Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Persona y Bioética
Print version ISSN 2027-5382On-line version ISSN 0123-3122
pers.bioét. vol.20 no.1 Chia Jan./June 2016
https://doi.org/10.5294/PEBI.2016.20.1.5
AN ETHICAL EVALUATION METHODOLOGY FOR CLINICAL CASES
UNA METODOLOGÍA DE EVALUACIÓN ÉTICA PARA CASOS CLÍNICOS
UMA METODOLOGIA DE AVALIAÇÃO ÉTICA PARA CASOS CLÍNICOS
Vittoradolfo Tambone1, Giampaolo Ghilardi2
1 Università Campus Biomedico di Roma, Italia.
v.tambone@unicampus.it
2 Università Campus Biomedico di Roma, Italia.
g.ghilardi@unicampus.it
DATE RECEIVED: 2015-09-04 / DATE SENT TO PEER REVIEWERS: 2015-09-06 / DATE OF APROVAL FROM PEER REVIEWERS: 2015-11-04 / ACCEPTANCE DATE: 2015-11-07
PARA CITAR ESTE ARTÍCULO / TO REFERENCE THIS ARTICLE / PARA CITAR ESTE ARTIGO
Tambone V, Ghilardi G. An Ethical Evaluation Methodology for Clinical Cases. pers. y bioét. 2016;20(1):48-61. DOI: 10.5294/pebi.2016.20.1.5ABSTRACT
In the present article, we introduce an ethical evaluation methodology for clinical cases. Although rejecting proceduralism as a system, we develop a procedure that eventually could be formalized as a flow chart to help carry out an ethical evaluation for clinical cases. We clarify the elements that constitute an ethical evaluation: aim (patient's health), integration (action interconnections), and how the action is performed. We leave aside the aspect of intentions, focusing on the object of a medical action, arguing that the internal aim of a clinical action carries a moral value per se. Our evaluation system takes into account only objects and circumstances and their intrinsic morality, since we are dealing with the evaluation of a clinical case, and not with a personal and complete clinical action.
Keywords: Ethics; ethical evaluation; methodology; moral object; clinical case (Source: DeCS, Bireme).
RESUMEN
En el presente artículo se introduce una metodología de evaluación ética de los casos clínicos. Aunque se rechaza el procedimentalismo como sistema, se ha desarrollado un procedimiento que podría llegar a ser formalizado como un diagrama de flujo para ayudar a llevar a cabo una evaluación ética de los casos clínicos. Se aclaran los elementos que constituyen una evaluación ética: el objetivo (la salud del paciente), la integración de interconexiones (acción) y cómo se realiza la acción. Se dejan a un lado las intenciones para centrarse en el objeto de una acción médica; se argumenta que el objetivo interno de una acción clínica tiene un valor moral en sí. El sistema de evaluación tiene en cuenta solamente los objetos y las circunstancias y su moral intrínseca, ya que se trata de la evaluación de un caso clínico, y no de una acción clínica personal y completa.
Palabras clave: ética; evaluación ética; metodología; objeto moral; caso clínico (Fuente: DeCS, Bireme).
RESUMO
No presente artigo, introduz-se uma metodologia de avaliação ética dos casos clínicos. Embora rejeitemos o procedimentalismo como sistema, desenvolvemos um procedimento que poderia chegar a ser formalizado como um diagrama de fluxo para ajudar a realizar uma avaliação ética dos casos clínicos. Esclarecemos os elementos que constituem uma avaliação ética: o objetivo (a saúde do paciente), a integração de interconexões (ação) e como se realiza a ação. Deixamos de lado o aspecto das intenções e centralizamo-nos no objeto de uma ação médica, argumentando que o objetivo interno de uma ação clínica tem um valor moral em si. Nosso sistema de avaliação considera somente os objetos e as circunstâncias e sua moral intrínseca, visto que se trata da avaliação de um caso clínico, e não de uma ação clínica pessoal e completa.
Palavras-chave: ética; avaliação ética; metodologia; objeto moral; caso clínico (Fonte: DeCS, Bireme).
INTRODUCTION
The primary purpose of the ethical evaluation system presented here is not to evaluate extreme cases that can be found in the field of medicine (so-called 'frontier bioethics' cases), but rather to offer a simple methodology for determining the good and the bad of medical acts performed on a daily basis.
We begin with some clarifications regarding terminology. We use the term 'system' in its technical sense; that is, as an analytical scheme created for a multidimensional context, in relation to which the basic elements all must be used together to obtain the desired result. The clinical context presents such a multiplicity of facets, levels of intervention and possible actions that must be considered in their full complexity. For this reason, each evaluation necessarily must take all these elements into consideration. It is important, however, not to confuse our reference to the concept of system with that of scientific proceduralism. More specifically, the notion of system is frequently associated today with a proceduralistic concept of science for which, once the operative procedures are guaranteed or - in our case - evaluated, the field of ethical analysis would be completely ignored. This is not the idea behind this paper. We believe, on the contrary, that the use of procedures and systems does not necessarily imply the proceduralistic corollary3(1) that often accompanies them, just as in scientific practice the adoption of practices of reduction does not necessarily imply reductionism (2). We must make a clear distinction between means and ends.
BIOETHICS AND PROCEDURALISM (3)4
In order to understand the reasons for rejecting the proceduralist system, we would like to recall an experience of ours several years ago when Tom Lamar Beauchamp5, in replying to our question about finding a balance between possibly conflicting principles, said the external reference to the principialist system was public morals. We think this point needs to be clarified. "The ethics of procedure has its roots in Hobbes's idea of ethics, understood as a convention or institution of rules for collaboration for the benefit of and in the interest of all" (3). For Hobbes, the new moral science, in line with mathematics and geometry, becomes a form of quantifiable and verifiable mechanics, "knowledge of the causes, the passions that provoke human behavior and of the laws according to which from those causes certain infallible causes can be produced in human behavior" (4). Moral philosophy, in this way, becomes a tool for building a society capable of satisfying human needs. It becomes a regulatory science of a just society that creates and even presupposes the ever-functioning correlation 'just law = goodness'. The highest good (the absolute moral principle) becomes, in this way, a source of conflict and violence, and will be replaced by political-social paradigms that can ensure coexistence, progress and peace, as well as personal improvement. As is well known, practical reason in this context has the role of calculating efficiency based on the 19 'rules of collaboration'. Natural law no longer has a connection to God, the Creator, but to the intrinsic mathematical order of what exists. The moral norm becomes the rational norm and configures an ethics of the third person. The revived interest in Hobbes of the 1950s focused on four points: morals are interpreted as social convention aiming at collaboration; ethics is a set of rules established through negotiation; the concept of 'good' is absorbed into that of 'just'; and morals are read in mechanistic terms. Thus, there is a strong dependence on public morals.
This way of thinking essentially leads to the deferment of moral law in favor of civil law. The important question to address to this type of system is: "Now, can we say that a society is well-ordered when it is designed not only to advance the good of its members, but when it also is effectively regulated by a public conception of justice? In other words, it is a society in which 1) everyone accepts and knows that others accept the same principles ofjustice, and 2) the basic social institutions generally satisfy and are generally known to satisfy these principles" (5). Proceduralism is formally open to all the various ethical positions and, therefore, is the preferred context, even for effective political toleration. However, it is easy to see this is not true, even based solely on the fact that it theoretically and practically excludes all those positions that refer to an 'ethics of contents,' to the existence of a truth even at a gnoseological and ethical level; that is, it excludes a cognitivist position at both at a logical and ethical level. Furthermore, the conclusion that public morals must not be the concern of the various ethical positions has close ties with the drama of Nazi medicine and the definition of human rights that grew out of the Nuremberg trials. A very effective synthesis of this question is given by MacIntyre in his History of Ethics, where he asks "If, in a society of twelve people, ten are sadists who will get great pleasure from torturing the remaining two, does the principle of utility enjoin that the two should be tortured?" (6). Here, the heart of the problem is profoundly clear: consensus, in itself, does not legitimize immoral practices.
For those in the fields of medicine and scientific research, the possibility of knowing reality in a context of scientific realist cognitivism is a fundament of the rationality of what they do: if we could not know the truth, it would be useless to do a physical examination or clinical analysis, make a diagnosis or even give medication or do a follow-up; if reality could be defined by public consensus, ignorance would change the laws of physics; if we could not discover true things, research would be a mad and senseless game. Medicine and science also require, for internal coherence, a reference in a cognitivist ethical context. This is why trying to establish an ethics that focuses solely on procedure and excludes content can only result in failure. For this reason, we propose an Aristotelian Thomistic structure that can consider the content and formal/procedural aspects of moral norms.
ELEMENTS FOR AN ETHICAL EVALUATION OF CLINICAL CASES
There are three elements that are essential for an ethical evaluation:
-
The aim of a medical act is always the health of the patient (and not the good of the patient). Thus, a 'medical act' can be defined as one whose aim is the patient's health. The term 'health' will need to be redefined in a normative sense.
-
A medical act is configured as an integrated act involving various actors and competences. The convergence of various actors in a single aim, identified as the patient's health, qualifies a medical act as an integrated act. How the integration of the partial aims of the actors constituting the action can be achieved will need to be established.
-
The goodness of a medical act can be judged by how the act is performed; that is, by how the action is objectively carried out. The condition that determines that a medical act is ethically good is its being well done; that is, its adherence to the best evidence, its meeting a gold standard, its correct nosographic classification, etc.
We prefer, for now, not to introduce elements of subjective intentions into the discussion, since they would interfere with our efforts to define, as far as possible, an objective evaluation for clinical cases and not for a clinical act. We have specified that we do not want to deal with subjective intentions, because the dimension of objective intentions also exists. By 'objective intentions' we mean the directing of the agent's will towards the aim of the action itself. This directing constitutes the formal profile of the action and is, therefore, the object of an ethical evaluation. It also should be noted that this point merges with our third point: the modalities of the action depend, in large part, on the aim of the action itself. How something is done depends on the reasons for which it is done.
The goodness of the three elements brings us to evaluate a clinical case ethically. This evaluation will be part of a broader evaluation of the complete clinical act in relation to which the intentions of the agent subject will need to be evaluated as well. The distinction between clinical case and clinical act is important, because it allows for a greater internal articulation of the evaluation: in a clinical case, we evaluate both the object and the circumstances of the action; in a clinical act, besides these two elements, we also must consider intentions. We will now explain the three elements.
The aim of a medical act is the health and not the good of the patient
This statement may seem to contrast with the personalist view of medicine, which we do honor, and it may seem coherent with technicized, dehumanized and perhaps cynical clinical practice. The title of Edmund Pellegrino's principle work, For the Patient's Good (7), reflects the attitude of doctors who are respectful of the person, of a science not 'for science's sake' but 'for Man's sake,' of a clinical practice that can apply technical competence in accordance with the qualitative aspect of the patient, the families involved and society. These are all noble and widely shared intentions. However, identifying the aim of medicine (scientific practice) with the personal aim of Man (his good) makes a particular science absolute and reduces Man's personal aim to one of its aspects: health. This is why, in order to promote the truth about the human person also in relation to medicine, we need to think again about the aim of medicine, an aim that should correctly be seen as a partial aim of Man: his health.
If this were not the case, the answers about the good of a person would be found in medical science and the medical doctor would be transformed into he or she who can (and must) indicate the behavior to be followed (moral norms), evaluate the dignity of a life (ontological evaluation), regulate interpersonal relations (political/ bio-political responsibilities), supervise the reproduction and quality of the species (artificial procreation) and, naturally, ensure the happiness of individuals (care for the quality of life). Medicine, with its ancillary sciences, becomes, in this way, a vehicle for a specific and totalizing bio-politics, starting with a teleological anthropological reductionism defined by the aim of medicine. If we do not rethink this aim, it is also difficult to establish a methodology for ethically evaluating clinical cases that does not refer to a global evaluation of the act in question, precisely because it is the victim of a reductionistic vision. In other words, if I reduce the good of a person to his health, then I will evaluate a clinical act on the basis of all the human values at play: in the principialist vision, autonomy, charity and justice; in the consequentialist vision, the good of mankind; in the realist/objective vision, all the sources of morality of a human act. Thus, when we have to evaluate a clinical case, we have to evaluate everything that relates to the case in one way or another, and the evaluation becomes very complicated and difficult. But, not only will it be difficult, in our view, it also will be mistaken, because the evaluation will no longer be of the clinical case but of the human act of the doctor as a complex entity, and there is a big difference between the two.
If we evaluate a clinical act sub ratione boni and not sub ratione salutis, not only does the evaluation become unmanageable, crammed with too many different elements, but the good of health itself loses its specificity and the evaluation is no longer of the clinical act, but of the clinician. We are no longer evaluating whether the doctor is a 'good doctor' (i.e., competent), but rather whether he or she is a 'moralistically good doctor'. Admittedly, there is not necessarily a conflict between the 'goodness' and 'moral goodness' of technical competence. Ideally, there should be a virtuous relation between the two. It is the Dr. House separatistic mentality that finds a conflict between these two domains of 'good'. However, once we have clarified that they are not irreconcilable, we can and must recover the distinction between the two domains, each with its own practical physiognomy.
In the end, recognizing the practical distinctions is an act of moral reflection. The virtue of prudence can be practiced even by delegating to more specific competences, where specific areas of knowledge are involved. Here, too, specialization is not necessarily specialism ('barbaric,' as Ortega & Gasset would say) (8).
Integrated Act: Trust and Dependence as Limits or as Recognized Virtues
Human and clinical acts are not exceptions in this regard. They are constitutionally integrated. That is, they proceed from a series of other actions and trigger successive actions. Besides this temporal scheme in which they are inserted and integrated, there is also an interpersonal context in the sense that each action is in relation to the actions of others. This simple observation has interesting consequences in our case, in that the cooperative aspect (2) is an essential trait of action. In a clinical case, collaboration is a necessary ethical and scientific practice. Here, we use the term 'practice' because the actions are per force at the intersection of other actions. The practice is ethical because the collaboration can be seen as a moral virtue. It is scientific because knowledge requires continuous integration to overcome partiality. The ethical dimension is well illustrated, for example, by Edmund Pellegrino at the beginning of chapter five in Virtues in Medical Practice where he states "Trust is ineradicable in human relationships. Without it we could not live in society or attain even the rudiments of a fulfilling life. Without trust we could not anticipate the future, and we would therefore be paralyzed into inaction. Yet to trust and entrust is to become vulnerable and dependent on the good will and motivations of those we trust. Trust, ineradicable as it is, is also always problematic" (9).
MacIntyre explains our position even more clearly when he writes about the "virtues ofacknowledged dependence" (10); that is, of those capabilities that lead us to become independent and responsible subjects, thanks to the diverse relations that constitute our education within the contexts of family, school, friends, etc. All this appears in sharp contrast to a vision of individualist autonomy seen as perfection in opposition to dependence, where dependence is seen as a weakness to be overcome. In recent years, there has been much discussion about the "perversion of autonomy" (11) as Willard Gaylin and Bruce Jennings have defined it, seen as a devastating effect of a form of addiction to individualism.
All this is very important when we consider its practical application; that is, if we look at what really happens at any given level of human (and not only human) action, as in the analyses of Robert Aumnann, John Harsanyi, Reinhard Selten and John Nash regarding the existing dynamics between rationality and cooperation. Game theory is, after all, a description of reality according to applied mathematics or. as Myerson puts it, "the study of mathematical models of conflict and cooperation between intelligent rational decision-makers" (12). In other words, "game theory does not say whether or not behavior based on individual rationality is morally or ethically correct. It merely describes what rational entities acting in their own interest do" (13) and, for this reason, it helps us to see human action as integrated and cooperating.
The Morals of Work Well Done: Orthopraxis and Orthodoxy
By saying a medical act is judged also by the way it is executed, by measuring it according to guidelines, best practices and gold standards, we are affirming that the criteria of evaluation of an act are external to the act itself. A clinical act can and must conform to a model that, in a sense, precedes it. When we say an operation was a success, performed well, in accordance with the highest standards, we are expressing a comparison between the action and an ideal model that was constructed as the ideal norm for that type of operation.
It is important to stress this dynamic because here, too, a procedural norm, as we also shall see for procedures, does not have an intrinsic aim, but rather its aim changes in relation to specific contexts. When we state that an operation was performed well, 'well' indicates conformity with an archetype that cannot be restricted to a practical context.
The classical terms used to describe this process are those of orthodoxy and orthopraxis (14). The former expresses the attempt of opinion to conform to truth; the latter expresses the attempt of action to conform to good. These terms, stemming from a theological context, have undergone a particular semantic development so that orthopraxis has come to mean an action having, in itself, the criteria for its evaluation, which is precisely the point we are contesting. In other words, "good practice and good clinical practice can only exist as the effect of good science".
In synthesis, we argue that a clinical case in the context of realist/objective methodology consists of the desired object in the circumstance of the complete human act, without necessarily touching on the intentional aspect of the act. In this perspective, we have the following progression:
-
An action planned and foreseen by the subject (object of a desired act; finis operis) that will be the content of the evaluation in point 1.
-
This will be desired for a reason (intention, finis operantis) that will be the context of the evaluation in point 2.
-
The desired action, for this reason, will be carried out by determined means, through a determined collaboration, at a determined time, in a determined place, etc. (circumstances, quibus auxiliis, etc.) that will be the content of evaluation in point 3.
-
The complete human act will be evaluated (point 4) as a synthesis of the evaluations in points 1, 2 and 3.
-
The evaluation of the clinical case, on the other hand, will be a synthesis of points 1 and 3.
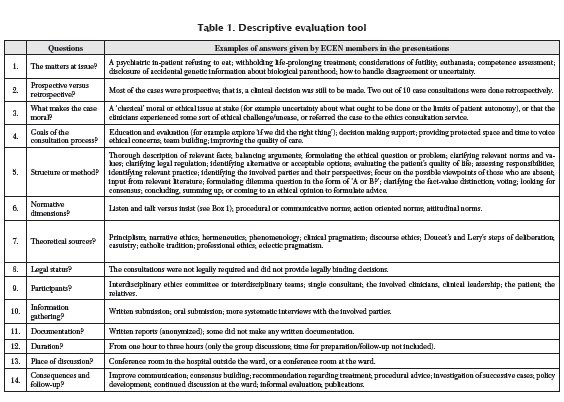
COMMENT ON AND RE-ELABORATION OF PEDERSEN'S PROPOSAL
We now will offer a detailed concrete proposal for the ethical evaluation of clinical cases. In their article, Pedersen et al. (15) examine the process of constructing and analyzing a tool for ethical evaluation in concrete clinical cases. One of the merits of their study is that it shows how these evaluations are carried out in the daily routine of clinical practice and, from these evaluations, it goes on to develop a specific evaluation scheme.
This scheme synthesizes the order of the questions posed during the evaluation. Let us closely observe the converging elements in the evaluation:
The matters at issue. That is, the concrete case under observation. In scholastic terms, this category would have been defined as the material object of the act: that which is the object of discussion. For example, the situation of a psychiatric patient who refuses to eat or how to proceed in the face of different evaluations regarding the probability of success of an operation.
Prospective versus retrospective. This category indicates the fact that the themes discussed relate both to moral decisions yet to be taken (prospective) and to situations that have already occurred (retrospective). By analogy, the results of retrospective evaluations can be applied to prospective ones. End of life decisions offer the most paradigmatic example. Per force, these decisions precede the unfortunate event and are, therefore, prospective. Thus, prospective decisions are made before the fact, having as their retrospective reference the way in which analogous events concluded. The prospective-retrospective dynamic takes this shape: I give an antibiotic to treat pneumonia (prospective aspect), on the basis of the available evidence (retrospective aspect). From this point of view, I do not consider the consequences as an ethical category, but rather as an analogical and probabilistic cognitive category that is able, for this reason, to propose a rational choice to the agent's will. What makes a case moral? This, in our opinion, is the most prominent point. It explains what makes the cases under analysis moral questions. The authors, analyzing ten case reports, observed that the answer to this question was obtained, for the most part, by exhibiting what we have defined as the material object of the evaluation. For example, what determines whether a specific case is of moral interest is seen as the fact that it deals with the autonomy of the patient, or euthanasia, or problems related to informed consent, etc. The authors make a point of noting this type of answer presupposes previous consent by the evaluators regarding what are to be considered moral problems and how to indicate them in medical practice (15).
Given the importance of this aspect of the authors' argument, we shall offer a further theoretical examination. Let us start with the original question: what makes a specific clinical case of moral interest? To answer the question, we shall adapt Kant'sfactum rationis (16) (a fact of reason), which he defined as the very existence of the question; that is, the moral nature of being human. This morality intrinsic to the question itself is not an object to be demonstrated, nor is it a judgement in Kantian terms, but a fact or primary evidence that can only be acknowledged. This recognition precedes the various possible answers that can be elaborated in relation to models of morals.
After answering this question, we must understand the morality of an action depends on various factors that have been listed above. Now, we can clarify that the morality of a specific clinical case can be separate, in some respects, from the intentional aspect ofthe agent (in scholastic terms, the finis operantis) in order to indicate the objective aspect (in scholastic terms, the finis operis)6 (17); in other words, the aspect that is most specifically related to the medical intervention. It is important to understand that the medical/clinical act itself bears a moral standing, independent ofthe intentions that move it, since it has its own form and purpose.
Let us consider this example. I want to gain access to a patient's abdomen with a scalpel. This volition is the moral object of my action (what I want to do), which can be undertaken for any number of purposes (why I want to do it): economic (I want to become rich); professional (I want to practice surgery); philanthropic (I want to save a life). All these purposes provide an answer to the 'why' of the action. At the same time, the object of the action or the 'what' (access to the patient's abdomen) remains unchanged.
Goals of the consultation process. We basically agree with the listed objectives.
Structure or method? Any evaluation procedure implicitly or explicitly refers to a clear and precise theoretical position. In our opinion, this theoretical basis must be made explicit; first, for the sake of transparent dialogue and debate, and secondly, but of equal importance, to guard against the debate becoming rhetorical, sophistic, or polemical. The debate must be rational.
Normative dimension? In line with the assumptions of cognitivist ethics, we agree with the normative instance claim of the ethical evaluation, adding that an ethical evaluation that does not derive from a normative/regulatory context would not achieve its scope.
Theoretical sources? Regarding this point, we maintain the sources of one's moral evaluations must be explicit, as we have just stated and, for the sake of their technicalscientific aspect, the best available evidence needs to be added.
Legal status? We are in full agreement about the separation of the moral and legal contexts, in keeping with the criticism of Hobbesian contractualism, which to the contrary subordinates the ethical context to the legal one. Participants? We agree that everyone affected by the decisional process must participate in it.
Information gathering? Here, too, we are basically in agreement, stressing the usefulness of having written references to what is decided.
Documentation? Also, in this case, the preference is for written documentation; the various stages of the evaluation can be retraced if necessary.
Duration? We do not think it is useful to establish a time limit for the evaluation. We believe this variable must depend on the context of the evaluation.
Place of discussion? Also, for this issue, we do not deem it necessary to specify the appropriate physical context for the evaluation. We further hold that the themes must first be studied and only discussed afterwards. This necessity might constitute an additional item.
Consequences and follow-up? We basically agree with the listed consequences, and we also maintain that a further item should be added; that is, the study of possible theoretical questions that emerge during the process of evaluation.
CONCLUSIONS
In conclusion, we can affirm that a clinical case is of moral interest for the specifically objectual aspect of its physiognomy. In other words, for every clinical intervention, we can evaluate the good or bad of the act in accordance with the intrinsic purpose of the act itself. It is easy to see that the definition of morality significantly extends the context of evaluation of clinical cases. Patient autonomy, informed consent, euthanasia, etc. are no longer seen in the traditional context. Nonetheless, this extension is in no way moralistic; it does not address the intentional context, but stays within the objectual domain of the act.
We would like to recall attention to the terminology choice we use in this last section, where we frequently mention the 'objectual aspect' of the act and not, more simply, the 'objective context'. We wanted to highlight this difference to emphasize the distinction between the objective domain, which implies, by definition, a reference to the subjectivity that aligns itself with the object, and the objectual domain, where the reference to the object prescinds from the sphere of the subject's intentions to center itself in the formal context of the object itself. If objectivity is the result of an intentionality toward the object, objectuality - as we are using the term - is the result of the conformity of the object to its form.
In this sense, it is appropriate to speak of an objectual ethics, one that is relative to the intrinsic ethicity of the human act in its formal component. We must ask ourselves, first of all, when we find ourselves faced with the work of a health worker, if the work conformed to the intrinsic purpose of the desired work, if the finis operis was achieved in the best possible way. Only after that, and as we see it, not necessarily within an ethical evaluation of a clinical case, can we proceed to considerations on the intentions with which the work was conceived.
Thus, the ethical evaluation of clinical cases that we are proposing is reduced to the desired object of the act and its circumstances. The complete evaluation of a clinical act also must include an evaluation of the intentions of the subject agent. In this respect, we do not want to take away from the importance of the 'first person' aspect, but we maintain that, in this way, we can clarify the role of the desired object and of the circumstances in the completeness of the discussion of the sources of the morality of the human act.
Here, then, are the two main points of our discussion of the evaluation of a clinical case:
-
The planned action foreseen by the subject (object of the desired act: finis operis).
-
For this reason, the desired action will be achieved by specific means, with a specific collaboration, in a specified time and place, etc. (Circumstances; quibus auxiliis, etc.).
An ethical evaluation of a clinical case is obtained through a synthesis of the moral object, the 'what' that has been done or is to be done, and the circumstances in which it has been determined to proceed; that is, the 'how' to do what has been planned.
This approach, which we have defined as 'objectual', maintains the moral object at the center of the analysis, accompanied, per force, by consideration of the circumstances. And, even if it does not intersect with the context of the intentions of the agent, it also does not exclude the possibility of this further sphere of investigation. Rather, from a certain perspective, it invokes it. The objectual approach can be combined with an analysis of intentions, but we feel this level of discussion must not, per force, be a part of the ethical evaluation of clinical cases where the morality of the action is sufficiently expressed by the object of the action and by the circumstances of its mise en pratique.
3 Although the notion of proceduralism evolved within the philosophical political debate of the previous century, specifically as a political form of liberalism, its meaning has extended to other contexts such as science, ethics and medicine, to mention only the most well-known. Regarding the problematic role of proceduralism in medicine,
4 All translations from Italian in this paper are ours.
5 Author, with Childress, of one of the best known textbooks on bioethics: Principles of Biomedical Ethics; one of best known exponents of the American proceduralistic school.
6 The comparative discussion offinis operis and finis operantis has its origins in scholasticism. The most authoritative source is Saint Thomas.
REFERENCES
1. Cavicchi I. Medicina e sanità: snodi cruciali, Dedalo, Bari 2010. [ Links ]
2. Tambone V, Ghilardi G. Riduzione consapevole e cooperante. La Clinica Terapeutica. 2012;163(3):133-143. [ Links ]
3. Tambone V. Proceduralismo e Bioetica (I). La Clinica Terapeutica. 2004;155(5):201. [ Links ]
4. Abbà F. Quale impostazione per la Filosofia Morale? Roma: LAS; 1996. [ Links ]
5. Rawls J. A Theory of Justice. Cambridge: Harvard University Press; 1999. [ Links ]
6. Mclntyre A. A Short History of Ethics, 2nd ed. New York: Macmillan; 1966. [ Links ]
7. Pellegrino ED, Thomasma DC. For the Patient's Good: The Restoration of Beneficience in Health Care. New York: Oxford University Press; 1988. [ Links ]
8. Ortega & Gasset J. The Revolt of the Masses. New York: New American Library; 1930. [ Links ]
9. Pellegrino E, Thomasma DC. Virtues in Medical Practice. New York: Oxford University Press; 1993. [ Links ]
10. MacIntyre A. Dependent Rational Animals: Why Human Beings Need the Virtues. Chicago: Open Court; 1999. [ Links ]
11. Gaylin W, Jennings B. The Perversion of Autonomy. Washington D. C.: Georgetown University Press; 2003. [ Links ]
12. Myerson RB. Game Theory: Analysis of Conflict. Cambridge: Harvard University Press; 1991. [ Links ]
13. Aumann R. Razionalità, Cooperazione, Conflitto. Morcelliana; 2008. [ Links ]
14. Tambone V, Ghilardi G. La mucca pazza e il Dottor Watson, filosofia e deontologia dell'agire medico. Roma: SEU; 2015. [ Links ]
15. Pedersen R, Hurst SA, Schildmann J, Schuster S, Molewijk B. The development of a descriptive evaluation tool for clinical ethics case consultations. Clinical Ethics. 2010;5: 136-141. [ Links ]
16. Kant E. Critique of Practical Reason (ed. 1788), 56. [ Links ]
17. Saint Thomas. Summa, IaIIae Q. 18 and Veritatis Splendor, ch. 78. [ Links ]
Inicio