Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
TecnoLógicas
versão impressa ISSN 0123-7799versão On-line ISSN 2256-5337
TecnoL. vol.20 no.40 Medellín dez. 2017
Artículo de investigación/Research article
Development and implementation of technologies for physical telerehabilitation in Latin America: a systematic review of literature, programs and projects
Desarrollo e implementación de tecnologías para telerehabilitación física en América Latina: una revisión sistemática de literatura, programas y proyectos
Fabián Narváez1, Diana M Marín-Castrillón2, Ma. Cisne Cuenca3, Ma. Augusta Latta4
1 Electronic Engineer, M.Sc in Biomedical Engineering, PhD in Engineering. Biomedical Engineering - GIIB-UDA Research Group, Electronic Engineering School, Science and Technology Faculty, Universidad del Azuay, Cuenca, Ecuador, frnarvaeze@uazuay.edu.ec
2 Biomedical Engineer, Automatic, Electronic and Computational Sciences Research Group, Engineering Faculty, Instituto Tecnológico Metropolitano, Medellín, Colombia, dianamarin121064@correo.itm.edu.co
3 M.Sc in Biomedical Engineering, Biomedical Engineering - GIIB-UDA Research Group, Electronic Engineering School, Science and Technology Faculty, Universidad del Azuay, Cuenca, Ecuador, mayercs17@gmail.com
4 B.S in Physiotherapy, Health Science Faculty, Physic Teraphy Program, Universidad Técnica de Ambato, Ambato, Ecuador, mariaalatta@uta.edu.ec
Fecha de recepción: 24 de junio de 2017/ Fecha de aceptación: 15 de septiembre de 2017
Como citar / How to cite
F. Narváez, D:M Marín-Castrillón, M.C. Cuenca y M.A. Latta. Development and Implementation of Technologies for Physical Telerehabilitation in Latin America: a systematic review of literature, programs and projects. TecnoLógicas, vol. 20, no. 40, pp. 155-176, 2017.
Abstract
Telerehabilitation has arised by the inclusion of emerging technologies for capturing, transmitting, analyzing and visualizing movement patterns associated to musculoskeletal disorders. This therapeutic strategy enables to carry out diagnosis processes and provide rehabilitation treatments. This paper presents a systematic review of the current development and implementation of telerehabilitation technologies in Latin America. The main goal is to explore the scientific literature and dissemination sources to establish if such technologies have been introduced in this region. Likewise, this work highlights existing prototypes or systems that are to being used or that are still under development. A systematic search strategy was conducted by two different searches: the first one involves a rigorous literature search from the most relevant scientific digital repositories; the second one included telerehabilitation projects and programs retrieved by an advanced Google search. A total of 53 documents from six countries (Colombia, Brazil, Mexico, Ecuador, Chile and Argentina) were found. Most of them were focused on academic and research initiatives to develop in-home telerehabilitation technologies for pediatric and elderly populations affected by motor and functional impairment, cerebral palsy, neurocognitive disorders and stroke. The analysis of the findings revealed the need for a comprehensive approach that integrates health care and the social system to increase the current availability of telerehabilitation initiatives in Latin America.
Keywords: physical telerehabilitation, emerging technologies, review, Latin America.
Resumen
La telerehabilitation ha surgido debido a la inclusión de tecnologías emergentes para la captura, transmisión, análisis y visualización de patrones de movimiento asociados a pacientes con trastornos músculo-esqueléticos. Esta estrategia permite llevar a cabo procesos de diagnóstico y tratamientos de rehabilitación a distancia. Este artículo presenta una revisión sistemática del desarrollo e implementación actual de las tecnologías de telerehabilitación en la región latinoamericana. El objetivo principal es explorar, a partir de la literatura científica reportada y fuentes divulgativas, si las tecnologías de telerehabilitación han logrado ser introducidas en esta región. Asimismo, este trabajo revela los prototipos actuales o sistemas que están en desarrollo o que ya están siendo usados. Se llevó a cabo una revisión sistemática, mediante dos búsquedas diferentes. La primera implicó una búsqueda bibliográfica rigurosa en los repositorios digitales científicos más relevantes en el área y la segunda incluyó proyectos y programas de telerehabilitación implementados en la región, encontrados a partir de una búsqueda avanzada en Google. Se encontró un total de 53 documentos de seis países (Colombia, Brasil, México, Ecuador, Chile y Argentina); la mayoría de ellos estaban enfocados en iniciativas académicas y de investigación para el desarrollo de prototipos tecnológicos para telerehabilitación de pacientes pediátricos y adultos mayores, afectados por deficiencias motoras o funcionales, parálisis cerebral, enfermedades neurocognitivas y accidente cerebrovascular. El análisis de estos documentos reveló la necesidad de un extenso enfoque integrado de salud y sistema social para aumentar la disponibilidad actual de iniciativas de telerehabilitación en la región latinoamericana.
Palabras clave: telerehabilitación Física, tecnologías emergentes, revisión, Latinoamérica.
1. Introduction
According to the World Health Organization, at least 15% of the world population could present musculoskeletal disabilities [1]. They may be caused by different factors such as a constant aging population, congenital disorders and survival to neurological diseases and trauma, leaving physical sequels to be rehabilitated [2]. From these groups, it is estimated that between 76% and 85% of subjects do not have access to rehabilitation programs [1]. In Latin American countries, previous reports have estimated that between 6% and 31% of the population is affected by some type of functional disability [3], but only 3% of those who require rehabilitation services have access to them [3], [4]. Although these countries have earmarked important economic resources to meet the increasing demand by providing efficient health services, approximately 6.8% of their Gross Domestic Product (GDP)., they still presented a huge deficit to provide these services [5]. In addition, according to 2010 data [6], disability rates range from 5.1% in Mexico to 23.9% in Brazil, whereas in the Caribbean the proportion varies between 2.9% in the Bahamas and 6.9% in Aruba. That is to say, almost 12% of the Latin American population is estimated to live with at least one disability; this represents around 85 million people, but only 2% has access to a suitable rehabilitation program. However, it has been estimated that the statistics may remain steady due to the constant aging of the population, the increase in the occurrence of catastrophic diseases and physical traumas. These factors have encouraged the development of novel strategies, procedures and systems related to healthcare services provision whose main purpose is to maintain or improve the functional mobility and independence, facilitate the patient’s social inclusion and enhance the overall wellness and quality of life [7].
In the area of physiotherapy, the use of telemonitoring technologies has been proposed as an alternative for providing affordable functional rehabilitation services and reducing hospital overloads, thus removing some space-time constraints [8], [9]. A retrospective study with 155 patients and 155 control subjects shown that the costs of hospital bed days of care (1,449 days) in the year before the implementation of telerehabilitation programs totaled approximately $1,500,000, which decreased more than around $804,000 the year following the implementation of the telerehabilitation program, which represents a 46% decrease in costs and a decrease of 826 days of care [10]. Likewise, primary care and geriatric visits decreased by over 100 during that year. On the other hand, in some countries in Latin America physical rehabilitation programs are provided to social security beneficiaries (65%), private health care plan members (30%) and as private health services (5%) [11]. However, access to public health systems is not free in most Latin American countries and, therefore, patients need private health services with variable costs, including some related to mobility and personalized assistance. Besides, the charges depend on the cost of living in each country, a fact that makes more difficult to estimate constant economic benefits of telerehabilitation. Therefore, the cost effectiveness of telerehabilitation programs has been evaluated for a specific disability, as described in [8]-[10], [12]. Thus, telerehabilitation is still considered a growing alternative to traditional face-to-face therapy that employs technological solutions to remotely provide rehabilitation care in both clinical centers and in-home programs. This strategy should not be seen as a technology itself, but as the use of new emerging technologies—such as motion capture sensors, wearable devices and computational tools, among others—to provide healthcare assistance to patients in their own home or residence, which reduces high costs and discomfort due to long patient transportation [13]. Consequently, telerehabilitation systems or programs are developed to cover the high demand of disabled people with different types of physical impairments in developed and high-income countries are reported in different sources of scientific and dissemination literature.
This paper presents a systematic review of the current development and implementation of telerehabilitation technologies in Latin American countries. The main goal is to explore from reported scientific literature and informative sources to establish if rehabilitation technologies have been introduced in this region. Likewise, this work expects to describe current prototypes or systems that are being used or still under development, which are not yet reported in scientific literature.
2. Overview of technologies for telerehabilitation
Telerehabilitation is comprised of a set of instruments and protocols aimed at providing access to rehabilitation services to patients at geographically distant locations [13]. Previous works have reported some important benefits for patients in specific rehabilitation programs that use information and communication technologies. The outcomes are comparable to those obtained by the well-known face-to-face physiotherapy [14]-[17]. Since telerehabilitation systems are used in real clinical scenarios, several assistive technologies have been implemented using basic communication tools, e.g., healthcare assistance by videoconference [18]. Because of technological advances, more sophisticated methods were introduced into rehabilitation processes [19]. Thus, the principal aim is to include low-cost technologies to improve and optimize the rehabilitation service and patient outcomes by reinforcing traditional rehabilitation programs and providing applicability and portability at home. Most rehabilitation technologies are customized to personal practices [20], which suggests reduced applicability in other rehabilitation practices. In fact, some clinical studies reveal that only 31% of the patients actually follow home exercise routine such as prescribed by therapists [21]. Currently, home rehabilitation protocols are addressed to those patients in a game context, thus maintaining the effectiveness of cognitively challenging exercises [22]. For that reason, telerehabilitation systems based on motion capture have been shown to increase the intensity of rehabilitation sessions and improve the user’s experience [23], [24]. These systems have encouraged the use of different kinds of commercial sensor technologies for capturing, storing, analyzing and processing movement information related to orientation and position of different body segments (limbs) of patients from which both video and spatiotemporal signals are acquired [21], [25]. Therefore, different assistive technologies have been implemented in telerehabilitation systems and resulted in the emergence of some disciplines, such as the following:
2.1 Virtual environments and serious games (exergames)
A virtual interaction between patient-to-clinician allows to simulate traditional treatments, being as effective as in-person therapies [26]. Several rehabilitation systems based on low-cost motion tracking technologies have been developed to record the user’s movements in 3D graphic environments with devices, such as Nintendo Wii Remote, Kinect Camera and inertial sensors (Inertial Measurement Units - IMUs) implemented in 3D computer graphic environments [21], [27]. Some research projects have directly explored the potential of current commercial games for rehabilitation. This is the case of commercial console games with motion-based input devices, such as Playstation and Wii Sports, which have been used in real clinical studies [28]-[30]. Their main drawbacks are related to a design that is directed at normal subjects. Other systems [31], [32], inspired by game consoles in the market (Wii, Xbox) have proposed a mixed rehabilitative/gaming use of these commercial devices. Among them, very few studies are devoted to develop exergaming devices customized for rehabilitation [33], [34]. However, not all of them are suitable for home care settings, and none of them can be integrated as a telerehabilitation device. Likewise, virtual environments and virtual reality engines such as Unity 3D, Games Maker Studio, Unreal Engine and Blender toolkits, among others, have been used as development kits for 2D and 3D video games. They enable to simulate real clinical scenarios for both patients and clinicians.
2.2 Robotic-based rehabilitation
Nowadays, low-cost technologies allow different developments of telerehabilitation prototypes, which can be provided in a variety of modes. They include both robotic devices and virtual reality applications for tele-homecare to coordinate in-home therapy and patient support, in-home patient telemonitoring, and teletherapy for exercise recognition and supervision by a remote therapist [22], [35], [36]. Specifically, a therapy robot is used during a rehabilitation program for a certain period of time to increase an individual’s ability to recover the capability of movement [37]. These robots are part of human-machine interactions that are often considered robotic therapy aids to assist disabled patients. They implement simple technologies to be used and managed by patients, engineers, therapists and clinicians. Such is the case of robots based on haptic sensors combined with inertial and depth sensors (Kinect® camera), which enable to estimate measurements such as strength (force), orientation and position of human body segments [38], [39]. These strategies are being used to cover post-surgery movements of human limbs and provide mobility aids based on exoskeletal devices. Usually, the Kinect® cameras provide the position of joints between two adjacent body segments, which are extracted from the human silhouette by processing the depth images obtained from the Kinect® technology [15], [40]. This device uses a skeleton with fifteen or twenty joints, depending on the version, Kinect v1 or v2. Hence, spatial information allows to locate the body segment under evaluation.
On the other hand, the most widely used wearable sensors are of the inertial type, which retrieve information from gyroscopes, accelerometers and magnetometers contained in an IMU unit [41], [42]. This information allows to estimate 3-axis data regarding the orientation of each body segment under analysis. In addition, the clinic movements can be estimated depending on anatomical planes by processing the information about their positions. These devices enable to wirelessly measure joint angles for diagnosis during rehabilitation exercises [43].
Finally, haptic technologies are used to recreate the sense of touch by applying forces, vibrations, or motions to the users [29]. This kind of mechanical stimulations are used to assist in the creation or handling of virtual objects in a graphic environment [44], [45]. Their main advantage is providing biofeedback during a rehabilitation process that can be used to enhance some control systems, mainly when they are included in exoskeletal systems based on motor movements.
3. Methods
3.1 Data sources and search strategys
In this work, a systematic strategy was taken to conduct the review by two different searches. The first one involves a rigorous literature search from some scientific digital repositories and second one includes telerehabilitation projects and programs implemented in Latin American region by both academic and healthcare institutions. Each search is described below.
3.1.1 Searching Scientific Literature
To identify relevant articles focused on telerehabilitation endeavors in Latin American region, a literature search was conducted from different scientific databases such as: Embase, IEEE Xplore, PlosOne, Medline, ScienceDirect, Scopus, Scielo, Redalyc and Google Scholar. This search was related to keywords: "telerehabilitation" OR "tele-rehabilitation" OR "telerehabilitación" OR "tele-rehabilitación" "tele reabilitação" OR "telereabilitação" AND “Motor” OR “Motion” OR “Motriz” OR “Movement” OR “Movimiento” OR “Movimento” AND any name of Latin America countries (Argentina, Bolivia, Brazil, Chile, Colombia, among others). For doing so, refereed journals and peer-reviewed articles published in either conference proceedings or book chapters from January 2011 to May 2017 were taken into account. In addition, only articles written in English, Spanish or Portuguese were included. Hence, the title and abstract of all the retrieved articles were initially reviewed by title and abstract to identify potentially relevant papers.
3.1.2 Searching Telerehabilitation Programs/projects
Several telerehabilitation initiatives have emerged as simple academic prototypes that later transcended as research projects by universities, hospitals and government or private institutions. Their outcomes have allowed to implement different telerehabilitation programs in public health systems in some Latin American countries. However, the technological development of these programs or projects has not always been reported through scientific articles. Therefore, our second search regarding telerehabilitation programs and projects was conducted on Google. For doing so, we used search terms related to telerehabilitation services, programs or projects. Thus, the search terms were combined as follows: ("telerehabilitación" OR "tele-rehabilitación" OR "tele reabilitação" OR "telereabilitação") AND ("Servicio" OR "programa" OR "proyecto" OR "serviço" OR "Projeto" OR "Programa"). The second search strategy aimed to retrieve technical information such as: informative literature, technical reports, websites and informative documents. Those written in Spanish or Portuguese languages due to that we suppose that the most relevant information is disseminated in the native language of each country. This way, informative and technical reports from January 2006 to May 2017 were retrieved. For that purpose, the web domains of each Latin American country were included in the search, e.g., *.co, *.ch, *.ar, *.ec and *.br, among others.
The time period of the search was defined by the release date of video game technologies used for telerehabilitation such as Nintendo WII (2006), Kinect® camera by Microsoft (2010) and exergames development based on WebGL (2011). Likewise, all the titles and abstracts of the retrieved documents were initially reviewed to identify potentially relevant information. Finally, once all the relevant articles and informative documents related to telerehabilitation programs/projects were identified, an inclusion/exclusion process was established based on some criteria, as described below.
3.2 Study selection-inclusion/exclusion criteria
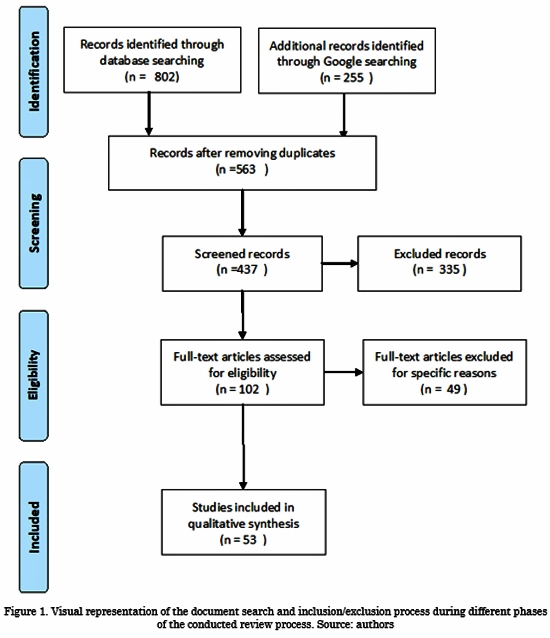
Once the two sets of scientific articles and technical reports on telerehabilitation programs/projects were identified and retrieved (e.g., from digital repositories and websites or documents), a selection process was introduced. The latter was based on the Preferred Reporting Items for Systematic Review and Meta-Analyses - PRISMA statement [46], as illustrated in Fig. 1.
Thus, a preliminary selection task was carried out by removing all duplicate articles or technical reports related to the same telerehabilitation program/project. Then, two groups of inclusion/exclusion criteria were defined: one for the scientific literature and another one for the telerehabilitation programs/projects.
3.2.1 Scientific literature criteria
The selected articles were assessed based on the following screening questions.
Inclusion criteria questions:
1. Is the publication focused on the development or implementation of technologies in physical telerehabilitation?
2. Does the publication describe research or implementation projects carried out in a Latin American country?
3. Was the document published between January 2011 and May 2017?
4. Is the publication a MSc or PhD the-sis?
5. Is the retrieved publication written in English, Spanish or Portuguese?
If the answer was “yes” to all the questions above based on the title and abstract of the selected article, that document was included in an eligibility review. The articles that cast doubt regarding any question were also remained. On the other hand, an exclusion criterion was also defined; it allowed to remove articles with absolute certainty. Likewise, if the review process resulted in “no” answers to all the exclusion question, the article was included. The detailed list of exclusion questions is below.
Exclusion criteria questions:
1. Is the publication focused on the de-velopment or implementation of technolo-gies for other telerehabilitation services (different to motor impairments)?
2. Does the publication describe research or implementation projects that were developed out of Latin American countries?
3. Is the publication a review, a degree project or a text book?
Finally, the review process concludes with an eligibility review stage. During the latter, the full text was read and reviewed to establish if it met some eligibility criteria such as telerehabilitation platform, method-ological evaluations and clinical results.
3.2.2 Projects and Programs criteria
Similarly, the retrieved documents were screened by reviewers to find programs and projects that led to answer “yes” to all the inclusion and exclusion criteria questions below. Since some of those documents were news articles and other unofficial texts, the projects and programs reported by them were followed in order to obtain official information. Then, specific news articles were accepted as official information when the reported data was provided by clearly identified official sources.
Inclusion criteria questions:
1. Is the project or program concerned with developing or implementing physical telerehabilitation services in a Latin American country?
2. Was the program or project devel-oped between January 2007 and May 2017?
Exclusion criteria:
1. Is there any official or technical doc-ument that allows to verify the execution of the program or project?
4. Results
4.1 Database search and selected papers
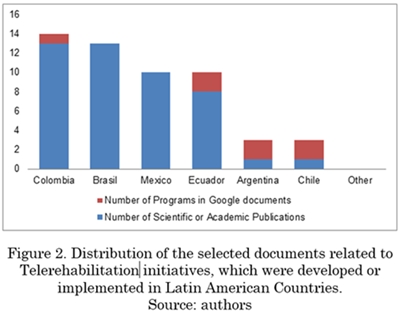
An overview of our obtained results from both scientific literature and telerehabilitation projects/programs searches are shown in Fig. 1. A group of 802 articles and 255 Google documents were initially retrieved by the aforementioned searches. Out of those, only 46 relevant articles and 7 documents related to programs and projects met all the inclusion criteria proposed in this systematic review. A distribution of the selected scientific papers and projects by Latin American region is shown in Fig. 2. It reveals that only six countries have reported any telerehabilitation initiative based on emerging technologies for restoring some motor impairments. As a result, a total of 14 documents were found from Colombia, 13 from Brazil, 10 from Ecuador and 10 from Mexico. Argentina and Chile reported 3 documents each. Additionally, in the particular case of Chile, a set of 8 documents related to telerehabilitation projects developed by Teletón Institute was retrieved. However, those initiatives were summarized and reported in a single relevant document, which is considered in this systematic review.
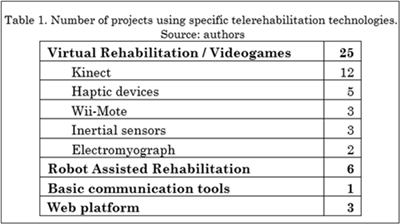
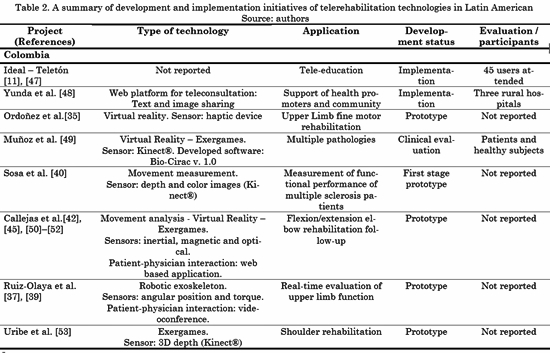
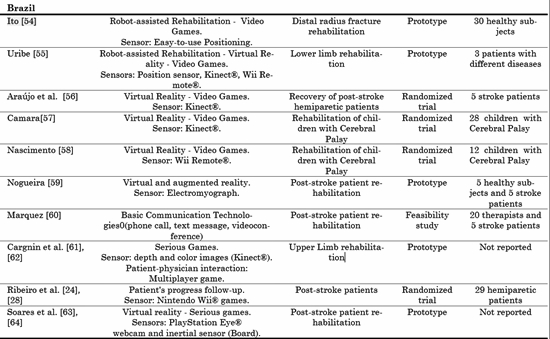
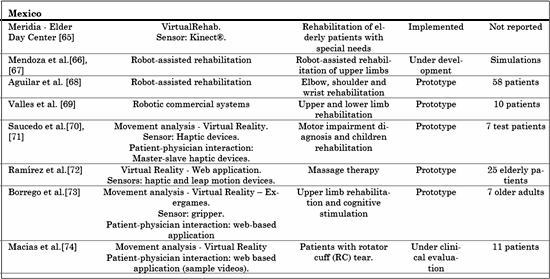
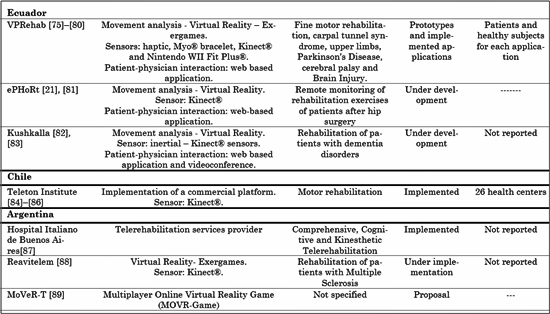
The selected studies were classified by country and project, as the results of our eligibility process. In addition, the review allowed to determine that some documents had been written by the same authors (or some of them) and they were the outcomes of the same projects that also described their use and applied technology. Table 1 presents a summary of the technologies used in those projects. It can be observed that a large number of studies reported the development or use of virtual rehabilitation technologies (25) compared to robot-assisted rehabilitation (6), web platforms (3) and basic communication tools (1). Likewise, the Kinect® depth camera was the most widely used sensor for interacting with virtual environments, which was an expected result because it allows patients to move freely. Furthermore, Table 2 describes the most relevant aspects of the selected studies grouped by projects. It can be seen that a reduced number of the selected studies reported a clinical evaluation of real patients.
4.2 Telerehabilitation related to national Initiatives
Among other countries in Latin America, Colombia, Ecuador, Mexico, Brazil, Argentina and Chile have reported technological developments and innovation of emerging telerehabilitation technologies, processes and services directed at people with disabilities, mobility difficulties and older adults. The details of those initiatives are presented below.
4.2.1 Colombia
In this study, Colombia holds the highest number of scientific or academic documents published in Latin America, which is a sign of the development and/or implementation of telerehabilitation initiatives. Seven telerehabilitation projects were identified from a subset of eleven peer-reviewed documents and one rehabilitation program. The program was executed as a cooperation agreement between Teletón and a non-profit organization, Fundación IDEAL [11], [47]. It consisted of an educational process for rehabilitation promoters, disabled people, their families and caregivers. In addition, this initiative was implemented in the Amazonian region. According to Teletón, from 2015 to 2016, 45 users were assisted using this initiative; this number is due to the fact that they faced some problems, such as the internet connection [11]. Besides, the analysis of the documents from that country revealed only one peer-reviewed document that reported a real telerehabilitation implementation in a clinical scenario [48]. Such work comprises a teleconsultation platform for both health promoters and people from a specific community to assist patients who have trouble getting to a medical center. Likewise, most of the other selected documents reported the use of virtual reality combined with low-cost technologies for motion capture based on devices such as inertial and magnetic sensors [42], [45], [50]-[52], Kinect® cameras [40], [53] and haptic devices [35]. These emerging technologies were used for motion tracking and measuring joint angles in order to track the progress of patients with disabilities caused by multiple sclerosis [20] and upper limb motor disabilities during rehabilitation programs [42], [45], [50]-[52], [53], [35], [37], [39].
Colombia also reported the use of exergaming technologies (serious games) as telerehabilitation initiatives for improving user experience [35], [45], [53]. A remarkable telerehabilitation system was developed by Callejas et al. .[42], [45], [50]-[52] for people with upper limb motor disabilities. Their system includes a sensor module to capture motion information by using an optical device and three inertial sensors located on each arm joint. The information is wirelessly sent to a receiver module installed on the health professional's computer to analyze the movements related to a patient’s progress and match them with a therapeutic plan based on video games. Another well-known technology is also adapted in Colombia: robotic-based assistance. Some selected documents presented the use of a teleoperated exoskeleton composed of torque and angular position sensors controlled in real time via Ethernet [37], [39].
4.2.2 Brazil
In Brazil, two types of telerehabilitation have been proposed and both use low-cost technologies. One of them aims to conduct randomized trials and the other one at providing remote rehabilitation. Randomized trials are used to evaluate the efficacy of virtual reality scenarios and exergaming technologies in rehabilitation sessions. Such technologies are implemented using commercial controller devices, such as the Wii Remote® [28], [58] and Kinect® [56], [57]. These works aim to improve the physical functions of Cerebral Palsy [57], [58] and stroke [28], [56] patients. In general, those studies have shown that Virtual Reality contributes to motor damage recovery and follow up. In contrast, the study by do Nascimento [58] revealed that virtual reality was not useful to improve the upper limb function of children with cerebral palsy. Additionally, in 2014, Marques M. [60] carried out a study to demonstrate the feasibility of using conventional technologies such as phone calls, text messages and videoconferences to support the physical rehabilitation process in remote areas. According to her results, both therapists and patients reported satisfaction when they use the proposed technologies and feasibility during the rehabilitation process. In terms of developed technologies, most of those systems aim to support the physical rehabilitation through some virtual rehabilitation applications, which are based on serious games (exergames). Like in other countries in Latin America, those systems propose to use different low-cost devices such as Kinect® [59], [61], [62], Nintendo Wii® [24], [28], balance board [64] and PlayStation EYE® webcam [63], among others. Those initiatives allowed to provide therapeutic treatments for hemiparetic stroke [24], [28], [63], [64] and upper limb disabilities [61], [62]. Although those works indicate the potential of the proposed technologies for performing home rehabilitation therapies, none of them includes an e-health platform designed to provide remote rehabilitation services. In contrast, Dornellas et al. [61] described an innovative strategy based on a virtual world for a multiplayer game that establishes an efficient interaction between the patient and the physical therapist. In addition, the therapist can accurately evaluate and monitor the joint angles and position of the patient by means of a skeleton representation in a graphic interface in real time. Additionally, a novel stabilometry system based on serious games was proposed. It uses a balance board with an inertial sensor unit (accelerometer and gyroscope sensor) for training and evaluating the balance of hemiparetic stroke patients [64]. This work shows a low-cost rehabilitation initiative that employs simple hardware according to specific requirements. Furthermore, two documents reported the development of low-cost mechatronic systems integrated with virtual games to simulate rehabilitation routines [54], [55]. In those cases, the systems were developed as a complement to rehabilitation and not as a replacement of the physical contact between patient and therapist. One relevant aspect of Brazilian initiatives is that most of them were evaluated using real patients. For instance, the usability of serious games proposed for upper limb rehabilitation was evaluated by 48 subjects [61], [62]. Besides, the feasibility of a virtual reality strategy was also evaluated by using 43 post-stroke hemiparetic subjects [24], [28].
4.2.3 México
Currently, Mexico is promoting the development of virtual rehabilitation combined with robotic-based technologies for improving rehabilitation sessions. Hence, several scientific and academic documents in this review correspond to initiatives developed in Mexican healthcare institutions. One project aimed at adopting commercial solutions was also identified. Those commercial solutions are based on controllers to provide robot-assisted rehabilitation for upper limbs [66], [67] and mechatronic devices for arm, elbow, wrist and shoulders rehabilitation, respectively [68]. In addition, an assistive technology based on robotic-rehabilitation was implemented by using commercial devices: The Gymnasium for Robotic Rehabilitation (Robot Gym). In general terms, those commercial devices have proven to be a cost- and labor-efficient alternative for post-stroke rehabilitation compared to standard time-matched rehabilitation sessions [69]. Also, Mexican researchers have shown great interest in the development of rehabilitation systems based on virtual reality. Saucedo et al. proposed to use two haptic devices to perform pediatric motor rehabilitation in a virtual world by applying computer graphics. To do so, a master-slave communication between the two devices allows the therapist to guide the patient to perform some proposed activities [70], [71]. Likewise, haptic and Leap Motion® devices connected to virtual non-immersive environments were proposed for managing online programs of back massage therapy [72]. Another initiative by Borrego et al. [73] involved a collaborative game for motor telerehabilitation. In this sense, a therapy session for two patients is adapted as a game, thus enabling the patients to play simultaneously while the therapist can remotely analyze and monitor their movements.
Another telerehabilitation platform designed for patients with partial rotator cuff tear was reported in this review. Such platform is an interactive environment that provides patients with access to a set of rehabilitation resources, such as education on the pathology, injury care, joint hygiene, activity modification and therapeutic exercises. This platform is currently undergoing clinical trials [74]. Finally, we found some news about the implementation of VirtualRehab, a commercial Kinect®-based platform for physical therapy supported by exergames. This platform is being used at an adult day care center, namely Meridia [65]. However, technical reports with implementation details or results were not found.
4.2.4 Ecuador
In Ecuador, three official projects were identified among eleven retrieved documents (10 selected papers and one official research project). VPRehab (Desarrollo de un demostrador tecnológico en pacientes con daño cerebral adquirido) is a project developed by researchers from ESPE (the Army University) and Zaragoza University in Ecuador and Spain, respectively. It was designed as a rehabilitation system based on virtual reality that can be used to carry out in-home rehabilitation programs. Even though its main purpose was focused on the rehabilitation of disorders caused by acquired brain injury, the selected reports show that it has been used for providing remote rehabilitation assistance to patients with chronic acquired brain injury [76], Parkinson’s disease [75], cerebral palsy [77], stroke [78], carpal tunnel syndrome [79] and upper limbs disabilities [80]. To do so, this project included low-cost devices for motion capture that interact with Kinect® cameras, Nintendo Wii Fit Plus®, MyO® armband, a haptic device and a robot ball. The movement is simulated in virtual environments under the exergaming philosophy (serious games). In all cases, the evaluation was conducted using real patients and healthy subjects, but its use in real clinical scenarios or health-care services was not reported. The second project, named ePHoRt, is an ongoing project proposed by Ecuadorian and Portuguese researchers. It aims to develop a web-based platform for in-home motor rehabilitation of patients after hip arthroplasty surgery. The proposed platform will include motion capture and tracking, movement recognition and assessment, exergames, biofeedback and message-based communication modules [21], [81]. Some preliminary outcomes related to motion capture and movement recognition tasks are reported in [81]. Likewise, Kushkalla [83] is a web-based telerehabilitation platform developed as part of the project Plataforma de telerehabilitación para adultos mayores con trastornos asociados a demencia, basada en tecnologías emergentes [82]. This platform includes a virtual environment to provide user-clinician interaction, a motion capture system and graphic elements for quantitative movement analysis during in-home rehabilitation treatments. To do so, they proposed a gait analysis strategy based on information fusion from inertial sensors and depth image data. In addition, this project will develop some educational plans for caregivers in order to train them on the correct use of the developed technologies.
4.2.5 Chile
Unlike other countries in the region, only one scientific paper was found form Chile: a technologic development. In contrast, the number of implemented cases identified in our search was significant. Moreover, the only paper we found concerns one of those implementation cases [84]. Those initiatives have mainly been developed by Instituto Teletón, a non-profit entity responsible for the comprehensive rehabilitation of children with neuromusculoskeletal damage. For that purpose, Teletón entered an agreement with Virtual Ware (http://virtualwaregroup.com/es) for using VirtualRehab (a virtual rehabilitation system based on exergames and Kinect® interaction) and providing telerehabilitation services in several municipalities of this country [85]. Two main programs are currently being implemented by this Foundation: Teletón en tu comuna and Teletón en casa. The first one is developed under a specific agreement with the local governments. It aims to equip local health care centers with Virtual Rehab technology for providing some comprehensive rehabilitation programs, which are monitored by specialists located at regional Teletón institutes. The second one, Teletón en tu casa, uses more affordable technologies such as personal computers and tablets; hence, patients receive personalized exercise recommendations by therapists. It is carried out using text messages and videoconference sessions [86]. There were no statistical reports about patients treated with this rehabilitation strategy and this program is not currently available. However, Teletón reports that 26 communities will benefit from those programs until 2017.
4.2.6 Argentina
In this country two telerehabilitation projects associated with healthcare institutions were found. They provide specific rehabilitation therapies by using virtual rehabilitation technologies. Hospital Italiano de Buenos Aires offers comprehensive, cognitive and kinesthetic telerehabilitation services for adults and children [87]. This Institution has a health informatics department that is developing several telemedicine projects; among them, there is a graphic application that enables some rehabilitation exercises at the patient's home (telerehabilitation) by using motion sensors [90]. In addition, Instituto de Neurociencias de Buenos Aires (INEBA) is developing a program that aims to evaluate the feasibility of virtual reality and telerehabilitation technologies for neurorehabilitation therapies of patients with multiple sclerosis. To do so, a group of partner healthcare centers will be provided by VirtualRehab, the same application used in Chile by Instituto Teletón. The project purposed to recruit 100 patients from ten neurorehabilitation centers located around the country [88]. Finally, another project was reported in [89]: a virtual rehabilitation system. This project is focused on the development of multiplayer online games with two interconnected applications: a patient-oriented component that is executable on virtual reality glasses and a program that enables physicians to arrange and follow up on therapy sessions from a remote rehabilitation center.
5. Discussion
The proposed systematic review revealed that physical rehabilitation based on telerehabilitation systems has received some attention from both academic and healthcare institutions. The retrieved literature (n=53) is focused on technological developments to assist the most relevant impairments, such as fine motor rehabilitation, upper limb joint injuries, movement disorders caused by cerebral palsy, multiple sclerosis, chronic acquired brain injury, Parkinson’s disease. Besides some documents deal with exercise programs for post-stroke patients. Most of these rehabilitation programs have included low-cost technologies for body movement analysis, measurement and exercise program monitoring. Technologies such as inertial and haptic sensors, Kinect® cameras, Nintendo Wii Fit Plus®, virtual reality, graphic environments and more have been established as fundamental tools for telerehabilitation systems in many clinical scenarios in industrialized countries [91]. Although in Latin America they are used for the same purposes, the reviewed literature shows that the initiatives in this region lack rigorous clinical evaluation. Perhaps this is due to the fact that several telerehabilitation initiatives retrieved in this study have emerged as technological developments more than real clinic applications. In contrast to reports from other regions around the world [9], [10], [12], our findings demonstrate that in Latin America there are no previous studies of economic and assistive benefits regarding these kind of assistive technologies used by either government or private health care systems to provide rehabilitation services. Therefore, a huge multidisciplinary effort by clinicians and researchers is necessary to validate—from the clinical and economic point of view—the profitability of assistive technologies used in remote urban areas in each country in this region.
Our systematic review also revealed that some Latin American countries have started the clinic implementation of low-cost technologies to create telerehabilitation programs and projects. In some instances, regional developments were found to be supported by working in partnership with the local government or commercial institutions [65], [85]. Based on the country-level findings and an overall review of all scientific papers and dissemination documents on telerehabilitation programs/projects gathered for this systematic review, it can be said that a set of telerehabilitation initiatives is currently being implemented in Latin America. Moreover, a few of them have reported their benefits and advantages or disadvantages to be aware of their existence and clinical benefits. Colombia, Mexico and Ecuador have reported the greatest amount of telerehabilitation initiatives as academic developments, but a reduced number of clinical implementations were identified. Conversely, Chile and Argentina reported few academic initiatives, but they have some clinical implementations of telerehabilitation programs, as shown in Table 1. These clinical implementations have been supported by some cooperation agreements between the local health care provider and foreign institutions.
Even though Colombia and Mexico have directed their efforts to adapt different low-cost technologies to clinical scenarios, few programs were clinically evaluated with real patients. For instance, in Colombia, the reported initiatives lack rigorous evaluation. [11] reported a tele-education strategy, but it was evaluated using 45 users. In [48], a web platform for teleconsulting was proposed and evaluated during two months at three rural hospitals. However, only six teleconsultations were carried out. Similarly, in Mexico, robot-assisted rehabilitation combined with exergaming strategies is of great interest; however, the reported evaluation is not exhaustive, as observed in Table 1. Finally, in Brazil and Chile, the retrieved literature has shown that their rehabilitation strategies also lack thorough clinical evaluation. This review reveals that in all Latin American countries the emerging technologies have been well-adopted to support physical rehabilitation without being limited to a specific disability. Nevertheless, clinical protocols must be introduced to evaluate and establish the disadvantages, advantages and benefits of the implementation of this kind of alternative rehabilitation programs in different rehabilitation fields. Therefore, in Latin America, telerehabilitation still is a growing research area that offers opportunities for further formalizing methods from a clinical point of view.
Another observation based on the review is that the telerehabilitation programs currently available in the region were partially or fully supported by or working in partnership with the government or foreign companies focused on this task [85].
Additionally, it is important to highlight that telerehabilitation programs are likely to be accepted by the Latin American population, which was evidenced in the review. The growing social acceptability of telerehabilitation programs contributes to the usability of emerging technologies. In other words, the users are more likely to adopt them. In addition, telerehabilitation needs to be seen differently—as a set of highly useful technological strategies that aids many populations with existing impairments and disabilities and prevents severe health problems.
6. Conclusions and recommendations
Physical rehabilitation based on emerging technologies for impaired populations has received some attention in Latin America. Specifically, the telerehabilitation programs and projects under development are related to disabilities caused by pediatric motor impairment, cerebral palsy, stroke, neurocognitive disorders and functional movement rehabilitation. Nevertheless, a strong effort is being made to provide rehabilitation programs for the elderly population, who inevitably are at a high impairment and disability risk as a result of ageing. For instance, Colombia, Mexico and Ecuador have reported the greatest amount of telerehabilitation initiatives based on virtual reality combined with wearable sensors such as haptic, inertial, torque and Kinect® sensors that adopt the philosophy of exergaming and assistive robotics. However, a reduced number of clinical validations was identified. In contrast, Chile and Argentina have reported few academic initiatives, but they presented some clinical implementations of telerehabilitation programs supported by cooperation agreements between local health care providers and foreign institutions. Finally, regarding Brazil and Chile, the retrieved literature has shown that their rehabilitation strategies also lack thorough clinical evaluation. However, more systematic planning and efforts are required to design, produce and ensure the availability of affordable, acceptable, accessible and adaptable telerehabilitation programs to assist disabled population in general terms. In addition, economic support from health care institutions or government policies is essential to establish standardized clinical protocols for validating and evaluating the technology in real clinical scenarios. Furthermore, national enabling legislation is necessary in each of the six reviewed countries to implement these strategies in a safe and reliable way for users and clinicians. The analysis of the results from the six Latin American countries also suggests the need for a comprehensive, integrated health and social system approach to increase the current availability of telerehabilitation initiatives for disabled population in this region.
Such approach would entail several tasks: promoting initiatives for low-cost telerehabilitation programs; raising awareness and building capacity on emerging technologies; bridging the gap between rehabilitation policy and practice in a remote manner; and fostering targeted research on telerehabilitation based on emerging technologies.
7. Acknowledgments
This work was partially funded by the Ecuadorian Consortium for Advanced Internet Development (CEDIA) through the CEPRA projects. Specifically, under grants CEPRA-X-2016 project; "Telerehabilitation platform for elderly with dementia disorders, based on emerging technologies". [Grant number: X-2016-02].
Referencias
[1] OMS, “Informe mundial sobre la discapacidad,” World Health Organization, 2011. [ Links ]
[2] M. F. Stang Alva, Las personas con discapacidad en america Latina: del reconocimiento juridico a la desigualdad real. 2011. [ Links ]
[3] A. Vásquez, “La discapacidad en América Latina,” Discapacidad. Lo que todos debemos saber, Organ. Panam. la Salud, 2006. [ Links ]
[4] F. Caravaca, B. Gonzales, M. Á. Bayo, and E. Luna, “Dolor músculo-esquelético en pacientes con enfermedad renal crónica,” Nefrología, vol. 36, no. 4, pp. 433-440, Jul. 2016. [ Links ]
[5] N. Heredia, “El derecho a la salud: ¿cuál es el modelo para América Latina?,” MEDICC Rev., vol. 17, no. 14, pp. 16-18, 2015. [ Links ]
[6] S. Schkolnik, “América Latina: la medición de la discapacidad a partir de los censos y fuentes alternativas,” in Los censos de 2010 y la salud: informe del seminario-taller, CEPAL, Ed. 2010. [ Links ]
[7] L. O. M. de Andrade, A. Pellegrini-Filho, O. Solar, F. Rígoli, L. M. de Salazar, P.C. Florit-Serrate, K. Gomes-Ribeiro, T. Swift-Koller, F. N. Bravo-Cruz, R. Atun,, “Determinantes sociales de salud, cobertura universal de salud y desarrollo sostenible: estudios de caso en países latinoamericanos,” in MEDICC Review, vol. 17, no. 1, 2015, pp. s53--s61. [ Links ]
[8] D. Hailey, R. Roine, A. Ohinmaa, and L. Dennett, “Evidence of benefit from telerehabilitation in routine care: a systematic review,” J. Telemed. Telecare, vol. 17, no. 6, pp. 281-287, Sep. 2011. [ Links ]
[9] M. Tousignant, H. Moffet, S. Nadeau, C. Mérette, P. Boissy, H. Corriveau, F. Marquis, F. Cabana, P. Ranger, É. L. Belzile, and R. Dimentberg, “Cost Analysis of In-Home Telerehabilitation for Post-Knee Arthroplasty,” J. Med. Internet Res., vol. 17, no. 3, p. e83, Mar. 2015. [ Links ]
[10] R. M. Bendixen, C. E. Levy, E. S. Olive, R. F. Kobb, and W. C. Mann, “Cost Effectiveness of a Telerehabilitation Program to Support Chronically Ill and Disabled Elders in Their Homes,” Telemed. e-Health, vol. 15, no. 1, pp. 31-38, 2009. [ Links ]
[11] “Informe de Gestión Fundación Teletón 2016,” 2016. [ Links ]
[12] S. Dhurjaty, “The Economics of Telerehabilitation,” Telemed. J. e-Health, vol. 10, no. 2, pp. 196-199, Jun. 2004. [ Links ]
[13] A. Peretti, F. Amenta, S. K. Tayebati, G. Nittari, and S. S. Mahdi, “Telerehabilitation: Review of the State-of-the-Art and Areas of Application,” JMIR Rehabil. Assist. Technol., vol. 4, no. 2, p. e7, Jul. 2017. [ Links ]
[14] R. Salviola, “Effect of a Telemonitoring Intervention on Health Outcomes Among Patients at Risk for Progression of Heart Disease,” A.T. Still University, 2016. [ Links ]
[15] D. Antón, A. Goñi, and A. Illarramendi, “Exercise Recognition for Kinect-based Telerehabilitation,” Methods Inf. Med., vol. 54, no. 2, pp. 145-155, Oct. 2014. [ Links ]
[16] J. Rodiz Cuevas, E. Lopez Dominguez, and Y. Hernandez Velazquez, “Telemonitoring System for Patients with Chronic Kidney Disease Undergoing Peritoneal Dialysis,” IEEE Lat. Am. Trans., vol. 14, no. 4, pp. 2000-2006, 2016. [ Links ]
[17] L. J. V. Escobar and S. A. Salinas, “e-Health prototype system for cardiac telemonitoring,” in 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 2016, pp. 4399-4402. [ Links ]
[18] S. Lovo Grona, B. Bath, A. Busch, T. Rotter, C. Trask, and E. Harrison, “Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review,” J. Telemed. Telecare, p. 1357633X1770078, 2017. [ Links ]
[19] D. M. Brennan, P. S. Lum, G. Uswatte, E. Taub, B. M. Gilmore, and J. Barman, “A telerehabilitation platform for home-based automated therapy of arm function,” in 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2011, pp. 1819-1822. [ Links ]
[20] J. Gutierrez-Martinez and A. Ortiz-Espinosa, “System to measure the range of motion of the joints of the human hand,” Rev. Investig. Clin., vol. 66, pp. 122-130, 2014. [ Links ]
[21] Y. Rybarczyk, J. K. Deters, A. A. Gonzalvo, M. Gonzalez, S. Villarreal, and D. Esparza, “ePHoRt Project: A Web-Based Platform for Home Motor Rehabilitation,” in World Conference on, Springer, Cham, 2017, pp. 609-618. [ Links ]
[22] C. Rodriguez-de-Pablo, S. Balasubramanian, A. Savic, T. D. Tomic, L. Konstantinovic, and T. Keller, “Validating ArmAssist Assessment as outcome measure in upper-limb post-stroke telerehabilitation,” in 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 2015, pp. 4623-4626. [ Links ]
[23] A. Briseño-Cerón, O. Domínguez-Ugalde, and I. Saucedo-Ugalde, “El uso de captura de movimiento corporal para el análisis de discapacidades en miembros superior o inferior: Caso de uso: hemiplejia,” Rev. Int. Tecnol. Cienc. y Soc., vol. 1, no. 2, Jun. 2012. [ Links ]
[24] E. Pedreira da Fonseca, N. M. Ribeiro da Silva, and E. B. Pinto, “Therapeutic Effect of Virtual Reality on Post-Stroke Patients: Randomized Clinical Trial,” J. Stroke Cerebrovasc. Dis., vol. 26, no. 1, pp. 94-100, 2017. [ Links ]
[25] M. Callejas Cuervo, G. M. Díaz, and A. F. Ruíz-Olaya, “Integration of emerging motion capture technologies and videogames for human upper-limb telerehabilitation: A systematic review,” Dyna, vol. 82, no. 189, pp. 68-75, Feb. 2015. [ Links ]
[26] P. F. Monserrat, F. Llull, M. M. Aguilo, J. S. Terrasa, and Y. Gonzalez-Cid, “P4H: An example of successful use of serious games in telerehabilitation,” in 2015 Internet Technologies and Applications (ITA), 2015, pp. 261-265. [ Links ]
[27] D. Anton, A. Goni, A. Illarramendi, J. J. Torres-Unda, and J. Seco, “KiReS: A Kinect-based telerehabilitation system,” in 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013), 2013, no. Healthcom, pp. 444-448. [ Links ]
[28] N. M. da Silva Ribeiro, D. D. Ferraz, É. Pedreira, Í. Pinheiro, A. C. da Silva Pinto, M. G. Neto, L. R. A. dos Santos, M. G. G. Pozzato, R. S. Pinho, and M. R. Masruha, “Virtual rehabilitation via Nintendo Wii®and conventional physical therapy effectively treat post-stroke hemiparetic patients,” Top. Stroke Rehabil., vol. 22, no. 4, pp. 299-305, 2015. [ Links ]
[29] B. Lange, S. Koenig, C.-Y. Chang, E. McConnell, E. Suma, M. Bolas, and A. Rizzo, “Designing informed game-based rehabilitation tasks leveraging advances in virtual reality,” Disabil. Rehabil., vol. 34, no. 22, pp. 1863-1870, Nov. 2012. [ Links ]
[30] A. Nayak, “A pilot study: Effect of a novel dual-task treadmill walking program on balance, mobility, gaze and cognition in community dwelling older adults,” University of Manitoba, 2015. [ Links ]
[31] J. B. H. Gutiérrez, “Efecto de un programa de rehabilitación virtual con Nintendo Wii Balance Board®en un grupo de pacientes de lesión medular establecida en la Clínica Universidad de La Sabana: Un estudio piloto,” Universidad de la Sabana, 2013. [ Links ]
[32] G. C. Burdea, A. Jain, B. Rabin, R. Pellosie, and M. Golomb, “Long-term hand tele-rehabilitation on the playstation 3: Benefits and challenges,” in 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2011, pp. 1835-1838. [ Links ]
[33] K. E. Laver, S. George, S. Thomas, J. E. Deutsch, and M. Crotty, “Virtual reality for stroke rehabilitation,” in Cochrane Database of Systematic Reviews, K. E. Laver, Ed. Chichester, UK: John Wiley & Sons, Ltd, 2015. [ Links ]
[34] K. I. Ustinova, J. Perkins, W. A. Leonard, C. D. Ingersoll, and C. Hausebeck, “Virtual reality game-based therapy for persons with TBI: A pilot study,” in 2013 International Conference on Virtual Rehabilitation (ICVR), 2013, pp. 87-93. [ Links ]
[35] Y. Zuleima Ordóñez, C. Andrés Luna, and C. Felipe Rengifo, “Herramienta de Entrenamiento Virtual en 2-D para Rehabilitación de Motricidad Fina en Miembro Superior con Incorporación de un Dispositivo Háptico (software para rehabilitación fina en miembro superior),” Rev. Ing. Biomédica, vol. 7, no. 14, pp. 60-68, 2013. [ Links ]
[36] Z. Xu, R. Fiebrink, and Y. Matsuoka, “Virtual therapist: A Phantom robot-based haptic system for personalized post-surgery finger rehabilitation,” in 2012 IEEE International Conference on Robotics and Biomimetics (ROBIO), 2012, pp. 1662-1667. [ Links ]
[37] I. D. Plazas-Roa and A. F. Ruiz-Olaya, “A Tele-robotic System for Real-Time Remote Evaluation of Upper-Limb Function,” in VI Latin American Congress on Biomedical Engineering, 2015, pp. 230-233. [ Links ]
[38] V. Abraham, “The use of robotic/computer assistive technologies (R/CAT) during upper limb rehabilitation therapy sessions,” Int. J. Stroke, vol. 10, no. S3, 2015. [ Links ]
[39] A. F. Ruiz-Olaya, “Towards a robotic exoskeleton for remote evaluation of elbow and wrist joints,” in 2015 International Conference on Virtual Rehabilitation (ICVR), 2015, pp. 174-175. [ Links ]
[40] G. D. Sosa, J. Sanchez, and H. Franco, “Improved front-view tracking of human skeleton from Kinect data for rehabilitation support in Multiple Sclerosis,” in 2015 20th Symposium on Signal Processing, Images and Computer Vision (STSIVA), 2015, pp. 1-7. [ Links ]
[41] G. D. Voinea and G. Mogan, “Development of a Wearable Scoliosis Monitoring System Using Inertial Sensors,” Appl. Mech. Mater., vol. 811, pp. 353-358, Nov. 2015. [ Links ]
[42] M. Callejas-Cuervo, J. C. Alvarez, and D. Alvarez, “Capture and analysis of biomechanical signals with inertial and magnetic sensors as support in physical rehabilitation processes,” in 2016 IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN), 2016, pp. 119-123. [ Links ]
[43] Joonbum Bae, Wenlong Zhang, and M. Tomizuka, “Network-Based Rehabilitation System for Improved Mobility and Tele-Rehabilitation,” IEEE Trans. Control Syst. Technol., vol. 21, no. 5, pp. 1980-1987, Sep. 2013. [ Links ]
[44] W. Alcocer, L. Vela, A. Blanco, J. Gonzalez, and M. Oliver, “Major trends in the development of ankle rehabilitation devices,” Dyna, vol. 79, no. 176, pp. 45-55, 2012. [ Links ]
[45] M. C. Cuervo, A. F. R. Olaya, and R. M. G. Salamanca, “Biomechanical motion capture methods focused on tele-physiotherapy,” in 2013 Pan American Health Care Exchanges (PAHCE), 2013, no. September, pp. 1-6. [ Links ]
[46] A. Liberati, D. G. Altman, J. Tetzlaff, C. Mulrow, P. C. Gøtzsche, J. P. A. Ioannidis, M. Clarke, P. J. Devereaux, J. Kleijnen, and D. Moher, “The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration,” PLoS Med., vol. 6, no. 7, p. e1000100, Jul. 2009. [ Links ]
[47] “Proyecto Telerehabilitación fundación IDEAL.” [Online]. Available:http://www.fundacionideal.org.co/proyectos/proyecto-telerehabilitación-fundacion-ideal. [Accessed: 23-May-2017] [ Links ].
[48] L. Yunda, L. F. G. Ortega, S. Rodríguez, and R. M. Muñoz, “Plataforma Web para un nuevo modelo de telerehabilitación, de base comunal, en áreas rurales,” Sist. y Telemática, vol. 9, no. 19, pp. 55-67, 2011. [ Links ]
[49] M. C. Manuel, A. V. Andrés, F. R. Rafael, M. Gutiérrez-salamanca, M. Andrés, A. Felipe, and M. Rafael, “Architecture proposal for a support system to upper limb telerehabilitation by capturing biomechanical signals Propuesta de arquitectura para un sistema de apoyo a telerehabilitación de miembro superior capturando señales biomecánicas Proposta de arquitet,” Rev. Fac. Ing., vol. 24, no. 40, pp. 43-50, 2015. [ Links ]
[50] M. Callejas-Cuervo, A. F. Ruíz-Olaya, and R. M. Gutiérrez, “Validación de una plataforma basada en sensores inerciales para adquirir información cinemática de estimación del ángulo articular humano,” DYNA, vol. 83, no. 197, p. 153, Jun. 2016. [ Links ]
[51] M. Callejas-Cuervo, R. M. Gutierrez, and A. I. Hernandez, “Joint amplitude MEMS based measurement platform for low cost and high accessibility telerehabilitation: Elbow case study,” J. Bodyw. Mov. Ther., vol. 21, no. 3, pp. 574-581, Jul. 2017. [ Links ]
[52] A. Uribe-Quevedo and B. Kapralos, “Exergaming for Shoulder-Based Exercise and Rehabilitation,” in Recent Advances in Technologies for Inclusive Well-Being, Springer, Cham, 2017, pp. 105-125. [ Links ]
[53] N. F. Nascimento, “Treino com realidade virtual no alcance manual de crianças com paralisia cerebral: ensaio clínico randomizado cruzado,” Universidade Federal Do Rio Grande Do Norte, 2015. [ Links ]
[54] M. Araújo, M. K. Postól, and A. D. Bruckheimer, “Realidade virtual: efeitos na recuperação do membro superior de pacientes hemiparéticos por acidente vascular cerebral,” Arq. Catarinenses Med., vol. 43, no. 1, pp. 15-20, 2014. [ Links ]
[55] Fabiana Rita Camara Machado, “Uso do Kinect® na reabilitação motora de crianças com paralisia cerebral,” Fundação Universidade Federal de Ciências da Saúde de Porto Alegre, 2014. [ Links ]
[56] M. R. Marques, “Viabilidade do uso de ferramentas de telereabilitação para o acompanhamento à distância de pacientes com sequelas pós-acidente vascular cerebral,” Universidade de Sao Paulo, 2014. [ Links ]
[57] J. F. López-Herrera, John E. Muñoz-Cardona, Oscar A. Henao-Gallo, “Sistema de Rehabilitación basado en el Uso de Análisis Biomecánico y Videojuegos mediante el Sensor Kinect,” Tecno Lógicas, pp. 43-54, 2013. [ Links ]
[58] G. G. Ito, “Sistema mecatrônico para reabilitação pós fratura da extremidade distal do rádio,” University of São Paulo, 2011. [ Links ]
[59] A. Uribe, “Desenvolvimento de dispositivo para membro inferior com deficiência parcial,” Universidade Estadual de Campinas, 2011. [ Links ]
[60] K. L. Nogueira, “Um framework de realidade virtual e aumentada para apoio a sistemas de reabilitação,” Universidade Federal de Uberlandia, 2014. [ Links ]
[61] M. C. DOrnellas, D. J. Cargnin, and A. L. C. Prado, “Thoroughly Approach to Upper Limb Rehabilitation Using Serious Games for Intensive Group Physical Therapy or Individual Biofeedback Training,” in 2014 Brazilian Symposium on Computer Games and Digital Entertainment, 2014, pp. 140-147. [ Links ]
[62] D. J. Cargnin, M. C. DOrnellas, and A. L. C. Prado, “A Serious Game for Upper Limb Stroke Rehabilitation Using Biofeedback and Mirror-Neurons Based Training.,” MedInfo, 2015. [ Links ]
[63] A. V. Soares, S. S. Woellner, C. dos S. Andrade, T. J. Mesadri, A. D. Bruckheimer, and M. da S. Hounsell, “The use of Virtual Reality for upper limb rehabilitation of hemiparetic Stroke patients,” Fisioter. em Mov., vol. 27, no. 3, pp. 309-317, Sep. 2014. [ Links ] [ Links ]
[65] “Primer centro de rehabilitación Virtual en Mexico | Virtualware.” [Online]. Available: http://virtualwaregroup.com/es/noticias/primer-centro-rehabilitacion-virtual-mexico. [Accessed: 13-Jul-2017] [ Links ].
[66] B. Maldonado, M. Mendoza, I. Bonilla, and I. Reyna-Gutierrez, “Stiffness-based tuning of an adaptive impedance controller for robot-assisted rehabilitation of upper limbs,” in 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 2015, pp. 3578-3581. [ Links ]
[67] M. Mendoza, I. Bonilla, E. González-Galván, and F. Reyes, “Impedance control in a wave-based teleoperator for rehabilitation motor therapies assisted by robots,” Comput. Methods Programs Biomed., vol. 123, pp. 54-67, 2016. [ Links ]
[68] T. A. C. Aguilar, B. V Manrique, and J. A. Torrejon, “Development of a Mechatronic Device for Arm Rehabilitation,” in 2do Congreso Internacional de Sistemas Embebidos y Mecatrónica, 2016, pp. 23-27. [ Links ]
[69] K. Bustamante Valles, S. Montes, M. de J. Madrigal, A. Burciaga, M. E. Martínez, and M. J. Johnson, “Technology-assisted stroke rehabilitation in Mexico: a pilot randomized trial comparing traditional therapy to circuit training in a Robot/technology-assisted therapy gym,” J. Neuroeng. Rehabil., vol. 13, no. 1, p. 83, 2016. [ Links ]
[70] C. E. López Padilla, J. L. Acosta García, W. C. Perez, M. A. Lugo Villeda, G. I. ellez Rodríguez, and I. Saucedo Ugalde, “Interfaz Háptica Teleperada para Rehabilitación Pediatríca,” in Memorias del XV Congreso Mexicano de Rob´ otica, 2014. [ Links ]
[71] J. Andrés, S. Castro, G. Irene, T. Rodríguez, A. B. Cerón, I. S. Ugalde, D. Aydee, and R. Vega, “Desarrollo del Entorno Virtual y Auditivo de una Plataforma Háptica para Rehabilitación Neurolingüística y Motriz,” in XV COMROB, 2013. [ Links ]
[72] C. Ramírez-Fernández, E. García-Canseco, A. L. Morán, O. Pabloff, D. Bonilla, N. Green, and V. Meza-Kubo, “GoodVybesConnect: A Real-Time Haptic Enhanced Tele-Rehabilitation System for Massage Therapy,” in Computing and Ambient., Springer, Cham, 2016, pp. 487-496. [ Links ]
[73] G. Borrego, A. L. Morán, A. LaFlor, V. Meza, E. García-Canseco, F. Orihuela-Espina, and L. E. Sucar, “Pilot Evaluation of a Collaborative Game for Motor Tele-Rehabilitation and Cognitive Stimulation of the Elderly,” in Lecture Notes in Computer Science, Springer, Cham, 2015, pp. 42-48. [ Links ]
[74] S. I. Macías-Hernández, D. S. Vásquez-Sotelo, M. V. Ferruzca-Navarro, S. H. Badillo Sánchez, J. Gutiérrez-Martínez, M. A. Núñez-Gaona, H. A. Meneses, O. B. Velez-Gutiérrez, I. Tapia-Ferrusco, M. de los Á. Soria-Bastida, R. Coronado-Zarco, and J. D. Morones-Alba, “Proposal and Evaluation of a Telerehabilitation Platform Designed for Patients With Partial Rotator Cuff Tears: A Preliminary Study,” Ann. Rehabil. Med., vol. 40, no. 4, p. 710, 2016. [ Links ]
[75] G. Palacios-Navarro, S. Albiol-Pérez, and I. García-Magariño, “A Kinect-Based Virtual Reality System for Parkinson Disease Rehabilitation,” in New Contributions in Information Systems and Technologies, Springer, Cham, 2015, pp. 1133-1139. [ Links ]
[76] S. Albiol-Pérez, E.-P. Pruna-Panchi, I.-P. Escobar-Anchaguano, J.-G. Bucheli-Andrade, M.-A. Pilatasig-Panchi, L.-E. Mena-Mena, J. Segovia-Chávez, A. Bernis, and P. Zumbana, “Acceptance and Suitability of a Novel Virtual System in Chronic Acquired Brain Injury Patients,” in New Advances in Information Systems and Technologies, Springer, Cham, 2016, pp. 1065-1071. [ Links ]
[77] S. Albiol-Pérez, E.-P. Pruna-Panchi, I.-P. Escobar-Anchaguano, M.-A. Pilatasig-Panchi, L.-E. Mena-Mena, J. Segovia-Chávez, A. Bernis, and P. Zumbana, “A Neurocognitive Virtual Rehabilitation System for Children with Cerebral Palsy: A Preliminary Usability Study,” in New Advances in Information Systems and Technologies, Springer, Cham, 2016, pp. 1057-1063. [ Links ]
[78] E. Pruna, A. Acurio S., I. Escobar, S. A. Pérez, P. Zumbana, A. Meythaler, and F. A. Álvarez, “3D Virtual System Using a Haptic Device for Fine Motor Rehabilitation,” in Recent Advances in Information Systems and Technologies, Springer, Cham, 2017, pp. 648-656. [ Links ]
[79] S. Albiol-Pérez, J. Mena-Cajas, I.-P. Escobar-Anchaguano, E.-P. Pruna-Panchi, and P. Zumbana, “Virtual fine rehabilitation in patients with carpal tunnel syndrome using low-cost devices,” in Proceedings of the 4th Workshop on ICTs for improving Patients Rehabilitation Research Techniques - REHAB 16, 2016, pp. 61-64. [ Links ]
[80] E. Pruna, W. López V., I. Escobar, E. D. Galarza, P. Zumbana, S. Albiol-Pérez, G. Ávila, and J. Bucheli, “Implementation of a Multipoint Virtual Goniometer (MVG) Trough Kinect-2 for Evaluation of the Upper Limbs,” in Recent Advances in Information Systems and Technologies, Springer, Cham, 2017, pp. 639-647. [ Links ]
[81] Y. Rybarczyk, J. K. Deters, A. A. Gonzalo, D. Esparza, M. Gonzalez, S. Villarreal, and I. L. Nunes, “Recognition of Physiotherapeutic Exercises Through DTW and Low-Cost Vision-Based Motion Capture,” in Advances in Human Factors and Systems Interaction, Springer, Cham, 2016, pp. 348-360. [ Links ]
[82] “Plataforma de tele-rehabilitación para adultos mayores con trastornos asociados a demencia, basada en tecnologías emergentes,” 2015. [Online]. Available: https://www.cedia.edu.ec/es/plataforma-de-tele-rehabilitacion-para-adultos-mayores-con-trastornos-asociados-a-demencia-basada-en-tecnologias-emergentes. [Accessed: 17-May-2017] [ Links ].
[83] “Kushkalla: Tele-Rehabilitation,” 2016. [Online]. Available: https://kushkalla.cedia.org.ec/. [Accessed: 17-May-2017] [ Links ].
[84] P. U. Caro, C. S. Siqués, R. B. Cubillos, and D. P. García, “Evaluación de satisfacción frente al uso del programa de telerehabilitación Rehabitic® para terapia física en niños con parálisis cerebral del Instituto Teletón Santiago. Estudio de 3 casos. [ Links ]”
[85] “Virtualrehab | Teleton avanza en la implementación de las terapias de rehabilitacion.” [Online]. Available: http://www.virtualrehab.info/es/teleton-avanza-en-la-implementacion-de-las-terapias-de-rehabilitacion/. [Accessed: 23-May-2017] [ Links ].
[86] “Teletón participa en congreso sobre nuevas tecnologías en salud.” [Online]. Available: http://www.teleton.cl/noticias/teleton-participa-en-congreso-sobre-nuevas-tecnologias-en-salud/. [Accessed: 18-May-2017] [ Links ].
[87] “Hospital Italiano de Buenos Arires: Telerehabilitación Integral, Cognitiva y Kinésica.” [Online]. Available: https://www.hospitalitaliano.org.ar/#!/home/comercial/noticia/26767. [Accessed: 15-May-2017] [ Links ].
[88] F. J. Cáceres, “Neurorehabilitación en Esclerosis Múltiple: ¿Donde estamos?,” in Biogen MS Innovation, 2015. [ Links ]
[89] C. Ferrarini Oliver, M. G. González de Doña, S. G. Zapata, L. A. L. Olguín, E. G. Ormeño, C. Ferrarini, M. González, S. G. Zapata, L. A. L. Olguín, and E. G. Ormeño, “MoVeR-T: Entorno de videojuego en Realidad Virtual Telecontrolado para Rehabilitación Motriz,” in XVIII Workshop de Investigadores en Ciencias de la Computación, 2016, pp. 621-625. [ Links ]
[90] D. Chueke, “Panorama de la Telemedicina en América Latina,” eyeforpharma. 2015. [ Links ]
[91] P. S. Archambault, N. G. Norouzi, D. Kairy, J. M. Solomon, and M. F. Levin, “Towards Establishing Clinical Guidelines for an Arm Rehabilitation Virtual Reality System,” in Replace, Repair, Restore, Relieve - Bridging Clinical and Engineering Solutions in Neurorehabilitation. Biosystems & Biorobotics, Springer, Cham, 2014, pp. 263-270 [ Links ]