Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Psicología desde el Caribe
On-line version ISSN 2011-7485
Psicol. caribe vol.32 no.3 Barranquilla Sep./Dec. 2015
https://doi.org/10.14482/psdc.32.3.6593
http://dx.doi.org/10.14482/psdc.32.3.6593
Spinal Cord Injury Functional Impairment and Caregiver Mental Health in a colombian sample: An exploratory study
Deficiencias funcionales en pacientes con lesiones de la médula espinal y la salud mental del cuidador: un estudio exploratorio en una muestra colombiana
Stephen K. Trapp, Ph.D.*
Gillian G. Leibach, M.S.*
Paul B. Perrin, Ph.D.*
Alejandra Morlett, M.S.*
Silvia Leonor Olivera, M.S.**
José Libardo Perdomo, B.S.***
José Anselmo Arango, B.S.***
Juan Carlos Arango-Lasprilla, Ph.D.****
*Department of Psychology, Virginia Commonwealth University, Richmond, Virginia, (Estados Unidos)
**Department of Psychology, Surcolombiana University, Neiva (Colombia)
***Department of Psychology, Universidad Cooperativa de Colombia, Neiva (Colombia)
****IKERBASQUE, Basque Foundation for Science, University of Deusto, Bilbao (España)
Correspondencia: Juan Carlos Arango-Lasprilla, Ph.D. IKERBASQUE Research Professor, Department of Psychology University of Deusto. IKERBASQUE, Basque Foundation for Science. Bilbao, Spain. Phone: (34) 608925426.jcarango@deusto.es.
Fecha de recepción: 22 de julio de 2014
Fecha de aceptación: 14 de abril de 2014
Abstract
Limited literature has examined the connections between caregiver mental health and the physical and psychosocial functioning of individuals with spinal cord injury (SCI) in Latin America, despite the dearth of services and unique needs of this population. The purpose of the current study was to examine the relationships between caregiver mental health (anxiety, burden, depression, satisfaction with life, and self-esteem) and SCI physical and psychosocial functional impairments in a Colombian sample. Forty SCI caregivers were recruited from Neiva, Colombia, and completed measures of SCI impairments and their own mental health. Greater SCI impairments, and caregiver stress due to those impairments, were associated with higher caregiver depression and anxiety, although only patient psychosocial functional impairments and related caregiver stress were uniquely associated with caregiver depression. Due to the collectivist nature of and the importance of family in many Latino cultures, mental health interventions for family members who provide care for an individual with SCI having greater psychosocial impairments may be particularly important.
Palabras clave: SCI impairment, caregivers, mental health.
Resumen
Poca literatura ha examinado las relaciones entre salud mental del cuidador y funcionamiento físico y psicosocial de las personas con traumatismo de médula espinal en América Latina, a pesar de la escasez de servicios y necesidades únicas de esta población. El propósito del presente estudio fue examinar las relaciones entre la salud mental del cuidador (ansiedad, sobrecarga, depresión, satisfacción con la vida y autoestima) y las discapacidades físicas y psicosociales de personas con traumatismo de médula espinal en una muestra colombiana. Cuarenta cuidadores de personas con traumatismo de médula espinal fueron reclutados en Neiva, Colombia, quienes completaron medidas de discapacidad del traumatismo de médula espinal y de su propia salud mental. Mayores niveles de discapacidad en personas con traumatismo de médula espinal y niveles de estrés del cuidador debido a esas discapacidades, fueron asociadas con mayores niveles de depresión y ansiedad en el cuidador, aunque sólo las discapacidades psicosociales de los pacientes y el estrés relacionado con el cuidador fueron asociados con la depresión en el cuidador. Debido a la naturaleza colectivista y la importancia de la familia en la mayoría de las culturas latinas, las intervenciones centradas en la salud mental de los familiares que cuidan de personas con traumatismo de la medula espinal pueden ser particularmente importantes.
Keywords: lesión medular, cuidadores, salud mental.
INTRODUCTIÓN
Spinal cord injury (SCI) is a traumatic injury to the spine that damages the spinal cord or local nerves (Elliott & Rivera, 2003). Common causes of SCI include falls, motor vehicle accidents, disease, and violence such as gunshot wounds and explosions (Chen, Tang, Vogel, & DeVivo, 2013). The global incidence rates of SCI range from 10.4 to 83 million per each year, and prevalence rates are estimated between 223 to 755 cases per million (Wyndaele & Wyndaele, 2006).
As a result of SCI, changes in physical functioning can vary from weakness to loss of sensation at or below the area of the injury depending on the injury site and severity of the lesion (Mc-Donald & Sadowsky, 2002). Further, chronic comorbid complications, such as infections and pressure sores are common post-injury (McKinley, Jackson, Cardenas, & De Vivo, 1999), as well as chronic pain, urinary tract infections, bladder cancer, impaired sexual functioning, renal stones, and gallstones (Charlifue, Weitzenkamp, & Whiteneck, 1999; Fisher et al., 2002; Priebe et al., 2007). Functional impairments can be pervasive, and rehabilitation may require regular medical care, including multifaceted home-based care involving caregivers (Burns & Ditunno, 2001).
In addition to physical challenges associated with SCI, psychosocial difficulties, including anxiety, depression, impaired vocational functioning, and decreased quality of life, are also common (Kannisto, Merikanto, Alaranta, Hokkanen, & Sintonen, 1998; Kemp, Krause, & Adkins, 1999; Kennedy & Rogers, 2000; Kennedy, Lude, & Taylor, 2005; Krause et al., 1999; Post & van Leeuwen, 2012). Although rates of psychosocial disturbance are variable, one study found that almost half of the individuals with SCI surveyed had experienced one or multiple symptoms of depression, symptoms of anxiety, clinically notable stress, or posttraumatic stress disorder (Migliorini, Tonge, & Taleporos, 2008). Studies conducted in developing nations have found similar comorbid psychosocial experiences. Two studies from Colombia found that individuals with SCI reported poorer overall health related quality of life (e.g., role limitations related to social functioning, role limitations related to physical functioning, lower general health, and higher pain; Arango-Lasprilla, Nicholls, Olivera, Perdomo, & Arango, 2010) and low rates of acceptance and comorbid depression (Nicholls et al., 2011).
Due to the many challenges associated with having an SCI (e.g., physical health, environmental obstacles), restoration of independent living post-injury is often hampered, and it is common for individuals with SCI to need someone to take on various caregiving tasks (Chen & Boore, 2008; Vissers et al., 2008; Whiteneck, Tate, & Charlifue, 1999). Caregiving for an individual with SCI has been found to be exceedingly time consuming, stressful, and associated with deleterious effects on mental health and overall quality of life for the caregiver (Blanes, Carmagnani, & Ferreira, 2007; Boschen, Tonack, & Gargaro, 2005; Chen & Boore, 2008; Raj, Manigandan, & Jacob, 2006; Shewchuk, Richards, & Elliott, 1998). In a cross sectional study conducted in Brazil, it was found that SCI caregivers reported lower overall health-related quality of life and greater burden (Blanes et al., 2007). Significant associations between the physical and psychosocial challenges faced by the individual with SCI and caregiver burden have been found (Post, Bloemen, & De Witte, 2005). In a study examining the relationship between family needs and psychosocial functioning of Colombian SCI caregivers, family needs were associated with depression, burden, and dissatisfaction with life (Arango-Lasprilla, et al., 2010). Further, health related quality of life in individuals with SCI has been associated with mental health of caregivers in Latin America as well (Coleman et al., 2013).
Although the pathophysiology of SCI is similar internationally, the causes, course, and treatment options vary across global regions (Ackery, Tator, & Krassioukov, 2004). For example, motor vehicle accidents are the principal cause of SCI in developed nations, whereas violence and steep falls are common causes of SCI in developing countries (Ackery et al., 2004). Further, notable differences exist between developed and developing nations in rehabilitation services and outcomes, as for example, life expectancy is estimated at less than two years for individuals with SCI in developing nations (Burns & O’Connell, 2012) with greater long-term suvival in developed nations (DeVivo, Krause, & Lammertse, 1999; DeVivo, & Chen, 2011; Middleton et al., 2012; Strauss, DeVivo, Paculdo, & Shavelle, 2006). Further, a variety of challenges exist in SCI rehabilitation in developing nations, including treatment of acute injury, assessment and evaluation, medical management, secondary complications, access to equipment, community reintegration, follow-up care, and culturally-pertinent medical services (Burns & O’Connell, 2012).
SCI rehabilitation literature from developed nations has established a base of evidence for the association between caregiver mental health and the physical and mental health of individuals with SCI (Post et al., 2005; Schulz, Tompkins, Wood, & Decker, 1987). However, very limited literature has examined these connections in developing global regions like Latin America, despite the lack of rehabilitation services and reduced life expectancy after SCI in those regions (Burns & O’Connell, 2012). To attend to this gap in the literature, the purpose of the current study was to examine the relationship between caregiver mental health and SCI functional impairment in a Colombian sample. Caregiver mental health variables included anxiety, burden, depression, satisfaction with life, and self-esteem. SCI-related functional impairments were divided into two categories: psychosocial problems and physical problems. Further, this study examined the relationships between caregiver stress due to these two types of problems in individuals with SCI and caregiver mental health.
METHOD
Participants
Forty SCI caregivers were recruited from the Foundation for the Integral Development of People with Disabilities, a not-for-profit organization that provides psychosocial services (e.g., counseling, social work, and meeting spaces) to individuals living with a disability and their caregivers in Neiva, Colombia. Medical record examination allowed for identification and subsequent recruitment efforts targeting individuals who sought psychosocial care for challenges related to an SCI. Inclusion criteria for caregivers included being over the age of 18, being the primary caregiver, and providing dayto-day care for a person with SCI least 6 months post-injury, having no history of alcohol/drug abuse, psychiatric conditions, or neurological conditions.
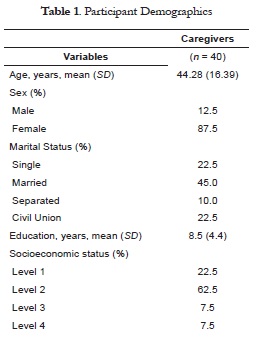
The majority of participants were female (87.5%), the mean age was 44.3 years (SD = 16.4), and caregivers’ mean number of years of education was 8.5 (SD = 4.4). Caregivers fell into the following socioeconomic status categories (of 6 levels of socioeconomic status defined by the Colombian government): Level 1 (22.5%), Level 2 (62.5%), Level 3 (7.5%), and Level 4 (7.5%). Most of the caregivers were parents of the individual with SCI (45%), while the others were a spouse (27.5%), sibling (15%), other relative (5%), professional caregiver (5%), or friend (2.5%). The marital statuses of caregivers were as follows: married (45%), single (22.5%), civil union (22.5%), and separated (10%). Caregivers dedicated an average of 80.8 hours (SD = 46.3) per week to caregiving.
Measures
SCI Functional Impairment Questionnaire
A series of SCI common functional impairments and related medical conditions were queried for and aggregated into two factors: physical and psychosocial. Items assessed the presence of the SCI-related functional impairments or medical conditions (1 = "yes," 2 = "no") and the level of caregiver stress associated with the impairment. Physical examples included "loss of bladder control," "respiratory muscle paralysis," and "sexual disturbances," while psychosocial examples included "depression," "irritability," and "lack of motivation." Stress was rated on a four-point Likert type scale (ranging from 1 = "no stress" to 4 = "much stress").
Patient health Questionnaire-9 (PhQ-9)
The PHQ-9 (Kroenke & Spitzer, 2002) was used to assess caregiver depressive symptoms. Nine items utilizing a four-point Likert type scale (ranging from 0 = "not at all" to 3 = "nearly every day") indicated how frequently a participant is bothered by a depressive symptom (e.g., "poor appetite or overeating," "little interest or pleasure in doing things"). The total score ranges from 0 to 27, and higher scores indicate higher levels of depressive symptoms. The present study administered a Spanish version of the PHQ-9, which studies have previously demonstrated evidence for validity and reliability for administration to Spanish speakers (Diez-Quevedo, Rangil, Sanchez-Planell, Kroenke, & Spitzer, 2001; Donlan & Lee, 2010; Wulsin, Somoza, & Heck, 2002).
Zarit Burden Interview (ZBI). Caregiver burden was measured with the ZBI (Zarit, Reever, & Bach-Peterson, 1980). The scale assesses the extent to which being a caregiver affects the caregiver’s psychological well-being, social status, health status, and financial status. The 22 questions are scored on a five-point Likert type scale in which burden is rated from "never" to "nearly always." The final score is summed and ranges from zero to 88. Evidence for the validity of a Spanish version was used in the current study (Martin-Carrasco et al., 2010).
Satisfaction with Life Scale (SWLS). General life satisfaction was assessed with the SWLS (Pavot & Diener, 1993), which has been found to have adequate reliability and validity in neurological populations (Putzke, Richards, Hicken, & DeVivo, 2002). Five items utilizing a sevenpoint Likert type scale allow participants to rate their general life satisfaction from "strongly agree" to "strongly disagree." The final score is summed and ranges from five to 35. A Spanish version was used in the present study and has demonstrated adequate internal consistency (Martínez et al., 2004).
State Trait Anxiety Inventory (STAI). State and trait anxiety were measured by the STAI (Spielberger & Gorsuch, 1983). Twenty items were assessed using a four-point Likert type scale to rate the experience of anxiety from zero (not at all) to three (very much so). A summed score is calculated, and higher scores indicate higher levels of perceived anxiety. In this study, a well-validated Spanish version was used (Novy, Nelson, Smith, Rogers, & Rowzee, 1995; Spielberger & Díaz-Guerrero, 1975; Virella, Arbona, & Novy, 1994).
Rosenberg’s Self-Esteem Scale (RSES). The RSES (Rosenberg, 1965) was utilized to measure participants’ sense of self-worth. The RSES is a 10-item scale that uses four-point response options ranging from "strongly agree" to "strongly disagree." In the summed score, higher scores indicate higher self-esteem. Sample items include: "I feel I do not have much to be proud of " and "I am able to do things as well as most other people." Cross cultural evidence has shown that the RSES is appropriate for use with Spanish speakers in Central and South American countries (Schmitt & Allik, 2005).
PROCEDURE
SCI caregivers were recruited at the Foundation for the Integral Development of People with Disabilities in Neiva, Colombia. Permission to conduct the study was provided by the ethics committee at Surcolombiana University. Participants were identified through a medical records review, and those caregivers who met study criteria were contacted. If the caregiver expressed interest, an appointment was scheduled to meet at the participant’s home, and all participants provided informed consent. The study was comprised of an interview and selfreport measures administered by a psychologist. The study took approximately 45 minutes to complete.
Data Analyses
Five multiple regressions were run in which the two independent variables were patient psychosocial and physical health functional impairments, and the dependent variables were each of five caregiver psychosocial health indices (e.g., depression, burden, satisfaction with life, self-esteem, and anxiety). An additional five multiple regressions were run in the same manner, but with caregivers’ reported stress associated with patient psychosocial and physical health functional impairments as the independent variables. Because of the exploratory nature of this study, all regressions used an alpha of .10 to provide a more sensitive estimation of relationships among the variables. Finally, a correlation matrix was run showing the bivariate correlations among all outcome variables in the study, and the traditional alpha level of .05 was still retained for identifying significant bivariate correlations because of the reduced demands on degrees of freedom for correlations in comparison to multiple regressions.
RESULTS
Depression
Functional Impairments. To examine whether patient psychosocial and physical functional impairments would be associated with caregiver depression, these two variables were entered into a simultaneous multiple regression as independent variables. The overall model was significantly associated (with an alpha = .10) with depression, F(2, 39) = 2.69, p = .082, R2 = .127. In this model, only patient psychosocial functional impairments were independently related to caregiver depression, β = -.38, p = .027.
Stress. To examine whether caregivers’ stress due to patient psychosocial and physical functional impairments were associated with caregiver depression, these two stress variables were entered into a multiple regression. The overall model was significantly associated with caregiver depression, F(2, 39) = 3.36, p = .045, R2 = .154. Again, only patient psychosocial functional impairments were independently related to caregiver depression, β = .42, p = .067.
Burden, Satisfaction with life, and Self-esteem
Functional Impairments. Three separate regressions with patient psychosocial and physical functional impairments as independent variables did not demonstrate a significant association with caregiver burden, F(2, 39) = .93, p = .403, R2 = .05, satisfaction with life, F(2, 39) = .62, p = .545, R2 = .03, or self-esteem, F(2, 39) = 1.18, p = .318, R2 = .06.
Stress. Similarly, three regressions with the caregiver stress due to patient psychosocial and physical functional impairments did not yield a significant association with caregiver burden, F(2, 39) = 1.38, p = .265, R2 = .07, satisfaction with life, F(2, 39) = .72, p = .492, R2 = .04, or self-esteem, F(2, 39) = .03, p = .972, R2 = .00.
Anxiety
Functional Impairments. To examine whether patient psychosocial and physical functional impairments were associated with caregiver anxiety, these two variables were entered into a multiple regression as independent variables, yielding an overall significant model, F(2, 39) = 2.60, p = .088, R2 = .12. However, in this model, neither independent variable was uniquely related to caregiver anxiety.
Stress. To examine whether caregivers’ stress due to patient psychosocial and physical functional impairments were associated with caregiver anxiety, these two stress variables were entered into a multiple regression. The overall model was statistically significant, F(2, 39) = 2.54, p = .093, R2 = .12, however, again, neither independent variable was uniquely associated with caregiver anxiety.
Correlation Matrix
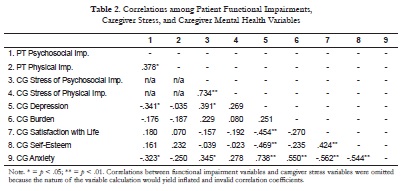
A correlation matrix was calculated showing the bivariate relationships among all variables in the current study. Significant correlations emerged between the patient psychosocial and physical functional impairments and between the two types of caregiver stress due to these impairments. Patient psychosocial impairments and caregiver stress associated with these functional impairments were both significantly correlated with caregiver depression and anxiety. Patient physical impairments and associated caregiver stress were not significantly correlated with caregiver mental health. Caregiver depression was significantly correlated with other caregiver mental health variables: satisfaction with life, self-esteem, and anxiety. Caregiver anxiety was also significantly correlated with caregiver burden and satisfaction with life.
DISCUSSION
Limited literature has examined the connections between caregiver mental health and the physical and psychosocial functioning of individuals with SCI in Latin America, despite the dearth of services and unique needs of this population (Burns & O’Connell, 2012). The purpose of the current study was to examine the relationships between caregiver mental health (anxiety, burden, depression, satisfaction with life, and self-esteem) and SCI physical and psychosocial functional impairments in a Colombian sample. Greater SCI impairments, and caregiver stress due to those impairments, were associated with higher caregiver depression and anxiety, although only patient psychosocial functional impairments and related caregiver stress were uniquely associated with caregiver depression.
Depression and Anxiety
The most robust findings in the current study indicated that greater SCI impairments, and caregiver stress due to those impairments, were associated with higher caregiver depresion and anxiety. These findings are in line with evidence collected in other global regions demonstrating a relationship between physical and psychosocial challenges of individuals with SCI and caregiver mental health (Post, Bloemen, & DeWitte, 2005). However, in the bivariate correlations, only psychosocial functional impairments and the resulting caregiver stress were significantly correlated with caregiver depression and anxiety. Similarly, in the multiple regressions, only psychosocial functional impairments and related caregiver stress were uniquely associated with caregiver depression. These findings together suggest that in Colombia perhaps the SCI impairments most affecting caregiver mental health are related to psychosocial impairments, as opposed to physical impairments. This is in line with findings from a qualitative study in which Latino caregivers described notable distress related to the affective changes and emotional needs of the individual with SCI, while the descriptions of physical care were seen as logistical difficulties (Lucke, Martinez, Mendez, & Arévalo-Flechas, 2013). Additionally, the caregivers in that qualitative study reported that the distress from the change in affect primarily originated from a lack of preparation for dealing with the emotional changes. Considering these previous findings, the origins of the relationships found in the present study may also be due to a lack of preparation regarding psychosocial needs in rehabilitation. This would not be surprising as there are fewer overall rehabilitation services for individuals with an SCI in Latin America, let alone mental health or caregiver services (Burns & O’Connell, 2012).
Burden, Satisfaction with life, and Self-esteem
Interestingly, greater SCI impairments and caregiver stress due to those impairments were not significantly associated with caregiver burden, satisfaction with life, or self-esteem, either in the multiple regressions or the bivariate correlations. In fact, the amount of variance explained in these three variables ranged from 0-7%, which is extremely small and suggests that the lack of statistical significance is not due to the limited sample size used in the current study. Although the findings with burden were surprising and contrary to previous research (Post, Bloeman, & Witte, 2005), greater functional impairments in individuals with SCI—and resulting greater care needs—may not be associated with reduced satisfaction with life and self-esteem in the same way that these variables are in Western cultures. In Latino cultures, providing care for a loved one can offer a tremendous sense of meaning and life satisfaction, as the act of caregiving may fulfill a cultural sense of duty to care for a sick or injured family member (Lucke et al., 2013). Accordingly, these positive effects related to Latino cultural values may account for the non-significant associations in this study.
Clinical Implications
The findings from the current study suggest that SCI caregivers have increased depression and anxiety when the individuals for whom they provide care have higher psychosocial impairments, but not necessarily higher physical impairments. It would benefit rehabilitation professionals to have surveillance methods in place to identify individuals with SCI who are experiencing greater psychosocial impairments and screen their caregivers for mental health needs. A more comprehensive family needs assessment would provide valuable knowledge for clinicians to identify the degree to which specific psychosocial and injury-related educational needs are being fulfilled in the family context. Instruments, such as the Family Needs Questionnaire (FNQ; Meade, Taylor, Kreutzer, Marwitx, & Thomas, 2004) are often used to assess the degree to which needs are being met (e.g., health information needs, community support needs, instrumental support needs, professional support needs, involvement in care needs, and emotional support needs are being met). Namely, a Spanish language version of the FNQ has been constructed, and evidence of validity in Latin America has been demonstrated (Hora & Sousa, 2007). Use of this instrument in a structured family needs assessment may have clinical utility in identifying SCI patients and caregivers in need of psychosocial services throughout the region.
Limitations and Future Directions
While the findings highlight that SCI functional impairments are relevant to caregiver mental health in Colombia, the present study has a variety of limitations. The first was the relatively small sample. Although the nature of this study was exploratory, a larger sample would have provided a clearer picture of the associations between variables. Due to the small sample size and exploratory nature of the study, the authors identified a more sensitive alpha level, which may have resulted in a slightly increased risk of Type-I error although it minimized the risk of Type-II error. A second limitation is that the current study was conducted in one city in Colombia, so caution should be taken when generalizing the findings to other SCI caregiving populations in Latin America. Third, although it is generally assumed that a higher level of impairments in individuals with SCI causes mental health problems in caregivers, the opposite causal direction could be true such that caregivers who are depressed or anxious tend to perceive a higher level of impairment in individuals with SCI than may actually be present. As a result, future research would benefit from clinician reports of SCI impairments or of caregiver mental health.
Future research should focus on constructing empirically supported interventions targeting SCI caregiver mental health needs. Caregivers in American samples have been found to benefit from psychosocial and educational services related to the perceived challenges of caregiving (House, Russell, Kelly, Gerson, & Vogel, 2009), and the current findings highlight a need for future research on similar services in Latin America. Due to the collectivist nature of many Latino cultures (Marin & Marin, 1991), and the importance of family in rehabilitation with Latino populations (Hanson & Kerkhoff, 2007), family support systems may be important variables to consider when constructing these SCI caregiver interventions.
Despite these limitations, the findings from the current study are important, as there is a lack of research exploring the associations between SCI functional impairments and caregiver mental health within this population that is extremely underrepresented in the research literature. The findings supported the hypothesis that SCI psychosocial functional impairments would be associated with caregiver depression and anxiety in Colombia and highlight the need for the development and provision of services for SCI caregivers in this region. If found effective in future research, these caregiver services have the potential to improve caregiver mental health, and perhaps as a result, improve the quality of informal care they are able to provide for individuals with SCI.
REFERENCES
Ackery, A., Tator, C., & Krassioukov, A. (2004). A global perspective on spinal cord injury epidemiology. Journal of Neurotrauma, 21(10), 1355-1370. doi:10.1089/neu.2004.21.1355. [ Links ]
Arango-Lasprilla, J. C., Nicholls, E., Olivera, S. L., Perdomo, J. L., & Arango, J. A. (2010). Healthrelated quality of life in individuals with spinal cord injury in Colombia, South America. NeuroRehabilitation, 27(4), 313-319. doi: 10.3233/ NRE-2010-0614. [ Links ]
Arango-Lasprilla, J. C., Plaza, S. L. O., Drew, A., Romero, J. L. P., Pizarro, J. A. A., Francis, K., & Kreutzer, J. (2010). Family needs and psychosocial functioning of caregivers of individuals with spinal cord injury from Colombia, South America. NeuroRehabilitation, 27(1), 83-93. doi: 10.3233/NRE-2010-0583. [ Links ]
Blanes, L., Carmagnani, M., & Ferreira, L. (2007). Health-related quality of life of primary caregivers of persons with paraplegia. Spinal Cord, 45(6), 399-403. doi:10.1038/sj.sc.3102038. [ Links ]
Boschen, K. A., Tonack, M., & Gargaro, J. (2005). The Impact of Being a Support Provider to a Person Living in the Community With a Spinal Cord Injury. Rehabilitation Psychology; Rehabilitation Psychology, 50(4), 397-407. doi:10.1037/00905550.50.4.397. [ Links ]
Burns, A. S., & Ditunno, J. F. (2001). Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine, 26(24S), S137-S145. [ Links ]
Burns, A. S., & O'Connell, C. (2012). The challenge of spinal cord injury care in the developing world. The Journal of Spinal Cord Medicine, 35(1), 3-8. doi: 10.1179/2045772311Y.0000000043. [ Links ]
Charlifue, S. W., Weitzenkamp, D. A., & Whiteneck, G. G. (1999). Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Archives of Physical Medicine and Rehabilitation, 80(11), 1429-1434. [ Links ]
Chen, H. Y., & Boore, J. R. P. (2008). Living with a spinal cord injury: a grounded theory approach. Journal of Clinical Nursing, 17(5a), 116-124. DOI: 10.1111/j.1365-2702.2007.02117. [ Links ]
Chen, H.Y., Tang, Y., Vogel, L. C., & Devivo, M. J. (2013). Causes of spinal cord injury. Topics in Spinal Cord Injury Rehabilitation, 19(1), 1-8. doi: 10.1310/sci1901-1. [ Links ]
Coleman, J. A., Harper, L. A., Perrin, P. B., Olivera, S. L., Perdomo, J. L., Arango, J. A., & Arango-Lasprilla, J. C. (2013). Examining the relationship between health-related quality of life in individuals with spinal cord injury and the mental health of their caregivers in Colombia, South America. International Journal of Rehabilitation Research. doi: 10.1097/MRR.0b013e3283634e7f. [ Links ]
DeVivo, M. J., & Chen, Y. (2011). Trends in new injuries, prevalent cases, and aging with spinal cord injury. Archives of Physical Medicine and Re-habilitation, 92(3), 332-338. DOI: http://dx.doi.org/10.1016/j.apmr.2010.08.031. [ Links ]
DeVivo, M. J., Krause, S.J., & Lammertse, D. P. (1999). Recent trends in mortality and causes of death among persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 80(11), 1411-1419. [ Links ]
Diez-Quevedo, C., Rangil, T., Sanchez-Planell, L., Kroenke, K., & Spitzer, R. L. (2001). Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic Medicine, 63(4), 679-686. DOI: 10.1097/00006842200107000-00021. [ Links ]
Donlan, W., & Lee, J. (2010). Screening for depression among indigenous Mexican migrant farmworkers using the Patient Health Questionnaire-9. Psychological Reports, 106(2), 419-432. doi: 10.2466/pr0.106.2.419-432. [ Links ]
Elliott T. R., & Rivera, P. (2003). Spinal cord injury. In A. Nezu, C. Nezu, & P. Geller (Eds.) Handbook of Psychology (pp. 415-435). New Jersey: Wiley & Sons, Inc. [ Links ]
Fisher, T. L., Laud, P. W., Byfield, M. G., Brown, T. T., Hayat, M. J., & Fiedler, I. G. (2002). Sexual health after spinal cord injury: a longitudinal study. Archives of Physical Medicine and Rehabilitation, 83(8), 1043-1051. DOI: http://dx.doi.org/10.1053/apmr.2002.33654. [ Links ]
Hanson, S. L., & Kerkhoff, T. R. (2007). Ethical decision making in rehabilitation: Consideration of Latino cultural factors. Rehabilitation Psychology, 52(4), 409-420. doi:10.1037/0090-5550.52.4.409. [ Links ]
Hora, E. C., & Sousa, R. M. C. d. (2009). Crosscultural adaptation of the instrument" Family Needs Questionnaire". Revista Latino-Americana de Enfermagem, 17(4), 541-547. [ Links ]
House, L., Russell, H., Kelly, E., Gerson, A., & Vogel, L. (2009). Rehabilitation and future participation of youth following spinal cord injury: caregiver perspectives. Spinal Cord, 47(12), 882-886. doi:10.1038/sc.2009.64. [ Links ]
Kannisto, M., Merikanto, J., Alaranta, H., Hokkanen, H., & Sintonen, H. (1998). Comparison of health-related quality of life in three subgroups of spinal cord injury patients. Spinal Cord, 36(3), 193-199. [ Links ]
Kemp, B., Krause, J. S., & Adkins, R. (1999). Depression among African Americans, Latinos, and Caucasians with spinal cord injury: A exploratory study. Rehabilitation Psluychology, 44(3), 235-247. [ Links ]
Kennedy, P., Lude, P., & Taylor, N. (2005). Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord, 44(2), 95-105. doi: 10.1038/sj.sc.3101787. [ Links ]
Kennedy, P., & Rogers, B. A. (2000). Anxiety and depression after spinal cord injury: A longitudinal analysis. Archives of Physical Medicine and Rehabilitation, 81(7), 932-937. DOI: http://dx.doi.org/10.1053/apmr.2000.5580. [ Links ]
Krause, J. S., Kewman, D., DeVivo, M. J., Maynard, F., Coker, J., Roach, M. J., & Ducharme, S. (1999). Employment after spinal cord injury: an analysis of cases from the Model Spinal Cord Injury Systems. Archives of Physical Medicine and Rehabilitation, 80(11), 1492-1500. [ Links ]
Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatry Annals, 32(9), 1-7. [ Links ]
Lucke, K. T., Martinez, H., Mendez, T. B., & Arévalo-Flechas, L. C. (2013). Resolving to Go Forward The Experience of Latino/Hispanic Family Caregivers. Qualitative Health Research, 23(2), 218-230. DOI: 10.1177/1049732312468062. [ Links ]
Marin, G., & Marin, B. V. O. (1991). Research with Hispanic populations: Sage Publications, Inc. [ Links ]
Martin-Carrasco, M., Otermin, P., Pérez-Camo, V., Pujol, J., Agüera, L., Martín, M., ... Balañá, M. (2010). EDUCA study: Psychometric properties of the Spanish version of the Zarit Caregiver Burden Scale. Aging & Mental Health, 14(6), 705-11. DOI:10.1080/13607860903586094. [ Links ]
Martínez, C. M. J., Martínez, R. M., García, C. J., Orts-Cortés, M. I., Reig-Ferrer, A., & Tosal-Herrero, B. (2004). Fiabilidad y validez de la Escala de Satisfacción con la Vida de Diener en una muestra de mujeres embarazadas y puérperas. Psicothema, 16(3), 448-455. [ Links ]
McDonald, J. W., & Sadowsky, C. (2002). Spinal-cord injury. The Lancet, 359(9304), 417-425. [ Links ]
McKinley, W. O., Jackson, A. B., Cardenas, D. D., & De Vivo, M. J. (1999). Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Archives of Physical Medicine and Rehabilitation, 80(11), 1402-1410. doi: 10.1016/S0003-9993(99)90251-4. [ Links ]
Middleton, J., Dayton, A., Walsh, J., Rutkowski, S., Leong, G., & Duong, S. (2012). Life expectancy after spinal cord injury: a 50-year study. Spinal Cord, 50(11), 803-811. doi:10.1038/sc.2012.55. [ Links ]
Migliorini, C., Tonge, B., & Taleporos, G. (2008). Spinal cord injury and mental health. Australian and New Zealand Journal of Psychiatry, 42(4), 309-314. [ Links ]
Nicholls, E., Lehan, T., Olivera Plaza, S. L., Deng, X., Perdomo Romero, J. L., Arango Pizarro, J. A., & Arango-Lasprilla, J. C. (2011). Factors influencing acceptance of disability in individuals with spinal cord injury in Neiva, Colombia, South America. Disability and Rehabilitation(00), 1-7. [ Links ]
Novy, D. M., Nelson, D. V., Smith, K. G., Rogers, P. A., & Rowzee, R. D. (1995). Psychometric comparability of the English-and Spanishlanguage versions of the State-Trait Anxiety Inventory. Hispanic Journal of Behavioral Sciences, 17(2), 209-224. [ Links ]
Pavot, W., & Diener, E. (1993). Review of the satisfaction with life scale. Psychological Assessment, 5(2), 164-172. doi:10.1037/1040-3590.5.2.164. [ Links ]
Post, M., Bloemen, J., & De Witte, L. (2005). Burden of support for partners of persons with spinal cord injuries. Spinal Cord, 43(5), 311-319. doi:10.1038/sj.sc.3101704. [ Links ]
Post, M., & van Leeuwen, C. (2012). Psychosocial issues in spinal cord injury: a review. Spinal Cord, 50(5), 382-389. doi: 10.1038/sc.2011.182. [ Links ]
Priebe, M. M., Chiodo, A. E., Scelza, W. M., Kirshblum, S. C., Wuermser, L. A., & Ho, C. H. (2007). Spinal cord injury medicine. 6. Economic and societal issues in spinal cord injury. Archives of Physical Medicine and Rehabilitation, 88(3), S84-S88. DOI: http://dx.doi.org/10.1016/j.apmr.2006.12.005. [ Links ]
Putzke, J. D., Richards, J. S., Hicken, B. L., & DeVivo, M. J. (2002). Predictors of life satisfaction: a spinal cord injury cohort study. Archives of Physical Medicine and Rehabilitation, 83(4), 555-561. [ Links ]
Raj, J., Manigandan, C., & Jacob, K. (2006). Leisure satisfaction and psychiatric morbidity among informal carers of people with spinal cord injury. Spinal Cord, 44(11), 676-679. doi:10.1038/ sj.sc.3101899. [ Links ]
Rosenberg, M. (1965). The measurement of selfesteem. Society and the Adolescent Self-Image, 16-36. [ Links ]
Schmitt, D. P., & Allik, J. (2005). Simultaneous administration of the Rosenberg Self-Esteem Scale in 53 nations: exploring the universal and culture-specific features of global self-esteem. Journal of Personality and Social Psychology, 89(4), 623-642. [ Links ]
Schulz, R., Tompkins, C. A., Wood, D., & Decker, S. (1987). The Social Psychology of Caregiving: Physical and Psychological Costs of Providing Support to the Disabled. Journal of Applied Social Psychology, 17(4), 401-428. [ Links ]
Shewchuk, R. M., Richards, J. S., & Elliott, T. R. (1998). Dynamic processes in health outcomes among caregivers of patients with spinal cord injuries. Health Psychology, 17(2), 125-129. [ Links ]
Spielberger, C. D., & Díaz-Guerrero, R. I. (1975). Inventario de ansiedad: rasgo-estado. México: El Manual Moderno. [ Links ]
Spielberger, C. D., & Gorsuch, R. L. (1983). Statetrait anxiety inventory for adults: sampler set: manual, test, scoring key: Mind Garden. [ Links ]
Strauss, D. J., DeVivo, M. J., Paculdo, D. R., & Shavelle, R. M. (2006). Trends in life expectancy after spinal cord injury. Archives of Physical Medicine and Rehabilitation, 87(8), 1079-1085. DOI: http://dx.doi.org/10.1016/j.apmr.2006.04.022. [ Links ]
Virella, B., Arbona, C., & Novy, D. M. (1994). Psychometric properties and factor structure of the Spanish version of the State-Trait Anxiety Inventory. Journal of Personality Assessment, 63(3), 401-412. [ Links ]
Vissers, M., van den Berg-Emons, R., Sluis, T., Bergen, M., Stam, H., & Bussmann, H. (2008). Barriers to and facilitators of everyday physical activity in persons with a spinal cord injury after discharge from the rehabilitation centre. Journal of Rehabilitation Medicine, 40(6), 461-467. doi: 10.2340/16501977-0191. [ Links ]
Whiteneck, G., Tate, D., & Charlifue, S. (1999). Predicting community reintegration after spinal cord injury from demographic and injury characteristics. Archives of Physical Medicine and Rehabilitation, 80(11), 1485-1491. [ Links ]
Wulsin, L., Somoza, E., & Heck, J. (2002). The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Primary Care Companion to the Journal of Clinical Psychiatry, 4(5), 191-195. [ Links ]
Wyndaele, M., & Wyndaele, J. J. (2006). Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord, 44(9), 523-529. doi:10.1038/sj.sc.3101893. [ Links ]
Zarit, S. H., Reever, K. E., & Bach-Peterson, J. (1980). Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist, 20(6), 649-655. doi: 10.1093/geront/20.6.649. [ Links ]













