. Daglilar, S. Salman, S. Agathopoulos, F.N. Oktar, "Composites of Bovine Hydroxyapatite (BHA) and ZnO", Journal of Materials Science, vol. 43, N° 8, pp. 2536-2540, 2008. [ Links ]
[5] A. Khalyfa, S. Vogt, J. Weisser, G. Grimm, A. Rechtenbach, W. Meyer, M. Schnalbelrauch, "Development of a new Calcium Phosphate Powder- binder System for SD Printing of Patient Specific Implants", Journal of Materials Science: Materials in Medicine, vol. 18, N° 5, pp. 909-916, 2007. [ Links ]
[6] F. Rojas, "Fabricação de implantes ortepédicos a partir da usinagem de osso humano", Tesis doctoral Ingeniería Mecánica, Universidad Federal de Santa Catarina, Florianópolis (Brasil), 2000. [ Links ]
[7] J. Rodríguez, "Producción y caracterización de elementos a partir de polvo de hueso por prototipeo rápido", proyecto de grado en Ingeniería Mecánica, Universidad de los Andes, Bogotá (Colombia), 2004 [ Links ]
[8] S. Quevedo, F. Rojas, A.M. Sanabria, "Desarrollo de una metodología para la fabricación de injertos compuestos de polvo de hueso y un biopolimero", Revista Ingeniería y Desarrollo, Universidad del Norte, vol. 20, pp. 45-63, 2006. [ Links ]
[9] J. Peñaloza, "Diseño de un material compuesto para implantes óseos", proyecto de grado, Departamento de Ingeniería Mecánica, Universidad de los Andes, Bogotá (Colombia), 2007. [ Links ]
[10] J.E. Shigley, Ch. Mischke and R. Budynas, Mechanical Engineering Design. New York: McGraw-Hill series in mechanical engineering, 2003, pp. 55-58. [ Links ]
[11] C. Abjornson, J. M. Lane, "Demineralized Bone Matrix and Synthetic Bone Graft Substitutes, Bone Grafts and Bone Graft Substitutes", American Academy of Orthopaedic Surgeons. [ Links ]
[12] P. Mangonon, The principles of materials selection for engineering design. Upper Saddle River, NJ: Prentice Hall, 1999. [ Links ]
[13] ASTM D790 "Standard Test Method for Flexural Properties of Reinforced Plastics and Insulating Materials". [ Links ]
[14] ASTM D695 "Standard Test Method for Compressive Properties of Rigid Plastics". [ Links ]
[15] T. Mosmann, "Rapid colorimetric assay for cellular growth and survival -application to proliferation and cytotoxicity assays", J. Immunol. Methods, vol. 65, pp. 55-63, 1983. [ Links ]
[16] D. Reina, "Implementation de un sistema de manufactura de injerto de polvo de hueso por inyección", proyecto de grado, Ingeniería Mecánica, Universidad de los Andes, Bogotá (Colombia), 2005. [ Links ]
[17] M.M. Blaschke, F. Rojas, "Semi-destructive tests for determining properties of human bone", Memorias I Congreso Internacional de Materiales y II Encuentro Nacional de Ciencia y Tecnología de Materiales, Bucaramanga, Colombia, 2001. [ Links ]
[18] J. J. Rodríguez, F. Rojas, "Mechanical and Physical Properties of Three-Dimensional Printed Elements from Bone Powder", Memorias III Conferencia científica internacional de Ingeniería Mecánica, COMEC, Universidad Central "Marta Abreu" de las Villas, Cuba, 2004. [ Links ]
[19] T. White, The human bone manual. Amsterdam: Elsevier Academic, 2005. [ Links ]
[20] Y. Shikinami, M. Okuno, "Bioresorbable devices made of forged composites of hydroxiapatite (HA) particles and poly-L-lactide (PLLA): Part I. Basic characteristics", Biomaterials, vol. 20, pp. 859-877, 1999. [ Links ]