Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Psicología desde el Caribe
versión impresa ISSN 0123-417X
Psicol. caribe vol.30 no.1 Barranquilla ene./jun. 2013
Development of the family needs assessment tool for caregivers of individuals with neurological conditions in Latin America
Desarrollo del instrumento de evaluación de las necesidades familiares para cuidadores de personas con alteraciones neurológicas en Latinoamérica
Diego Rivera, M.S. *, Paul B. Perrin, Ph.D. **, Hugo Senra, Ph.D.*, Carlos José De los Reyes, Ph.D.***, Silvia Leonor Olivera, M.S.****, Teresita Villaseñor, Ph.D.*****, Alexander Moreno, M.S.******, Juan Carlos Arango-Lasprilla, Ph.D*******
Correspondence: Diego Fernando Rivera Camacho, M.S. Doctoral student in Clinical and Health Psychology program University of Deusto Avda. de las Universidades 24, 48007 Bilbao (Spain)Phone: +34 94 413 90 03 (ext 3231). dfriverac@deusto.es
Fecha de recepción: 1 de febrero de 2013
Fecha de aceptación: 25 de abril de 2013
Abstract
This study developed and examined the psychometric proprieties of the Spanish Family Needs Assessment Tool (FNAT) for caregivers of individuals with neurological conditions in Latin America. Twentyseven items from previously published caregiver family needs scales were combined to represent nine types of needs. These items were administered to 308 caregivers of individuals with neurological conditions in Latin America. An exploratory factor analysis suggested the retention 14 items and five factors: Household Needs, Informational Needs, Financial Needs, Health Needs, and Social Support Needs. A confirmatory factor analysis then examined the fit of the five-factor solution and suggested adequate model fit. Cronbach's alphas for the overall scale and subscales suggested acceptable internal consistency. The FNAT holds promise to help researchers and clinicians assess the family needs of caregivers in Latin America.
Resumen
El objetivo de este estudio fue evaluar las propiedades psicométricas del instrumento de evaluación de necesidades familiares (FNAT) en un grupo de 308 cuidadores de personas con alteraciones neurológicas en Latinoamérica. El FNAT consta de 27 ítems que miden algunas de las principales necesidades que experimentan los cuidadores de estas personas. Con el objetivo de determinar la estructura factorial del instrumento se realizó un análisis factorial exploratorio. Los resultados muestran que de los 27 ítems iniciales del instrumento se obtuvieron 5 factores (Necesidades de ayuda en tareas domésticas, necesidades de recibir información, necesidades apoyo financiero, necesidades de ayuda para mejorar la salud y necesidades de apoyo social) que estarían conformados por 14 ítems. Mediante un análisis factorial confirmatorio, se evaluó el nivel de ajuste de estos cinco factores cuyo resultado final muestra un ajuste adecuado del modelo y un nivel aceptable de consistencia interna tanto para la escala completa como para las subescalas. En conclusión, esta nueva versión del FNAT de 14 ítems posee buenas características psicométricas que lo hacen ser un instrumento confiable en la evaluación de las necesidades de cuidadores de personas con alteraciones neurológicas tanto en contextos clínicos como de investigación.
Keywords: Evaluación necesidades familiares, Cuidadores, Alteraciones neurológicas.
INTRODUCTION
According to the World Health Organization (World Health Organization, 2006), there are currently millions of individuals worldwide affected by neurological disorders (ND), such as stroke, traumatic brain injury, and dementia, among others. These conditions are considered one of the main causes of disability and death around the world (World Health Organization, 2004; World Health Organization, 2006). The estimated costs of disability caused by ND is about 8 billion of dollars per year in the UK (World Health Organization, 2006), and 100 billion of dollars per year in the US (World Health Organization, 2006). Therefore, ND has been considered a public health problem with high impact on economy and society (World Health Organization, 2004; World Health Organization, 2006).
In general, individuals with ND often experience a variety of physical, cognitive and emotional problems that affect their ability to live independently and to maintain a productive life (Frank, Rosenthal, Caplan, 2010; Hachinski, 2006; Markopoulou, 2010; World Health Organization, 2004; World Health Organization, 2006). Because of these problems, an individual with ND often needs permanent assistance for their everyday life activities (Almenkerk, Smalbrugge, Depla, Eefsting Hertogh, 2013; Arango-Lasprilla, Krch, Drew, De Los Reyes Aragon, Stevens, 2012; Pachalska, Manko, Chantsoulis, Knapik, Mirski, Mirska, 2012) which is often provided by their own family members (Arango-Lasprilla, Moreno, Rogers, Francis, 2009; Covinsky, Newcomer, Fox, Wood, Sands, Dane, Yaffe, 2003; Ferrara, Langiano, Di Brango, De Vito, Di Cioccio, Bauco, 2008; Kreutzer et al., 2009; Wong et al., 2008).
NDs not only affect the patient but also their family as well. Different studies (Arango-Lasprilla et al., 2009; Bartolo, De Luca, Serrao, Sinforiani, Zucchella, Sandrini, 2010; Kim et al., 2007; Kreutzer et al., 2009; Norup, Siert, Lykke Mortensen, 2010) have shown that the informal caregivers of individuals with ND are often second victims of the disease, because of the level of their involvement in the care of these individuals. There is evidence suggesting caregivers are more likely to experience physical health problems, such as hypertension (Shaw, Patterson, Ziegler, Dimsdale, Semple, Grant, 1999), decrease in immune system functioning (Kiecolt-Glaser, Marucha, Malarkey, Mercado, Glaser, 1995), cardiovascular disease (Mausbach, Patterson, Rabinowitz, Grant, Schulz, 2007), symptoms of fatigue (Webster, Grossberg, 1996), and sleep problems (Fetveit, Bjorvatn, 2006). In addition, caregivers are also at risk of having relationship changes (Morris, Morris, Britton, 1988), family conflicts (Cameron, Naglie, Silver, Gignac, 2013), poor health-related quality of life (Norup et al., 2010; Rivera-Navarro et al., 2009) , poor social and emotional well-being (Kreutzer et al., 2009), social isolation (Hammell, 1994; Stoltz, Uden, Willman, 2004), inadequate social support (Coy et al., 2013; Stoltz et al., 2004), activity restrictions (Stevens et al., 2012), poor social functioning (Coy et al., 2013; Stoltz et al.), and financial problems (Coy et al., 2013). Finally, caring for an individual with ND has also been associated with higher risk of experiencing burden (Bartolo et al., 2010; Rivera-Navarro et al., 2009; Stevens et al., 2012; Tremont, Davis, Bishop, 2006), depression and anxiety (Arango-Lasprilla et al., 2009; Davis, Sander, Struchen, Sherer, Nakase-Richardson, Malec, 2009; Kreutzer et al., 2009; Norup et al., 2010) .
Given these physical and emotional problems for the individual and family resulting from a ND, it is not surprising that caregivers have many important family needs. Some of the most frequent needs pointed out by caregivers of these individuals are (Arango-Lasprilla et al., 2010; Arango-Lasprilla et al., 2010; Cameron et al., 2013; Gan, Gargaro, Brandys, Gerber, Boschen, 2010): receiving health information, emotional support, community support, professional support and respite. In addition, most of these caregivers have to stop working to be able to care for their relatives (Arango-Lasprilla et al., 2010; Arango-Lasprilla et al., 2010; Cameron et al., 2013; Gan et al., 2010) and therefore they often experience financial and economic needs. Studies have shown that when these needs are not met, caregivers can experience even more emotional distress and therefore are less willing to support their relatives and to contribute to patient's rehabilitation outcomes (Arango-Lasprilla et al., 2010; Coy et al., 2013).
In clinical practice the appraisal of family needs of individuals with ND is a very important part of the assessment protocols since these needs play an important role in the development and implementation of the rehabilitation programs (Arango-Lasprilla, Lehan, de los Reyes, Quijano, 2012; Coy et al., 2013; McCabe et al., 2007). In the two past decades, several instruments were created to assess family needs in caregivers of individuals with ND. Many of these instruments have been widely used both in rehabilitation practice and research (Arango-Lasprilla et al., 2012; McCabe et al., 2007).
The Family Needs Questionnaire from Kreutzer and Morwitz (Kreutzer, and Marwitz, 1989) is one of the most common instruments that measure family caregivers' needs of individuals with traumatic brain injury. It is a self-administered 40-item scale which aims to provide information about family caregivers' needs after traumatic brain injury. Information is collected about family perceptions of importance of needs and the extent to which each need has been met. Sub-scales include emotional, instrumental and involvement support. These needs may be appraised during acute rehabilitation, soon after discharge, as well as long-term.
Other instrument is the Multiple Sclerosis Needs Assessment Tool (MSNA), developed by Sato and colleagues (Sato, Ricks, Watkins, 1996). This instrument consists of a questionnaire designed to ascertain the needs of caregivers of people with Multiple Sclerosis. The questionnaire is composed of 22 statements with a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Four needs categories are assessed: physical, self-concept, role function, and interdependence. Total score ranges from 22 to 110. Higher scores mean higher levels of caregivers' needs.
Finally, Junqué and colleagues (Junqué, Bruna, Mataró, 1997) developed a questionnaire to evaluate the caregivers' perceptions of the current condition of the individual with traumatic brain injury. This questionnaire comprises 59 items dealing with physical, cognitive, behavioral and affective symptoms in individuals with traumatic brain injury, and 11 items related to four domains of family caregivers.
Although there are valid and sound instruments to assess family caregivers' needs, the primary limitation of the these instruments is that the majority them were originally conceived for people of Anglo-Saxon populations and have not been adapted or validated among Spanish-speaking caregivers, including those in Latin America. Therefore, the purpose of the current study is to develop and examine the psychometric proprieties of a family needs scale for caregivers of individuals with ND in Latin America.
METHODS
Participants
Participants consisted of 308 individuals who were recruited from the cities Neiva and Bogota in Colombia, and Guadalajara in Mexico. In order to be included in the study, the individuals had to be caregivers of patients with the diagnosis of spinal cord injury (SCI), multiple sclerosis (MS), dementia, or traumatic brain injury (TBI). Caregivers were recruited by the research team primarily through house visits and health institutions (Table 1).
Description of the Sample
The majority of the sample were women (81.2%), and the average age was 49.4 years (SD=15.4) with a range of 14 to 84 years. The average length of education was 8.8 years (SD=4.9).
Measures
The Family Needs Assessment Tool (FNAT) was created based on three questionnaires addressing the family needs of people with brain damage used in previous studies (Kreutzer, Devany, & Bergquist, 1994; Junque et al., 1997; Sato et al., 1996). The initial FNAT consisted of 27 self-report items which were translated into Spanish and backtranslated for the purpose of this study. Participants were asked to assess their degree of agreement or disagreement with each of the requirements. The scale for each item range from 1 (strongly disagree) to 5 (strongly agree). These items were specifically chosen to assess needs in nine different categories, with three items corresponding to each of the nine categories: need for emotional support, need for psychological support, need for financial support, need for time to rest, need for information, need to improve health, and need for community support (Arango-Lasprilla et al., 2009).
procedures
Caregivers were contacted and informed about the purpose of the study. Those who consented to participate and met the criteria for the study were asked to fill out several questionnaires during a visit to their home or hospital center. All caregivers completed a survey of sociodemographic information as well as history of medical or psychological problems and were administered the FNAT. The interview lasted 30-0 minutes.
Statistical Methods
Response data for the FNAT were analyzed using an exploratory factor analysis (EFA) with principal axis factoring and a Promax rotation in order to determine the number of factors and items to retain. Once an initial factor solution and item composition was determined, a confirmatory factor analysis (CFA) was performed in order to examine the overall fit of the factor solution identified in the EFA. Several analyses were used to test goodness of fit: the root mean square error of approximation (RMSEA), comparative fit index (CFI), goodness of fit index (GFI), adjusted goodness of fit index (AGFI), normed fit index (NFI), incremental fit index (IFI), Tucker-Lewis index (TLI), and comparative fit index (CFI). Good model fit criteria were as follows: RMSEA must be less than .08 (Browne & Cudeck, 1993), and the other fit indices should be greater than .90 (Bentler & Bonett, 1980; Bentler, 1990). Data analyses were conducted using SPSS v.20 and AMOS v. 16.
RESULTS
Exploratory Factor Analyses (EFA)
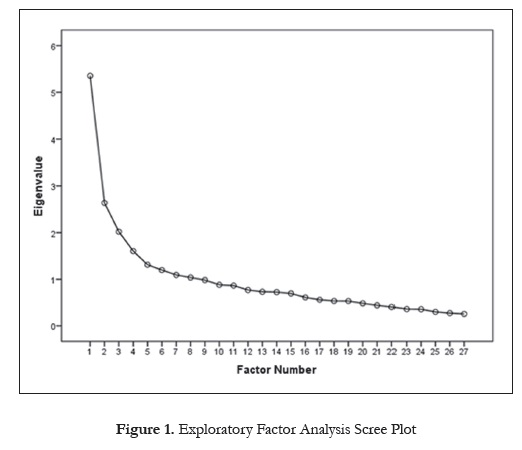
In order to determine the scale's factor structure, an EFA assuming no a priori factor structure was performed with principal axis factoring and a Promax rotation including all 27 items. A scree plot (Cattell, 1966; Figure 1) revealed a pronounced inflection points at the fifth-highest eigenvalue, or the fifth factor, with first five factors accounting 47.87% of the items' cumulative variance, suggesting the retention of a five-factor model. The factor loadings for the first five factors in this EFA appear in Table 1. An item was chosen to load onto a specific factor if it achieved simple structure, which was defined as the highest loading eigenvalue exceeding an absolute value of .40, with no other loading being higher than .10 below the highest loading eigenvalue. Items that did not achieve simple structure were considered not to be a meaningful part of the factor solution and appear at the bottom of Table 2.
Five items loaded on the first factor with simple structure. The two items with the highest loadings on this factor both represented the need for help with household chores, and as a result, Factor 1 was labeled "Household Needs". Two of the other items with lower loadings represented health needs, and the final item represented the need for more sleep. Because these three items had lower loadings on Factor 1 than did the first two items and did not represent household needs, these three items were removed from the scale.
Three items loaded onto the second factor with simple structure, all representing the need for information about the patient's disability, and as a result, Factor 2 was labeled "Informational Needs". Similarly, three items loaded onto Factor 3 representing economic needs and were thus labeled "Financial Needs". Four items loaded with simple structure onto Factor 4 which generally represented a self-appraisal of one's own health- and independence-related needs. Factor 4 was therefore labeled "Health Needs". Finally, two items loaded onto Factor 5 which each represented the needs for help from one's community or church, and as a result, this factor was labeled "Social Support Needs". The other ten items did not load with simple structure onto any of the first five factors and were removed from the scale, yielding a final scale with 14 items and five subscales.
Confirmatory Factor Analysis (CFA)
A CFA was conducted to examine the fit of the 5-factor structure in the family needs scale. The manifest variables in the CFA were the 14 items retained in the EFA, and the five latent constructs were the corresponding five subscales: Household Needs, Informational Needs, Financial Needs, Health Needs, and Social Support Needs. The model was comprised of 33 variables (33 estimated parameters), of which 14 were observed, 14 were uniquenesses, and five were factors. The confirmatory factor analysis with factor loadings (standard regression weights) appears in Figure 2. The manifest variables are those directly measured by an item, represented in Figure 2 by boxes. The latent variables are those measured indirectly from the shared variance of the manifest variables. In Figure 2, the latent variables are represented by circles.
Normality. Normality tests suggested that none of the item distributions were significantly skewed, although three were significantly kurtotic (Item 1, kurtosis coefficient = 3.00; Item 27, kurtosis coefficient = 2.34; and Item 23, kurtosis coefficient = 2.27). Further, a Mardia's coefficient of 59.32 (with a critical ratio of ratio of 24.59) suggested that the variables were multivariate kurtotic. Closer inspection revealed that data from 27 participants were significantly far away from the multivariate centroid (p < .01; i.e. multivariate outliers). The data from this small subsample are the likely source of non-normality. Because eliminating these 29 outliers would decrease the degrees of freedom and thus artificially improve the overall model fit, the outliers were retained in the analysis, providing a more conservative estimate of fit.
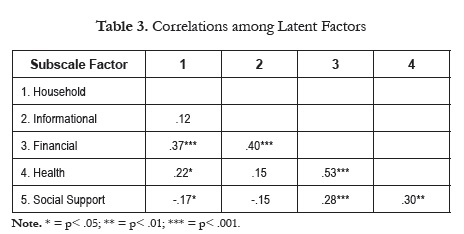
Model fit. Seven out of the 10 correlations among subscale latent factors were statistically significant (Table 2). The uniqueness terms for each scale item in the model were all significant (all ps < .004), suggesting that an amount of variance greater than 0 in each item was left unaccounted. All items loaded significantly onto their respective factor, all ps < .001 (Figure 2).
The x2 goodness-of-fit test was statistically significant, x2 (67) = 163.94, p < .001, and the ratio of the ^2 statistic to the degrees of freedom in the model was 2.45, which is slightly higher than conventional critical ratio cutoff of 2.0 for establishing good fit. The Hoelter's Index for the current model was 182 at p < .01, suggesting that a sample size of 182 would have given a non-significant x2, and as a result, would have evidenced adequate model fit. However, a sample size of 308 (the n in the current study) produced a significant x2 statistic, and therefore the large sample size influenced this statistical significance and the resulting x2 ratio, likely underestimating the model's fit.
Other evidence, however, generally supports the model's fit. The goodness of fit index (GFI) was .93, suggesting a good fit. The adjusted goodness of fit index (AGFI) and the normed fit index (NFI) were .89, and .85 respectively, where values of .90 or higher indicate an adequate fit. Similarly, the incremental fit index (IFI), Tucker-Lewis index (TLI), and comparative fit index (CFI) were .91, .87, and .90 respectively, where values close to 1.0 indicate good fit and values above .90 indicate adequate fit. The current model produced a root mean square error of approximation (RMSEA) of .069, where an RMSEA of .08 or less indicates a reasonable error of approximation and adequate fit given the model's degrees of freedom. Overall, these goodness-of-fit indices suggest that the 5-factor model fits adequately with the data.
Reliability Analyses
To investigate the scale's internal consistency reliability, Cronbach's alphas were calculated for each of the subscales and for the overall scale. The Household Needs subscale (alpha = .66), Informational Needs subscale (alpha = .74), Financial Needs subscale (alpha = .79), Health Needs subscale (alpha = .57), Social Support Needs subscale (alpha = .58), and the total score (alpha = .72), all were acceptabe given the number of items in the subscales and overall scale (Campo-Arias, Oviedo, 2008).
DISCUSSION
The purpose of this study was to develop and examine the psychometric proprieties of a family needs scale for caregivers of individuals with neurological conditions in Latin America. Twenty-seven items from previously published caregiver family needs scales were combined to represent nine types of needs. These items were administered to 308 caregivers of individuals with neurological conditions from Latin America. Data were analyzed using an exploratory factor analysis (EFA) that suggested the retention 14 items and five factors: Household Needs, Informational Needs, Financial Needs, Health Needs, and Social Support Needs. A confirmatory factor analysis (CFA) then examined the fit of the factor solution identified in the EFA and suggested adequate model fit, providing support for the development of the Spanish Family Needs Assessment Tool (FNAT). The Cronbach's alphas for the overall scale and subscales suggested adequate internal consistency.
The EFA imposing no a priori factor structure for the FNAT identified that the first five factors accounted for 47.87% of the original items' variance. Fifteen items loaded with simple structure onto these five factors and fit with the factors' conceptual foci. Upon further examination, the first factor appeared to be comprised of two separate needs: household needs and health needs, but the items loading onto Factor 1 that better conceptually represented health needs were removed because they lacked shared face validity with the other items loading onto the factor and Factor 4 more directly tapped health needs. The Household Needs subscale (Factor 1) identified in this study mirrored some of the instrumental needs identified by Kreutzer and Morwitz (Arango-Lasprilla et al., 2012), as well as some of the informal and formal support needs identified by Guberman and colleagues (Kreutzer and Marwitz, 1989). The Informational Needs subscale (Factor 2) of the FNAT addressing the need for disability-related information was similar to the informational needs component of the California Caregiver Resource Centers Uniform Assessment Tool (McCabe et al., 2007). The FNAT's Financial Needs subscale (Factor 3) addressed a similar construct as the financial conditions component of the Caregivers' Aspirations, Realities and Expectations - CARE (Kreutzer and Marwitz, 1989). The FNAT's Health Needs subscale (Factor 4) similarly resonated with the caregiver health component of the California Caregiver Resource Centers Uniform Assessment Tool and the physical and emotional health component of the CARE. Finally, the FNAT's Social Support Needs subscale (Factor 5) generally bore similarities to various components of all three other previously published scales tapping family needs that addressed receiving support from one's community. When examined holistically, the five subscales of the FNAT conformed to similar patterns of needs that had been identified in other family needs scales and caregiving populations in global regions outside of Latin America.
The fit indices of the CFA examining the FNAT's five-factor structure were generally in the adequate range, although several were below the conventional cutoff of .90. These fit indices, in combination with the significant item loadings on all latent factors, generally suggested that the five-factor structure fit adequately with the data, although future studies should continue to refine the FNAT and examine its psychometric properties in other Spanish-speaking populations. In the CFA, seven out of ten significant correlations among latent factors emerged, suggesting that shared variance existed among the five subscales. However, most of these correlations were in the small- or medium-sized range and therefore indicate that the five subscales tap unique sets of family needs. Finally, the Cronbach's alphas were adequate given the scale's overall number of items and number of items within each subscale, indicating adequate internal consistency at both the overall scale and subscale levels.
Limitations and Future Directions
Although the FNAT has potential to be an important tool for researchers and clinicians to assess the family needs of caregivers of individuals with neurological conditions in Latin America, it has several limitations that should be addressed in future studies. First, although the fit indices of the CFA were generally in the adequate range, several were not, and as a result, future investigation into the psychometric properties of the FNAT is warranted before it is definitively deemed a comprehensive measure for the assessment of family needs surrounding caregiving. Additional studies should be conducted in different caregiving populations in Latin America to determine whether the five-factor structure still holds. Second, all scale items were derived from previously published scales that had been generated in the United States, and therefore important items and family needs may exist that went uncaptured by the FNAT. Qualitative studies should be conducted to determine whether caregivers of individuals with neurological conditions in Latin America consistently report needs other than those measured by the FNAT. Third, all caregivers recruited for the current study were from either Mexico or Colombia, so the FNAT has not been validated in other countries in Latin America, and differences in dialect and even caregiving needs may limit its utility in those countries. As a result, future studies should investigate the FNAT's psychometric properties in other Spanish-speaking countries before immediately assuming that it is a valid and reliable measure in all of Latin America.
Despite these limitations, the current study was the first to generate and investigate the psychometric properties of a family needs scale for caregivers of individuals with neurological conditions in Latin America. This scale has the potential to advance research on the psychosocial and rehabilitation correlates of various family needs, as well as to help in treatment planning for families caring for a person with a neurological condition in this global region.
* Department of Methodology and Experimental Psychology. University of Deusto. Bilbao, Spain.
** Department of Psychology, Virginia Commonwealth University, Richmond, VA.
*** Departamento de Psicología. Universidad del Norte. Barranquilla, Colombia
**** Departamento de Psicología. Universidad Surcolombiana. Neiva, Huila.
*****Department of Neurosciences, Guadalajara University, Guadalajara, Mexico
******Centre de Recherche en Neuropsychologie et Cognition (CERNEC), Department of Psychology, Université de Montréal, Montréal, Québec, Canada.
******* IKERBASQUE, Basque Foundation for Science, University of Deusto. Bilbao, Spain.
References
Almenkerk S.V., Smalbrugge M., Depla M.F., Eefsting J.A., Hertogh C.M. (2013). What predicts a poor outcome in older stroke survivors? A systematic review of the literature. Disabil Rehabil. [ Links ]
Arango-Lasprilla J.C., Krch D., Drew A., De Los Reyes Aragon C.J., Stevens L.F. (2012). Health-related quality of life of individuals with traumatic brain injury in Barranquilla, Colombia. Brain Injury, 26(6), 825-33. [ Links ]
Arango-Lasprilla J.C., Lehan T., de los Reyes C., Quijano M. (2012). The ties that bind: The relationship between caregiver burden and the neuropsychological functioning of TBI survivors. Neurorehabilitation, 30(1), 87-95. [ Links ]
Arango-Lasprilla J.C., Moreno A., Rogers H., Francis K. (2009). The effect of dementia patient's physical, cognitive, and emotional/ behavioral problems on caregiver well-being: findings from a Spanish-speaking sample from Colombia, South America. American Journal Alzheimers Disease Other Dementias, 24(5), 384-95. [ Links ]
Arango-Lasprilla J.C., Plaza S., Drew A., Romero J.L, Pizarro J.A., Francis K., Kreutzer J. (2010). Family needs and psychosocial functioning of caregivers of individuals with spinal cord injury from Colombia, South America. Neurorehabilitation, 27(1), 83-93. [ Links ]
Arango-Lasprilla J.C., Quijano M., Aponte M., Cuervo M.T., Nicholls E., Rogers H.L., Kreutzer J. (2010). Family needs in caregivers of individuals with traumatic brain injury from Colombia, South America. Brain Injury, 24(7/8), 1017-1026. [ Links ]
Bartolo M., De Luca D., Serrao M., Sinforiani E., Zucchella C., Sandrini G. (2010). Caregivers burden and needs in community neurorehabilitation. Journal of Rehabilitation Medicine, 42(9), 818-22. [ Links ]
Bentler P. & Bonett D. (1980). Significance tests and goodness-of-fit in the analysis of covariance structures. Psychological Bulletin, 88 (3), 588-600. [ Links ]
Bentler P. (1990). "Comparative Fit Indexes in Structural Models". Psychological Bulletin, 107 (2), 238-46. [ Links ]
Browne M. & Cudeck R. (1993). Alternative ways of assessing model fit. In: Bollen, K. A. & Long, J. S. (Eds.) Testing Structural Equation Models (pp. 136-162). Beverly Hills, CA: Sage. [ Links ]
Cameron J., Naglie G., Silver F., Gignac M. (2013). Stroke family caregivers' support needs change across the care continuum: a qualitative study using the timing it right framework. Disability & Rehabilitation [serialonline], 35(4), 315-324. [ Links ]
Campo-Arias, A.; Oviedo, H. (2008). Psychometric properties of a scale: internal consistency. Revista de salud pública, 10 (5), 831-839. [ Links ]
Cattell R. B. (1966). Handbook of Multivariate Experimental Psychology. Chicago: Rand McNally. [ Links ]
Covinsky K., Newcomer R., Fox P., Wood J., Sands L., Dane K., Yaffe K (2003). Patient and Caregiver Characteristics Associated with Depression in Caregivers of Patients with Dementia. JGIM: Journal Of General Internal Medicine, 18(12), 1006-1014. [ Links ]
Coy A.E., Perrin P.B., Stevens L.F., Hubbard R., Díaz Sosa D.M., Espinosa Jove I.G., Arango-Lasprilla J.C. (2013). Moderated mediation path analysis of mexican traumatic brain injury patient social functioning, family functioning, and caregiver mental health. Archives Physical Medicine Rehabilitation, 94(2), 362-8. [ Links ]
Davis L.C., Sander A.M., Struchen M.A., Sherer M., Nakase-Richardson R., Malec J.F. (2009). Medical and psychosocial predictors of caregiver distress and perceived burden following traumatic brain injury. Journalof Head Trauma Rehabilitation, 24(3), 145-54. [ Links ]
Ferrara M., Langiano E., Di Brango T., De Vito E., Di Cioccio L., Bauco C. (2008). Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health and Quality Life Outcomes, 6, 6-93. [ Links ]
Fetveit A., Bjorvatn B. (2006). Sleep duration during the 24-hour day is associated with the severity of dementia in nursing home patients. International Journal Geriatric Psychiatry, 21(10), 945-950. [ Links ]
Frank R., Rosenthal M., Caplan B. (2010). Handbook of Rehabilitation Psychology (2nd ed.). Washington DC US: American Psychological Association. [ Links ]
Gan C., Gargaro J., Brandys C., Gerber G., Boschen K. (2010). Family care-givers' support needs after brain injury: A synthesis of perspectives from caregivers, programs, and researchers. Neurorehabilitation, 27(1), 5-18. [ Links ]
Hachinski V., Iadecola C., Petersen R.C., Breteler M.M., Nyenhuis D.L., Black S.E., Powers W.J., DeCarli C., Merino J.G., Kalaria R.N., Vinters H.V., Holtzman D.M., Rosenberg G.A., Wallin A., Dichgans M., Marler J.R., Leblanc G.G. (2006). National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke, 37 (9), 2220-41. [ Links ]
Hammell K.R. (1994). Psychosocial outcome following spinal cord injury. Parapkgia, 32 (11), 771-779. [ Links ]
Junque C., Bruna O., Mataro M. (1997). Information needs of the traumatic brain injury patient's family members regarding the consequences of the injury and associated perception of physical, cognitive, emotional and quality of life changes. Brain Injury, 11(4), 251-8. [ Links ]
Kiecolt-Glaser J.K., Marucha P.T., Malarkey W.B., Mercado A.M., Glaser R. (1995). Slowing of wound healing by psychological stress. Lancet, 346 (8984), 1194-1196. [ Links ]
Kim K.S., Kim B .J., Kim K.H., Choe M.A., Yi M., Hah Y.S., Chung S.J., Kwon S.H. (2007). Subjective and objective caregiver burden in Parkinson's disease. Taehan Kanho Hakhoe Chi, 37(2), 242-8. [ Links ]
Kreutzer J., Devany C, & Bergquist S. (1994). Family needs after brain injury: A quantitative analysis. Journal of Head Trauma Rehabilitation, 9(3), 104-115). [ Links ]
Kreutzer J.S., Rapport L.J., Marwitz J.H., Harrison-Felix C., Hart T., Glenn M., Hammond F. (2009). Caregivers' well-being after traumatic brain injury: a multicenter prospective investigation. Archives of Physical Medicine Rehabilitation, 90(6), 939-46. [ Links ]
Kreutzer, J., and Marwitz, J. (1989). The Family Needs Questionnaire. Richmond, Virginia: The National Resource Center for Traumatic Brain Injury. [ Links ]
Markopoulou K. (2010). Patterns of cognitive impairment in neurological disease. Current Psychiatry Reviews, 6(4), 244-251. [ Links ]
Mausbach B.T., Patterson T.L., Rabinowitz Y.G., Grant I., Schulz R. (2007). Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychology, 26(5), 539-544. [ Links ]
McCabe P., Lippert C., Weiser M., Hilditch M., Hartridge C., Villamere J.; Erabi Group (2007). Community reintegration following acquired brain injury. Brain Injury, 7; 21(2), 231-57. [ Links ]
Morris L.W, Morris R.G., Britton P.G. (1988). The relationship between marital intimacy, perceived strain and depression in spouse caregivers of dementia sufferers. British Journal of Medical Psychology, 61(3), 231-236. [ Links ]
Norup A., Siert L., Lykke Mortensen E. (2010). Emotional distress and quality of life in relatives of patients with severe brain injury: The first month after injury. Brain Injury, 24(2), 81-88. [ Links ]
Pa_chalska M., Manko G., Chantsoulis M., Knapik H., Mirski A., Mirska N. (2012). The quality of life of persons with TBI in the process of a comprehensive rehabilitation program. Medical Science Monitor, 18 (7), CR432-42. [ Links ]
Rivera-Navarro J., Benito-León J., Oreja-Guevara C., Pardo J., Bowakim Dib W, Orts E., Belló M. (2009). Burden and health-related quality of life of Spanish caregivers of persons with multiple sclerosis. Multiple Sclerosis, 15(11), 1347-1355. [ Links ]
Sato A., Ricks K., Watkins S. (1996). Needs of caregivers of clients with multiple sclerosis. Journal of Community and Health Nursing, 13 (1), 31-42. [ Links ]
Shaw WS., Patterson T.L., Ziegler M.G., Dimsdale J.E., Semple S.J., Grant I. (1999). Accelerated risk of hypertensive blood pressure recordings among Alzheimer caregivers. Journal of Psychosomatic Research, 46(3), 215-227. [ Links ]
Stevens L., Arango-Lasprilla J.C., Deng X., Schaaf IK.W, De los Reyes Aragón, C.J., Quijano, M.C., Kreutzer J. (2012). Factors associated with depression and burden in Spanish speaking caregivers of individuals with traumatic brain injury. Neurorehabilitation, 31 (4), 443-452. [ Links ]
Stoltz P., Uden G., Willman A. (2004). Support for family carers who care for an elderly person at home-a systematic literature review. Scandinavian Journal of Caring Science, 18(2), 111-119. [ Links ]
Tremont G., Davis J., Bishop D. (2006). Unique Contribution of Family Functioning in Caregivers of Patients with Mild to Moderate Dementia. Dementia & Geriatric Cognitive Disorders, 21(3), 170-174. [ Links ]
Webster J., Grossberg G.T. (1996). Disinhibition, apathy, indifference, fatigability, complaining, and negativism. InternationalPsychogeriatrics, 8 (Suppl 3), 403-408. [ Links ]
Wong P.K., Cheung G., Au A., et al. (2008). Patient and Caregiver Characteristics Associated with Depression in Dementia Caregivers. Journal Of Psychology In Chinese Societies, 9(2), 195-224. [ Links ]
World Health Organization (2004). Atlas - country resourcesfor neurological disorders. Geneve: WHO Press. [ Links ]
World Health Organization (2006). Neurological Disorders -public health challenges. Geneve: WHO Press. [ Links ]