INTRODUCTION
The World Health Organization (2012) defines dementia as a chronic and progressive brain disease that impairs memory, thinking, orientation, language, learning capacity and decision-making; as well as compromises emotional control, motivation and social behavior. The most common types of dementia are: Alzheimer's dementia (AD), vascular dementia with Lewy bodies and frontotemporal dementia; additionally, being frequent, dementia with mixed pathologies (Neuropathology Group of the Medical Research Council Cognitive Function and Aging Study, 2001; Niedermeyer & Ghigo, 2011).
In the world, there are about 47.5 million people with dementia, and each year, 7.7 million of new cases are expec ted (World Health Organization (WHO), 2012). Given the increase of life expectancy and the possibility of a greater diagnosis accuracy, it is estimated that by 2030 there will be 70 million cases of AD, approximately (Ferri et al, 2005).
The global annual cost of dementia for 2005, is estimated at 215 billion euros, and the annual spending average on medication for patient is estimated at 1.825 dollars and 15 per hour. Though, an AD early diagnosis and treatment, can represent significant savings for health system (Hogervorst, Ribeiro, Molyneux, Budge & Smith, 2002; Mittelman, Haley, Clay & Rith, 2006; Skoog et al., 1996).
In Latin America the prevalence of AD is: Peru 6.7%, Venezuela 8%, Argentina 11.5% and Brazil 5.3% (Custodio, Gutiérrez & Garcia, 2007; Molero, Pine-Ramirez & Master, 2007; Pages- Larraya, Grasso & Mari, 2004). In Colombia, the prevalence of AD for the year 2002 was 1.8% in patients between 65 and 74 years old, and 3.4% in population over 75 years old; with the highest prevalence in south-western (2,2%), and eastern (1.9%) (Pradilla, et al., 2002, Rosselli et al., 2000). The Memory Clinic at the Javeriana University in Bogota reported 2.018 patients diagnosed with dementia during the years 1997 to 2009. From this population, 49.56% had AD, 28.4% of them were women and 71.6% were men (Ruiz et al., 2009).
AD is characterized by an insidious course and the presence of the symptoms triad: amnesia, anomie, and apraxia. It is developed by a combination of factors (envi ronmental, genetic, and lifestyle); the disease may occur at any time of life, but it is most common in the elderly; and it is not considered as being part of the normal aging process (WHO, 2010).
Though until today, the AD does not have a cure; the treatments, pharmacological and non-pharmacological, have the purpose to reduce emotional symptoms, maintain a stable clinical condition, and mainly, promote patients' quality of life. Pharmacological treatments address the management of some symptoms and include antidepressants, cholinesterase inhibitors, antipsychotics, sedatives and others. Regarding non-pharmacological intervention programs, treatment modality depends on the patient deterioration degree. In early stages it seeks to stimulate or maintain cognitive and functional processes, and for advanced stages, the goal is to offset difficulties through external aid. As part of non-pharmacological programs, lately, a greater importance it has been given to physical activity. These type of programs intend to maintain mobility and balance, reduce the risk of falls, and improve mood; based on epidemiological studies results that indicate the relationship between physical activity and cognitive functioning (WHO, 2012).
It has been found that involve patients with AD in daily activity routines, that include physical activity, improve muscle strength, cardiorespiratory resistance, balance, flexibility, bone density, sleep quality, functionality, social interaction, and decrease behavioral and emotional altera tions (Arlene, Marieke & David, 2010; Chen et al., 2008; Dayanim, 2009; Graff-Radford, 2011; Gudlaugsson, et al., 2013; Liu & Latham, 2009; Oken et al., 2006; US Department of Health and Human Services, 2008; Ramos-Jimenez et al., 2009; Radak, et al., 2010; Yu & Kolanowski, 2009). U.S Department of Health and Human Services (2008) recommends that physical activity programs for people diagnosed with AD, be designed including a minimum of 150 minutes per week of aerobic activities, plus strength activities at least twice a week. However, the best results could be obtained by combining physical activity with cognitive tasks (Winchester et al., 2013).
The effects of exercise in patients with AD can be explained first, because exercise produces metabolic and neurological changes associated with decreased abnormal production of β-amyloid protein in the frontal cortex and hippocampus. It also increases blood circulation in the frontal, parietal and temporal lobes; and promotes the growth of capillaries in the primary motor cortex; as well as it promotes regulation of nitric oxide, that stimulates nerve growth factors, that are related with the production and operation of neurotransmitters, and with the increase of calcium levels that instead stimulate the dopamine synthesis. Second, it increases the endorphins production that helps reduce depression and promote feelings of well-being. And third, as in healthy people, physical activity, generates an increment of endorphins production, increases functionality, and improves physical qualities such as strength, flexibility and balance (Pérez & Cancela Carral, 2008).
Coehlo et al. (2012) conducted a study involving 27 people with AD. They applied a progressive complexity program of 16 weeks. The program included aerobic, strength, flexibility, balance, agility and cognitive activi ties. The authors found significant differences favoring the experimental group with respect to executive functions, information processing speed, and less deterioration.
De Andrade et al. (2013) conducted a study with the aim of improving fitness and executive functions with 30 AD patients, all with pharmacological intervention. They were divided in two groups (experimental and control). They increased the difficulty level of physical activity every four weeks up to 65% -75% of maximum heart rate. The results showed greater functionality and performance in executive functions in the experimental group; as well as better scores in the processing speed; however, they do not find statistically significant differences between groups.
Winchester et al. (2013) conducted a study through one year with 104 AD patients that were older than 60 years. The physical activity program involved various activities such as bowling, cycling, walking, swimming, yoga, strength training and hiking. The caregiver should record the amount of time the patient devoted to these activities every week, as well as the performance intensity. People walking constantly obtained more stable MMSE scores after 12 months.
Hatha yoga as physical activity has been studied as an exclusive intervention or in combination with traditional drug treatments for cancer (Cramer, et al, 2012; Smith & Pukall, 2009), menopausal symptoms (Cramer, Lauche, Langhorst & Dobos, 2012), chronic pain (Li & Goldsmith, 2012), anxiety and schizophrenia (Cramer et al., 2014; Vancampfort, et al, 2012), among other diseases. These programs are based on body postures (asanas) and slow and conscious movements, accompanied with breathing techniques (pranayama) and meditation exercises, that have the purpose of focusing attention (dyana).
Sengupta (2012) points out that yoga reduces arousal, heart rate, blood pressure and eases breathing; increases pain tolerance as well as melatonin levels in the blood; it also improves heart rate variability that is an indicator of adequate response to stress (Madanmohan, Rai, BalaVittal & Thombre cited by Sengupta, 2012; Smith, Hancock, Blake-Mortimer & Eckert, 2007; Tooley, Armstrong, Norman & Sali, 2000).
Some studies (Kjaer et al., 2002) have shown that Hatha yoga practice can increase the release of endogenous do-pamine in the ventral striatum and in the thalamic GABA levels. Likewise, it is associated with the increase of plasma serotonin in patients with depression (Devi, Chansauria & Udupa cited by Cramer et al., 2014). There is also evidence that yoga practice regulates the hypothalamic-pituitary-adrenal axis, that manages stress responses (Streeter, Gerbarg, Saper, Ciraulo & Brown, 2012) and it decreases levels of plasma cortisol (Jarcho, Slavich, Tylova-Stein, Wolkowitz & Burke, 2013; Gartside, Leitch, McQuade & Swarbrick, 2003; Vadiraja et al., 2009). Despite the described results, these are still considered inconclusive due to methodological difficulties (Li & Goldsmith, 2012).
Khoo, Van Schaik and McKeena (2014) conducted a study that aimed to assess the holistic exercise in 15 older adults with dementia. "Happy Antics Program" sessions were performed once a week, for 45 minutes, during six weeks. The program integrated music choreographed with tai-chi exercise, meditation, qigong, dancing and mindful-ness. Cognitive exercises were based on the presentation of images and the discussion about them; participants were reminded weekly for attending meetings; 70% attendance was reported. Results of a semi structured interview, after the program, established that all participants enjoyed the program, this was perceived as an opportunity to socialize and acquire new learning, and some patients reported pain decreased and relaxation after sessions. Six participants could anticipate movements associating them with music, and three could remember sequences of complete movements.
These results are consistent with those of Barnes, Mehlin, Taffe, Flores and Chesney (2013), who evaluated the PLIE (Preventing Loss of Independence through Exercise) program that uses six methods to keep the patients active, based on physical and occupational therapy, yoga, tai-chi and dance: (a) repetition with variations, (b) progressive and functional movements, (c) step by step instruction, (d) goals orientation, (e) physical care, mindfulness and breathing, and (f) social interaction. This program differs from Khoo et al. (2014) program that does not include cognitive stimulation exercises.
Fan and Chen (2011) evaluated the effects of a silver-yoga program (Hatha yoga combined with gerontology principles) on physical and mental health of 68 elderly people with dementia. The intervention consisted of three weekly sessions of 55 minutes each, during 12 weeks. The sessions included heating, Hatha yoga, and relaxation; involving two trainers, one as a model and the other as a support. The results showed significant differences between the experimental group measures pre-and post and among groups (experimental and control) in physical variables (blood pressure, respiratory rate, cardiopulmonary condition, flexibility, grip strength, muscular resistance, joint mobility and balance). In addition, the patients decreased behavioral problems and depression, and increased their interactions. These results are consistent with other studies (Arlene et al., 2010; Chen et al., 2008; McCaffrey, Ruknui, Hatthakit, & Kasetsomboon, 2014; Oken et al., 2006. Ramos-Jimenez et al., 2009).
Cramer et al. (2014) conducted a meta-analysis to determine the effect of yoga in patients with depressive disorders, differentiating short- (12 weeks) and long term (12 months). The results revealed a short but not long-term moderate effect. There was most effective evidence in patients with high levels of depression than in those diagnosed with depressive disorder. It was also found that the effects of yoga were comparable to those of drug treatment and group therapy.
Oken et al. (2006) point out there are at least two poten tial mechanisms by which, both Hatha yoga practice and exercise, could optimize cognitive ability. Both activities improve mood and reduce stress, that are related to cognitive decline. Moreover, the practice of yoga emphasizes body awareness, and the fact that involves focusing on breathing on specific muscles, could stimulate attention, a process that is essential for carrying out different tasks in everyday life, and necessary for learning, memory and language.
The literature review shows an extensive scientific interest on physical activity based on Hatha yoga and specifically in patients with AD, interest associated with the growth of worldwide elderly population; however, in Colombia there are no studies on the subject even though the number of people diagnosed with dementia keeps growing year after year. Thus, this study aims to determine the effect of a program of Hatha yoga on psychological variables (quality of life, depression, attention, memory and overall cogni tive functioning) and functional variables (independence to perform basic and instrumental daily life activities) in patients diagnosed with Alzheimer in the city of Bogotá.
METHOD
Participants
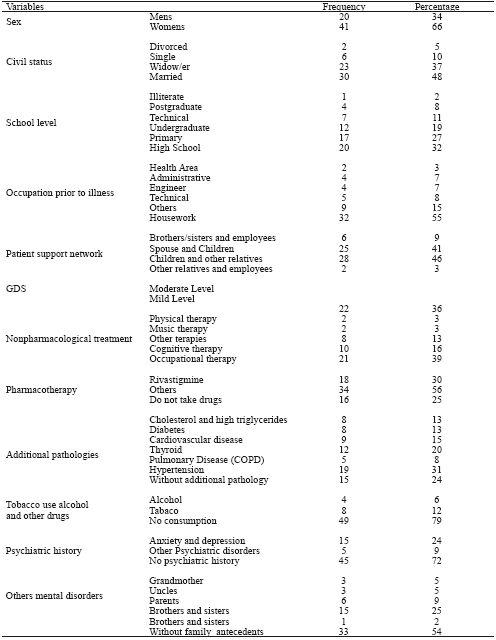
Participants sample was selected for convenience and consisted of 61 patients and their caregivers, who agreed to participate in the study voluntarily, and signed an informed consent. Inclusion criteria were: diagnosis of Alzheimer's disease by interdisciplinary team consensus (neurologist, psychiatrist, geriatrician, neuropsychologist, psychologist and occupational therapist); level of impairment, mild to moderate, according to the Global Deterioration Scale (GDS); do not present physical and sensory problems that would prevent patients from participate in the yoga program, they should be affiliated to a Health Promoting Company (EPS due to its initials in Spanish), and each patient should always be accompanied by a caregiver.
48% patients had never attended a yoga class, 22% had taken classes for at least one year, and one patient reported having taken classes for seven years. However, none of the patients reported being linked to yoga classes at the beginning of this study. According to caregivers, 72% patients had hearing loss, 60% used reading glasses and 23% had some ocular pathology (mostly cataracts). These sensory distur bances did not affect test performance neither participation in the program. 18% patients reported having been beaten in the head before the disease diagnosed, but there was no evidence for neurological sequelae. All patients reported having an adequate family support network, consisting in most cases by their spouses, children and other relatives (87%) (See Table 1).
Instruments
The following instruments were used:
Quality of Life Questionnaire: Built to measure quality of life in people with dementia, it is a scale that is applied to the caregiver and consists of 25 Likert items (0 = never and 4 = always). A higher score corresponds to a better quality of life. The questionnaire evaluates functionality, physical activity, affectivity, interpersonal relationships and cognitive aspects. Based on data from 59 patients (40 women and 19 men) diagnosed with Alzheimer, GDS mild to moderate, average age 75.4 and SD = 11.2; the authors estimated the Cronbach Alpha coefficient for the QoL scale (r = 0.81) and for each of the subscales: functional, physical, emotional, interpersonal, and cognitive (r = 0.62, r = 0.58; r = 0.88, r = 0.51 and r = 0.68 respectively). Also, they estimated the Pearson correlation coefficient between the QoL questionnaire total scores and ADRQL; and the result is r =0, 714 (p <.001), data that suggests that both tests are measuring the same construct (quality of life).
Scale of Alzheimer's Disease Related Quality of Life in (ADRQL) (Hophins, 2011); it evaluates the quality of life in people with AD. It is applied to the caregiver asking about the two prior weeks; it consists of 47 items with response type "agree" and "disagree", and assesses five subscales: (a) relationships with others, (b) personal and important identity, (c) stressful behaviors, (d) daily activities, and (e) behavior in the place of residence. The higher the scores the better quality of life. Based on data from 59 patients diagnosed with Alzheimer GDS mild to moderate (40 women and 19 men), average age 75.4 and SD = 11.2; the authors estimated the Cronbach Alpha coefficient for the total ADQRL scale (r = 0.79) and for each subscale (r =0. 61; r = 0.59; r = 0.68, r = 45 and r = 0.54, respectively).
Geriatric Depression Scale (Yesavage); the short version of 15 items validated for Spanish people over 65 years was used, it evaluates depressive symptoms (Martinez de la Iglesia et al., 2002). The examinee must answer YES or NO to the reading of each of the 15 claims. It is considered 0 to 5 normal, 6 to 10, moderate depression, and 11 to 15 severe depression. The Spanish validation reported rates for high reliability test: intraobserver (r =0.95), interobserver (r =0. 65) and internal consistency (r =0. 99) (Martinez de la Iglesia et al., 2002).
Digit Symbol subtest. It is part of the Wechsler Intelligence Scale (1997), and assesses the ability to sustain visual attention, motor persistence, information processing speed, and imitative activity. The task is to identify each number and put the symbol under. Henao et al. (2010) conducted a study to obtain evidence for reliability and validity, with elderly with and without a diagnosed of AD. Results indicate that the internal consistency coefficients are greater than r = 0.75 for both samples. They also obtained indices of intra-class correlation test-retest with a difference of a month, and the results were also higher than r =0.75 for both cases. These authors also pointed out that elderly performance on this test is based on their age, educational level, and level of cognitive decline, such as is the case of AP.
TrailMaking Test Form A (TMTA); it evaluates sustained attention through 25 digits visual search and tracking. The number of correct sequences is achieved in a maximum run time of 120 seconds. Henao et al. (2010) conducted a study to obtain evidence of reliability and validity with elderly with and without AD. Results indicate that for correct answers the coefficient of internal consistency in people with AD is r =0. 60 and the rate of intra-class correlation test-retest with a month of difference is r = 0.70, for both cases.
Digit Span subtest in forward and reverse order; it is part of the Wechsler Intelligence Scale for adults (WAIS-III) (1997) that measures attention and working memory. It is composed by pairs of numbers series, from three to nine digits, that the examiner repeats forward; and two to eight digits, that the examiner repeats backward. Both tasks require auditory attention and retention capacity in short term and working memory. Ardila, Roselli and Puente (1994) indicate that a normal retention performance of digits forward is between 6 +/- 1, and retention backwards is between 4 to 5 digits with differences considered normal in a range of one to two digits. In addition, individuals of 70 years or older, can present a decline in the backward digit span, and their educational level is related with this test performance (Ardila, Ostrosky-Solis, Roselli, & Gómez, 2000). AP have lower performance than expected in retention digit backward; additionally, in Alzheimer's advanced stages, the retention digit forward is also affected (Howeison & Lezak, 2008).
Mini-Mental State Examination (MMSE); it was used based on the study of Ardila et al. (2000) who shows that this test might be useful for assessing dementia. It assesses orientation, information retention, attention and calculation, recall, language, and construction. It is a screening scale that provides a measure of global cognitive performance. Maximum score to be obtained is 30, but it was cut at 26 because of a low educational level and mild cognitive im pairment on performance (Prince, Acosta, Chiu, Scazufica & Varghese, 2003). The MMSE with a cutoff of 25 based on ten studies has a sensitivity of 0.87 and specificity of 0.92; and a cutoff of 24 based on 15 studies, it has a sensitivity of 0.85 and specificity of 0.90 (Creavin et al., 2016).
Barthel scale (Mahoney & Barthel, 1965). It is applied to the caregiver, and assesses independence, need for help, or dependence in 10 areas of everyday life: food, transfers, personal hygiene, use of toilet, shower-bath, scroll up and down stairs, dressed, and bowel and bladder continence. A higher score means greater independence. The internal consistency coefficient Cronbach Alpha was r = 0.80 based on data from 59 patients (40 women and 19 men) diagnosed with Alzheimer, GDS mild to moderate, average age 75.4 and SD = 11.2. This estimate is consistent with the reported rate of others studies (Cid-Ruzafa & Damian-Moreno, 1997).
Lawton and Brody Scale (Lawton & Brody, 1969); it is applied to the caregiver, and measures the patient's level of independence to perform 14 instrumental activities of daily life. It is scored on four levels: without difficulty, with help, with difficulty, and always with help. A higher score means greater independence. Cronbach's Alpha coefficient (r = 0.89) was estimated based on data reported by care givers of 59 patients (40 women and 19 men) diagnosed with Alzheimer, GDS mild to moderate, average age 75.4 and SD = 11.2.
Procedure
In order to get the sample, authors made three calls through the Memory and Cognition Center "Intellectus" and the Foundation "Acción Familiar Alzheimer Colombia". The authors contacted by telephone 172 relatives of patients with AD. After hear the explanation of the program, 65 people (100%) enrolled in it. From this population 61 (94%) made the pre-test, 48 (74%) the posttest, and 35 patients (54%) completed the final monitoring test (6 months after the program ended).
Authors adjusted the program made by Quintero, Rodriguez, Guzman, Llanos and Reyes (2011). To do this, they trained a yoga instructor that was an expert in working with elderly people. The training was for skills to management of AD patients, then, they selected the most appropriate postures. These stances consisted of movements of extension and flexion of the spine involving flexibility, balance, and coordination. Finally, authors applied a pilot program to two healthy people (male and female), over 60 years. Based on the results of it, authors selected the final positions, and a new pilot was conducted with a person diagnosed with AD (86 years old, GDS 4, and with minor motor difficulties).
For the design and development of the final program, authors took into account the following: (a) short, simple instructions, (b) avoid complex names of body segments; (c) provide to patient visual and auditory contact with the instructor; (d) provide visual and verbal feedback execu tion; (e) touch the patients gently to correct their positions and generate an errorless learning (by the caregiver and research assistant), (f) positions are the same throughout the program (to facilitate appropriation and memorization) so that the level of demand is determined by the duration of a posture maintenance (initially more dynamic and ultimately more static) and posture accuracy, and (g) deliver a video program to facilitate maintaining yoga sessions at home.
Each yoga session consisted of awareness, warm-up exercises, postures, relaxation and closing.
• Awareness: it is the initial phase in which the partici pant is asked to focus his/her attention on his/her breathing (abdominal), emphasizing the relationship with the "here and now". This activity is included in other moments of the program to reorient the participant's attention to the present moment.
• Warm-up exercises: These prepare the body for the positions.
• Postures: they include various stances that should be performed (standing, sitting and lying); some of these are made dynamically (repeated) to encourage patients to gain body flexibility and gradually reach maintained fixed positions.
• Relaxation: it is the time when, in the session, each patient seeks to loose muscles and reduce thoughts continuum. It involves body and thoughts scanner in order to achieve a relaxation and rest state.
• Closing: It is done at the end of each session in easy stance (sitting with legs crossed) so that the participant is able to perceive the practice benefits, connects with his/her body and his/her breathing and observes, for a few minutes, the feeling of calm and wellness.
The yoga program consisted in 32 sessions, each of one hour, after which refreshments were offered to patients and caregivers; additionally, they were granted a transporta tion subsidy. Sessions took place in a room with adequate lighting and ventilation that was equipped with mattresses, blankets, and pillows; it can accommodate up to 30 people (patients and caregivers).
Authors trained, in clinical and observational skills, nine research assistants that applied test and interviews, to caregivers and patients; they also accompanied participants and facilitated the appropriation of the positions during program sessions.
Assessment pre-and post-treatment as well as the follow-up, six months after the program ended, were carried out at the place of residence of each patient. Once the program was completed, authors identified those patients that had attended more than 80% of the sessions. They invited them along with their caregivers to participate in a focus group interview. Twenty-two patients with their caregivers attended. Four patients groups and four caregivers groups were arranged, each group with a five member's average. Before each interview, everyone was given an informed consent that asked for videotaping authorization. Records obtained in the focus groups were transcribed and names were changed to preserve confidentiality. Inquiry object was looking for verbatim reports that indicate observed or perceived changes in patients' cognitive, affective, and functional level; and quality of life due to their participation in the Hatha yoga program.
RESULTS
Following, the results of this study are presented for each of the research specific objectives. The aim was to evaluate the effect of a Hatha yoga program in patients with AD on quality of life, depression, attention, memory, global cognitive functioning, and independence level in daily activities.
For all data analyzes, the authors used each test direct scores. In addition, it presents the results of patients and caregivers focus groups related to the perceived effects of the program on patients.
Yoga program effect on quality of life of AP
It compared the scores obtained on pre-treatment, post-treatment and follow-up at six months of the quality of life questionnaire (CV) and the ADQRL test.
The results for the z Kolmogorov Smirnov statistic for both test scores and their dimensions indicate that data fit the normal curve (p>0.05). The descriptive statistics (Table 2) indicate that the mean of both measures has growth rates until post treatment; however, from post treatment it shows a negative growth rate (see Figure 1). Additionally, the ANOVA of repeated measures for this variable indicates that there are not significant differences for neither of the tests scores (CV F2,J3 = 0.064;p> 0,05 and ADQRL F2,33 = 0.021;p> 0.05) between the three measurements.
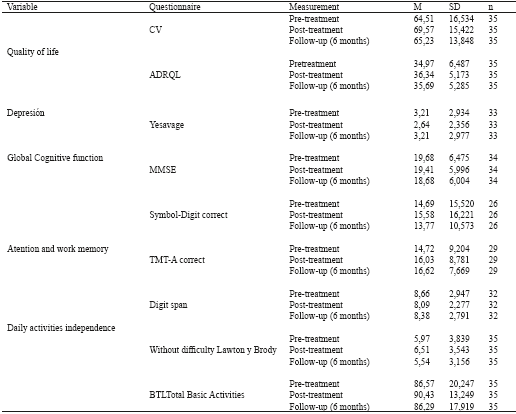
Table 2 Descriptive statistics for measured variables
Note: Some total does not add up to 100% by data not reported.
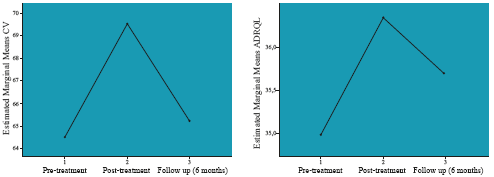
Figure 1 Mean of the scores obtained on three measures in AP using CV and ADQRL questionnaires for quality of life (n = 35).
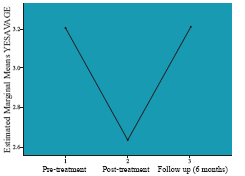
Yoga program effect on depression of AP
The scores of Yesavage Geriatric Depression Scale between three measurements were compared. The scores of this test fit the normal curve per the z Kolmogorov Smirnov statistic (p> 0.05). The results present in Table 2 and in Figure 2 indicate that the mean has a significant negative growth rate between pre-treatment and post-treatment, and the opposite trend between post-treatment and follow up. Either way, no score reaches values outside the range of "normal" according to the interpretative instrument scale. The ANOVA for repeated measures showed no statistically significant differences for this variable (F2 31) =0,034;p> 0.05) between the three measurements.
Yoga program on attention, memory and overall cognitive functioning of AP
To determine the effect of yoga program on attention and working memory, it was performed the same analysis from the scores on two subtests of the Wechsler Intelligence Scale (Symbol-Digit and Digit Span); and in order to assess the overall cognitive functioning MMSE was used. The scores of this test fit the normal curve per the z Kolmogorov Smirnov statistic (p> 0.05).
The results indicate that the mean of sustained attention and processing speed evaluated with the digit symbol, pre sented a growth rate between the measure of pre-treatment and post-treatment; meanwhile after post-treatment it shows a negative growth rate (table 2 and figure 3).
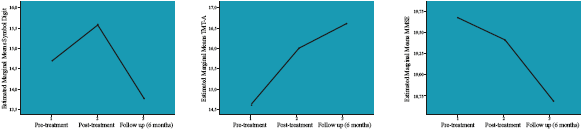
Figure 3 Mean of the scores obtained on three measures in APusing the scales Digit Symbol (n=26); TMT-A (n=29) and MMSE (n = 34).
Regarding test TMT-A, the average between pretreatment and posttreatment shows a growth rate that is maintained after the post-treatment measure. Referring to digit retention test, the mean tends to be constant in all three measurements. As for variable global cognitive function as measured by the MMSE scale, it has a negative growth rate, that is more marked once the program ends. The ANOVA of repeated measures showed no statistically significant differences for any of these cognitive variables among the three measurements (Symbol Digit: F2,22 =0. 010, p> .05; Digit Span:
F2,29 =0.025; p> 05; TMT-A F2,27 = 0,131, p> .05; MMSE:
F2,32 = 0.014, p> .05).
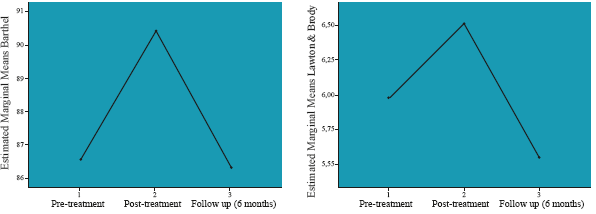
Yoga program effect on the level of independence in daily living activities of AP
It assessed the level of independence in daily living activities using the scores obtained with Lawton and Brody Scale and Barthel test. In the first case, the authors only took the number of activities that the patient performs autonomously (without difficulty); and, for the Barthel test were taken the independence in daily living activities. The scores of both measures fit the normal curve per the z Kolmogorov Smirnov statistic (p> 0.05).
Descriptive results presented in Table 2 and in Figure 4 indicate high growth rate until post-treatment, but on the follow up the growth rates are negative in both variables; being higher in the Lawton test. The ANOVA of repeated measures results indicate that there are not significant differences for neither of the tests scores (Lawton: F2,33 = 0.077; p> 0.05; Bartel: F2,33 = 0.065; p> 0.05) between the three measurements.
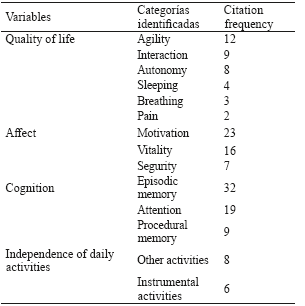
Evaluation of Yoga program effect through focus groups
Results from content analysis of four focus groups with patients and four groups with caregivers, prior consensus among researchers, show that the higher number of occurrences referring to positive change are in the categories of episodic memory, motivation, attention, vitality and agility (see Table 3).
DISCUSSION
This work was done to provide useful evidence in regards with management alternatives for AP and indirectly to their families. Its aim was to establish the effect of a Hatha yoga program in elderly diagnosed with Alzheimer on their quality of life, depression, attention, memory, global cognitive functioning, and independence in basic instrumental functional activities.
The results of the inferential test of repeated measures variance analysis did not show statistically significant evidence for any of the quantitative measurements obtai ned from patients on pre, post-treatment and follow-up; however, it observed a convergence trends in all variables measurements. This would suggest a possible improvement as effect of the program that in clinical terms could have a positive impact on patients' quality of life; although it is possible that trends are only effect of participant's subjective perception. The lack of a control group limits the scope of these inferences.
The trends outlined are consistent with the information provided by the focus groups that constitutes a complementary source of information to detect changes perceived from patients and caregivers regarding with have been participated in the program. Despite cognitive impairment showed by patients (mild to moderate dementia), their reports on the effect of the program were consistent with the perceptions reported by their caregivers, an aspect that should be considered important to understand what means living with dementia, and implies that should be taking patients direct experience (Fromholt, Telenius, Engedal & Bergland, 2015).
Quality of life was assessed by two instruments the ADQRL and CV; the scores mean obtained with both tests have a positive convergence trend during the program and it presents a negative trend of convergence after the program end. This pattern is repeated with depression scores (Yesavage); although variation in these scores does not means changes in mood. The pattern mentioned is repeated in the scores on independence of daily activities measured by Lawton and Brody and Barthel tests; and so does with the attention and memory variables, measured by the Digit Symbol Test and Trail Making Test Form A, and with global cognitive functioning variable that was evaluated, with the MMSE.
This would suggest, despite the limitations imposed by not having a control group, that could have occurred a deterioration attenuation with a slight improvement in the patients' capacities which has a positive effect on maintaining their quality of life, attention, memory and independence of daily activities. Possible causes of this concomitant improvement regarding to the Yoga program could be the increased production of endorphins that favors a positive mood and feelings of well-being, as well as strengthening of physical qualities such as strength, balance and coordination that allow better and more functionality in daily activities (Pérez & Cancela-Carral, 2008). However, the effect of endorphins is transitory (Maggouritsa et al., 2014), findings that are consistent with the results of this study.
Moreover, maintaining the mentioned abilities it could also be caused by repeated practice of yoga postures since the research findings suggest that higher and consistent levels of physical activity are associated with an increase in cerebral blood flow and therefore a lower risk of cognitive impairment (Chapman, Marshall, Strine, Anda & Moore, 2006). On the other hand, several studies have shown that the underlying and responsible neuroanatomical procedural memory system is independent of declarative memory and therefore, patients with Alzheimer's may acquire motor, perceptual and cognitive abilities; therefore, the preservation of implicit memory and procedural learning can occur until disease later stages (Peraita & Moreno, 2006), a situation that could be related to the opportunity to learn a routine of physical activity that involves the performance of motor skills which is implicit in the yoga program. To promote the permanence of the observed positive effects during the intervention phase, it would be appropriate that in future studies the patients were exposed to brief maintenance sessions after post-treatment test.
The above described trends are consistent with previous evidence (Coelho et al., 2012; De Andrade et al., 2013; Khoo et al., 2014. Fan & Chen, 2011; Winchester et al., 2013). However, none of these studies took follow-up measures that would allow to answer the questions on the effect achieved maintenance and evidenced by the post-treatment measurements. Moreover, the study results of Cramer et al. (2014) are consistent with the pattern of the results obtained in our follow-up measurement that could be compared with their long-term measurement. Finally, the results reflected in the study of Sharma, Robbins, Wagner and Colgrove (2015) with patients with Parkinson's disease, are consistent with the findings of this study, in the sense of considering the subjective perception of participants as an indicator of yoga effectiveness.
The Hatha yoga program under evaluation, established a routine of physical activity of two hours per week, with the standing invitation to caregivers to do at home one or two more sessions weekly with patients, in view of the recommendation US Department of Health and Human Services (2008) to practice aerobic exercise at least 150 minutes per week; however, this did not happen in our research and overall patient's physical activity was limited to the two sessions held in company with the instructor. In this sense, the results obtained in terms of the absence of statistical significance by repeated measures ANOVA on the target variables could be explained due to physical activity intensity on weekly basis was not enough to achieve an effective impact on these variables that is one of the limits of this research.
However, from the experience gained from this intervention program, some guidelines could be considered in physical activity future research and intervention propo sals for population diagnosed with dementia. Hatha yoga combines the low-impact exercise (requirement postures), breathing and relaxation, besides the attentional demand, so it is an alternative non-pharmacological intervention useful for this population. Although in this study no physical variables such as balance and flexibility were measured, but they were evaluated in the pilot study (Quintero, Rodriguez, Guzman, Llanos & Reyes, 2011) with positive results which also have found other authors (Donohue et al., 2006; McCaffrey et al., 2014; Riley, 2004), therefore, these variables should be evaluated in future studies.
To achieve better effectiveness of the yoga program on the target variables, adjustments would be required in the lifestyle of patients with the support of their caregivers, to maintain a stable practice of physical activity with the standard of 150 minutes per week, and in this way to have a more lasting positive impact on patients, their caretakers and families. However, this may be difficult in the context of this population due to ongoing medical complications that usually present as well as emotional changes, and the caretaker's attitude and occupations; aspects that in this study could be responsible for the attrition of patient's sample. Moreover, interventions aimed at promoting behaviors and healthy lifestyles as well as preventive behaviors should also be target to healthy population, such as caregivers.
In this study, unlike the pilot study (Quintero et al, 2011), qualitative measures and mixed methods that allowed us to observe a convergent trend as effect of the program, despite the sample characteristics, and the exercise intensity that was less than the standard proposed by literature. It is necessary for further investigations consider the methodological limitations of this study as they are: (a) the lack of a control group to assess the impact of disease deterioration in the experimental group, (b) have a larger sample to reduce the impact of attrition and achieve better statistical power in the data analysis.
Additionally, a new study that evaluates the effect of a Hatha yoga program in patients with AP, it should include at least three sessions per week of one hour, either in company with the instructor or with the support of a virtual technology that serve to encourage, guide and give feedback, and even to offer opportunity to interact with other people doing the same activity. Finally, in order to measure more accurately the changes produced by the Hatha yoga program, it would be appropriate to include measures of physical variables such as balance and flexibility, as well as measure the cortisol level because of the evidence in the literature of its association to negative affective states.











 text in
text in