Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Persona y Bioética
Print version ISSN 2027-5382On-line version ISSN 0123-3122
pers.bioét. vol.20 no.1 Chia Jan./June 2016
https://doi.org/10.5294/PEBI.2016.20.1.8
ETHICAL CONSIDERATIONS ON CASE REPORTS AND ANALYSIS OF QUALITY OF LIFE IN PATIENTS WITH COSMETIC RHINOPLASTY
CONSIDERACIONES ÉTICAS SOBRE INFORMES DE CASOS Y ANÁLISIS DE LA CALIDAD DE VIDA EN PACIENTES CON RINOPLASTIA COSMÉTICA
CONSIDERAÇÕES ÉTICAS SOBRE RELATÓRIOS DE CASOS E ANÁLISES DA QUALIDADE DE VIDA EM PACIENTES COM RINOPLASTIA COSMÉTICA
Mauro Barone1, Annalisa Cogliandro2, Paolo Persichetti3, Nicola Di Stefano4
1 University of Campus Bio-Medico of Rome, Italia.
m.barone@unicampus.it
2 University of Campus Bio-Medico of Rome, Italia.
a.cogliandro@unicampus.it
3 University of Campus Bio-Medico of Rome, Italia.
p.persichetti@unicampus.it
4 University of Campus Bio-Medico of Rome, Italia.
n.distefano@unicampus.it
DATE RECEIVED: 2015-08-17 / DATE SENT TO PEER REVIEWERS: 2015-08-19 / DATE OF APPROVAL FROM PEER REVIEWERS: 2015-10-23 / ACCEPTANCE DATE: 2015-12-03
TO CITE THIS ARTICLE / TO REFERENCE THIS ARTICLE / TO CITE THIS ARTIGO
Barone M, Cogliandro A, Persichetti P, Di Stefano N. Ethical Considerations on Case Reports and Analysis of Quality of life in Patients with Cosmetic Rhinoplasty. pers.bioét. 2016;20(1):77-85. DOI: 10.5294/pebi.2016.20.1.8
ABSTRACT
The paper discusses an ethical analysis of three common cases involving the most popular requests in rhinoplasty. As the nose plays a fundamental role in the aesthetics and physiognomy of the human face, the request for rhinoplasty may be an expression of both subjective discomfort and objective dysfunction. The paper aims, therefore, to fill the gap between qualitative-subjective impressions related to bodily self-perception and its quantitative-objective assessment. Ethical evaluation should start with consideration of the formal object and circumstances of the act, by posing the following question: Is this a real clinical case? Only after an undoubtedly positive answer to this question, should we consider specific case-related aspects; i.e., the best scientific evidence, available nosography and informed consent, before conducting an ethical evaluation of the case.
KEYWORDS: Rhinoplasty; ethical evaluation; quality of life; pre- and post-operative questionnaire (Source: DeCS, Bireme).
RESUMEN
En el artículo se describe un análisis ético de tres casos comunes relacionados con las peticiones más habituales de la rinoplastia. Como la nariz juega un papel fundamental en la estética y la fisonomía del rostro humano, la solicitud de la rinoplastia puede ser una expresión subjetiva de incomodidad y objetiva de la disfunción. El documento tiene por objeto, por lo tanto, llenar el vacío entre las impresiones cualitativas-subjetivas relacionadas con la autopercepción corporal y su evaluación cuantitativa-objetiva. La evaluación ética debe comenzar con el examen del objeto y las circunstancias del acto formal, planteando la siguiente pregunta: ¿Es este un caso clínico real? Solo después de una respuesta, sin duda positiva a esta pregunta, debemos considerar los aspectos específicos relacionados con el caso; es decir, la mejor evidencia científica, la nosografía disponible y el consentimiento informado, antes de realizar una evaluación ética del caso.
PALABRAS CLAVE: rinoplastia; evaluación ética; calidad de vida; cuestionarios pre y posoperatorios (Fuente: DeCS, Bireme).
RESUMO
Este artigo apresenta uma análise ética de três casos comuns relacionados com a maioria das petições habituais de rinoplastia. Como o nariz desempenha um papel fundamental na estética e na fisionomia do rosto humano, essa solicitação pode ser uma expressão subjetiva de desconforto e uma expressão objetiva da disfunção. Portanto, este texto tem como objetivo preencher o vazio entre as impressões qualitativas-subjetivas relacionadas com a autopercepção corporal e sua avaliação quantitativa-objetiva. A avaliação ética deve começar com o exame do objeto e as circunstâncias do ato formal, apresentando a seguinte pergunta: este é um caso clínico real? Somente após uma resposta, sem dúvida positiva a essa pergunta, devemos considerar os aspectos específicos relacionados com o caso, isto é, a melhor evidência científica, a nosografía disponível e o consentimento informado antes de realizar uma avaliação ética do caso.
PALAVRAS-CHAVE: rinoplastia; avaliação ética; qualidade de vida; questionários pré e pós-operatórios (Fonte: DeCS, Bireme).
INTRODUCTION
As the face is the most exposed and visible part of a person's body, surgical interventions on the face are the most popular among those the field of cosmetic surgery (1). The nose plays a fundamental role in the aesthetics and physiognomy of the human face (2, 3). Although we cannot easily define universal parameters of a perfect nose across cultures and ethnic backgrounds, it is possible to say the nose is located anatomically at the center of the face and any variation in its appearance causes a significant change in the features of the face as a whole (4).
Surgery is defined as a permanent action on a biological tissue that determines irreversible changes. Therefore, it is of utmost importance that the patient and the surgeon agree on a shared result that satisfies both of them. As the implementation of evidence-based medicine grows in everyday practice, there is increasing pressure to adopt validated survey instruments to demonstrate patient-reported outcomes (5). The need for ethical reflection on plastic and aesthetic surgery is also being called for (6). The aim of this paper is to analyze three cases involving patients who are candidates for rhinoplasty and to fill in the gap between the qualitative-subjective impression related to bodily self-perception and its quantitative-objective assessment. Although a subjective-qualitative evaluation is not necessarily vague or inaccurate, striving for a more objective and quantitatively measurable result brings an epistemological improvement to the surgical technique itself. This tool, in fact, will provide reliable feedback for the surgeon and the patient concerning the success of clinical practice in this regard, by taking into account a self-evaluation done by the patient and analyzed through a questionnaire constructed specifically to detect the aspects of patients' satisfaction/dissatisfaction. In order to provide an example of the process of objectification of self-perception, a questionnaire we normally use for patients who have undergone rhinoplasty (7) is introduced in the last section of this paper.
DESCRIPTION OF THE CASES
Case 1 involves a 30-year-old male patient with severe breathing problems in both nostrils. Physical examination: The patient has a septal deviation and turbinate hypertrophy that cause both the reported symptoms. He also has a severe hump in the bridge of the nose and an undefined bite with hypertrophy of the alar cartilages and DOME (a portion of alar cartilages of the nose) asymmetry. The patient's is asking to improve both the function of the nose and its aesthetic aspect. Although the patient exhibits no psycho-relational problems, he would feel more comfortable with a more harmonious nose.
Case 2 involves a 41-year-old female patient with no respiratory problems. A physical examination showed no septal deviation, a drooping tip caused by smiling, and a slight hump in the bridge. The patient brings several photographs of famous actresses to the first consultation. She wants to look like the actresses in the pictures and, therefore, has decided to request surgical intervention on her nose.
Case 3 involves a 25-years-old female patient with no respiratory problems. A physical examination showed she has a severe hump at the back of the nose and a hypertrophic tip. The patient's nose is not harmonious and she is asking to change the aesthetics of the nose so as to have a better-defined profile, an obtuse angle nose-front, an acute nasolabial angle and a 'straight nose'. The patient asks for photographs that show the predicted result of the intervention.
ETHICAL CONSIDERATIONS REGARDING THE CASES: FORMAL OBJECT AND CIRCUMSTANCES
In the present paper, we do not devise a new method for an ethical evaluation of clinical cases, as in literature presented recently (8,9); rather, we propose an evaluation of clinical practices focused on the formal object of the act and its circumstances, which have been shown to be important, particularly in cosmetic surgery (10).
Case 1
The first question, which relates to every case, is the following: Is this a clinical case? No positive answer can be taken for granted, as we always need to understand if we are dealing with a real clinical case before developing any reasonable ethical evaluation. Case 1 is surely a clinical case, as the patient presents specific symptoms that are usually addressed by medicine and, therefore, it is possible to draw a nosography. Subsequently, we could ask who are the subjects involved in the ethical evaluation. On the one hand, there are the surgeons and doctors; on the other, the patient. In this case, we can avoid considering the patient's parents or relatives, thereby narrowing the context.
Once we have ensured the patient's request is referred to the proper specialists, we need to know if the best evidence will be followed. Specifically, in Case 1, plastic surgeons need to adhere to international and scientific best practices for septal deviation and turbinate hypertrophy treatment. Then, we need to be sure the patient is informed about the surgical procedures, through appropriate and complete consent. Moreover, the patient needs to know about all future implications of the intervention. All qualitative and quantitative aspects of the patient-surgeon relationship need to be reported correctly and adequately.
Case 2
Is this a clinical case? As we argue, based on the description, this is not a plastic surgery case. The patient, in fact, presents no respiratory problem or symptoms, and the nosography cannot be referred to plastic surgery. Therefore, if this is a clinical case, it is surely not a surgical one. Hence, we need to take a step back and define whether the case can be associated with another branch of medicine; i.e., psychological or psychiatric medicine, or if it is a clinical case at all. If the case is psychological or psychiatric, the treatment must correspond to the case and it cannot be treated surgically. As far as Case 2 is concerned, consideration of the formal object suggests that it cannot be regarded as a plastic surgery case, since surgical best evidence to that effect is totally lacking.
Case 3
Case 3 is somewhat similar to Case 2, except for the fact that the patient did not bring photographs. Instead, she asked for photographs of the final result of the intervention in order to have an idea of what her post-operative appearance could be. In this case, informed consent must specifically address the fact that no prediction of surgical results can be considered reliable, since any intervention on biological tissue implies high individual variability, due to both the patient's and the surgeon's inter-variability. Therefore, the patient's request cannot be fulfilled, and she must be made aware of the fact that she might not be satisfied with the postoperative results, even if the surgical intervention were to be correct. Only after doing an adequate pre-operative information survey is it advisable to use photographs in plastic surgery to establish a proper therapeutic alliance between the doctor and the patient, and to avoid any possible misunderstanding about the post-operative outcome.
A TOOL FOR IMPROVING THE PATIENT-SURGEON RELATIONSHIP: A PRE- AND POST- OPERATIVE QUESTIONNAIRE
An experimental pilot protocol was developed based on 11 questions and administered to 105 patient-candidates who underwent aesthetic rhinoplasty. The ethics committee of the Campus Biomédico de Roma approved the questionnaire and authorized it to be administered to patients. The questionnaire was administered between August 2012 and April 2014. The pre-operative form was administered before surgery and the post-operative form, one year after surgery.
The pre- and post- operative questionnaire was comprised of 11 multiple-choice questions. The module was conceived by the authors as a self-administered test only for patients who are candidates for some type of cosmetic procedure. The questionnaires were filled out in an anonymous fashion. The pre-operative surveys were completed during the initial consultation, and the post-operative surveys were completed during the six-month post-operative visit. Because the surveys were filled out anonymously, there was no way to identify those patients who completed both the pre-operative and the post-operative surveys.
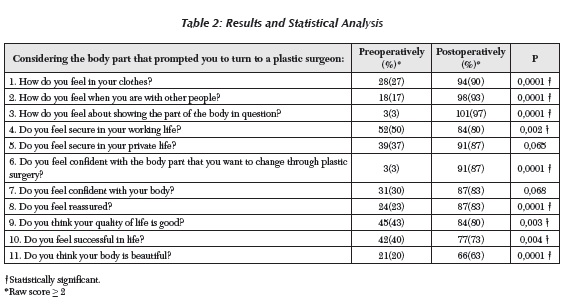
Statistical Analysis: The data obtained from the 105 questionnaires were compiled in a single Microsoft Excel™ file. Statistical analysis was performed using descriptive and summary statistics to identify a central tendency. An unpaired t test was performed to examine the significance of changes in mean scores of satisfaction. Fisher's exact test was used to detect any significant differences between pre-operative and post-operative satisfaction for a dichotomous outcome. A value of p < 0.05 was considered significant.
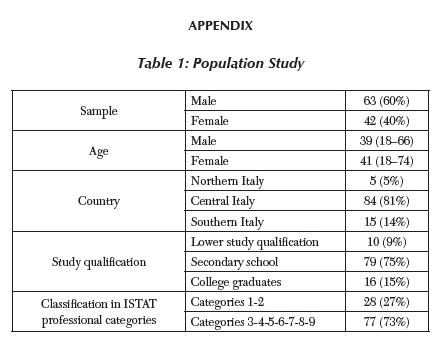
Results: One hundred five (105) patients underwent rhinoplasty between August 2012 and April 2014. All of them completed the pre- and post- operative surveys. The patient demographics are listed in Table 1 (see appendix). The average age of the patients was 39 ± 21 years in the male population and 41 ± 23 in the female population. Seventy-six (76) patients underwent closed rhinoplasty and 29 patients underwent open rhinoplasty. No patient underwent concurrent procedures. Statistically significant improvements were observed for the mean scores of all 11 surveys (See appendix, Table 2). Nine questions significantly increased their values (p<.05). Two were not significant and do not concern the aesthetic appearance of the body.
Discussion: An assessment of changes in quality of life after surgery and an exact identification of the patient's pre- and post-operative perception of body image are essential reflections for the surgeon, because patient satisfaction is the main factor that affects the success of a surgical or medical procedure (11). Only recently have surgeons begun to objectively quantify the degree of patient satisfaction and personal perception of body image (12).
Therefore, qualitative questionnaires are of utmost importance for the future development of ethical focuses on cosmetic surgery. In fact, the last decade has seen an explosion of interest in tools for assessing quality of life as a surrogate measure of overall benefit from health interventions. This interest has extended recently to the cosmetic surgery population (13). A series of measures related to health QOL (quality of life) is now available.
Most of these measures include generic elements that were not specifically created for patients undergoing cosmetic surgery and may underestimate the specific effects ofbody alteration resulting from such interventions (14). For instance, one known limitation of these generic tools for an assessment of QOL is their low sensitivity to detecting changes in healthy subjects. In addition, the continued efforts of medicine are stretched in two directions: on the one hand, to increase life expectancy and, on the other, to improve the patient's quality of life. As a result, we see medical and cosmetic surgical procedures being performed increasingly to improve the patient's subjective perception of physical appearance as a way to address self-esteem.
CONCLUSIONS
Plastic surgeons should consider whether the patient's facial proportions require rhinoplasty and must try to find the best solution to solve both aesthetic and functional problems. The nose should match the patient's identity, considering his/her nationality, gender and ethnicity, as well as cultural factors that might influence a surgical approach. The surgeon should be very careful with patients affected by body dysmorphic disorder5 who request a change in the appearance of their nose. Due to the lotus psychiatric problem, patients will never be satisfied with the post-operative results, even ifthe surgical intervention is done correctly (15). Moreover, although photographs are often useful in cosmetic surgery, it is crucial to assess the pre-operative situation and the results of rhinoplasty. Gathering adequate pre-operative information guarantees a therapeutic alliance between the doctor and the patient.
Ethical considerations need to start with a real clinical case. Therefore, it is crucial to understand if a case only seems to be clinical; i.e., surgical, or whether it concerns other branches ofspecialists to whom it should be referred in due course. Then, the focus should be on the formal object of the case; i.e., best evidence, informed consent, a full report and all the procedures that guarantee a scientifically advanced solution to the case.
5 «Individuals with body dysmorphic disorder (formerly known as dysmorphophobia) are preoccupied with one or more perceived defects or flaws in their physical appearance, which they believe look ugly, unattractive, abnormal, or deformed. The perceived flaws are not observable or appear only slight to other individuals. Concerns range from looking "unattractive" or "not right" to looking "hideous" or "like a monster." Preoccupations can focus on one or many body areas, most commonly the skin (e.g., perceived acne, scars, lines, wrinkles, and paleness), hair (e.g., "thinning" hair or "excessive" body or facial hair), or nose (e.g., size or shape). However, any body area can be the focus of concern (e.g., eyes, teeth, weight, stomach, breasts, legs, face size or shape, lips, chin, eyebrows, genitals). Some individuals are concerned about perceived asymmetry of body areas. The preoccupations are intrusive, unwanted, time-consuming (occurring, on average, 3-8 hours per day), and usually difficult to resist or control» (DSM V, p. 243).
Reference List
1. Persichetti P, Cogliandro A, Barone M.Nasal aesthetics: a cross-cultural analysis. Plast Reconstr Surg. 2013 Oct;132(4):664e-665e. [ Links ]
2. Barone M, Cogliandro A, Persichetti P. Preoperative symptoms of body dysmorphic disorder determine postoperative satisfaction and quality of life in aesthetic rhinoplasty. Plast Reconstr Surg. 2013 Dec;132(6):1078e-9e. [ Links ]
3. Picavet VA, Gabriels L, Grietens J, Jorissen M, Prokopakis EP, Hellings PW. Preoperative symptoms of body dysmorphic disorder determine postoperative satisfaction and quality of life in aesthetic rhinoplasty. Plast Reconstr Surg. 2013 Apr;131(4):861-8. [ Links ]
4. Barone M, Cogliandro A, Cagli B, Persichetti P. The face as an expression of who you are. Plast Reconstr Surg. 2015 Mar; 135(3):640e-1e. [ Links ]
5. Tambone V, Barone M, Cogliandro A, Di Stefano N, Persichetti P. How you become who you are: a new concept of beauty for plastic surgery. Arch Plast Surg. 2015 Sep;42(5):517-20. doi: 10.5999/aps.2015.42.5.517. Epub 2015 Sep 15. [ Links ]
6. K. Davis, Reshaping the female body. The dilemma of cosmetic surgery, Routledge, New York and London 1995, pp. 115-136. [ Links ]
7. Barone M, Cogliandro A, La Monaca G, Tambone V, Persichetti P. Cognitive investigation study of patients admitted for cosmetic surgery: information, expectations, and consent for treatment. Arch Plast Surg. 2015 Jan;42(1):46-51. doi: 10.5999/aps.2015.42.1.46. Epub 2015 Jan 14. [ Links ]
8. López Barreda R., Modelos de análisis de casos en ética clínica. Acta Bioethica. 2015; 21(2):281-90. [ Links ]
9. Beca, J.P., Método de decisión en ética clínica, en: J.P. Beca, C. Astete (eds.), Bioética clínica, Mediterraneo, Santiago de Chile 2012, pp. 232-243. [ Links ]
10. E.D. Pellegrino, "Rationing health care: the ethics of medical gatekeeping," Journal of Contemporary Health Law and Policy, 2 (1986), pp. 23-45. [ Links ]
11. Zojaji R, Keshavarzmanesh M, Arshadi HR, Mazloum Farsi Baf M, Esmaeelzadeh S. Quality of life in patients who underwent rhinoplasty. Facial Plast Surg. 2014 Oct; 30(5):593-6. Epub 2014 Nov 14. [ Links ]
12. Schwitzer JA, Albino FP, Mathis RK, Scott AM, Gamble L, Baker SB. Assessing demographic differences in patientperceived improvement in facial appearance and quality of life following rhinoplasty. Aesthet Surg J. 2015 Jun 10. [ Links ]
13. Litner JA, Rotenberg BW, Dennis M, Adamson PA. Impact of cosmetic facial surgery on satisfaction with appearance and quality of life. Arch Facial Plast Surg. 2008 Mar-Apr; 10(2):79-83. [ Links ]
14. Gunel C, Omurlu IK. The effect of rhinoplasty on psychosocial distress level and quality of life. Eur Arch Otorhinolaryngol. 2015 Aug; 272(8):1931-5. [ Links ]
15. Saleh AM, Younes A, Friedman O. Cosmetics and function: quality-of-life changes after rhinoplasty surgery. Laryngoscope. 2012 Feb; 122(2):254-9. [ Links ]