INTRODUCTION
Diabetes mellitus (DM) represents a serious problem for the health care system (Organización Mundial de la Salud [OMS], 2014). Worldwide, its incidence to date is 347 million diagnosed cases. A prevalence of11.7% among the population between age 20 and 79 is estimated in Mexico, and it is the main cause of death among the economically active population from age 45 to 64 (International Diabetes Federation, 2014). The OMS (2014) has stated the convenience of modifying unhealthy lifestyles in order to prevent and control Type 2 Diabetes Mellitus (Type-2 DM). Keeping the disease in check requires active participation from the patient, since the efficacy of the treatment cannot be fully controlled by the medical staff, and so the patient is directly responsible for the success of the treatment (Amador-Díaz, Márquez-Celedonio & Sabido-Sighler, 2007).
Regrettably, self-care is less than enough among Mexican population with Type-2 DM (Compeán, Gallegos, González & Gómez, 2010; Hernández- Romieu, Elnecavé-Olaiz, Huerta-Uribe & Reynoso-Noverón, 2011). People do not practice self-care behaviors to guarantee their well-being in general terms, and the only indicators of self-care available are the patient's attendance to appointments and whether they take their medication or not, whereas essential behaviors such as the modification of unhealthy habits are overlooked (Amador-Díaz et al., 2007; Compeán et al., 2010; Romero, Dos Santos, Martins & Zanetti, 2010).
Some authors (Hernández- Romieu et al., 2011) have concluded that the problem has multiple dimensions, since there are factors that compromise self-care, such as the time elapsed since diagnosis, age, access to quality medical attention and information, and quality of life, along with the patient's attitude toward focusing their behavior on positive behavior changes and consistent medication intake. There is evidence that the degree of self-care achieved is strongly associated with doctor-patient dynamics and perceived family support (Hoyos, Arteaga & Muñoz, 2011; Wilkinson, Whitehead & Ritchie, 2014); additionally, the level of knowledge about the disease is indispensable to anticipate health-protective behaviors (Bustos, Bustos, Bustos, Cabrera & Flores, 2011; Vargas, Pedroza, Aguilar & Moreno, 2010).
Sarkar, Fisher and Schillinger (2006) pointed out that self-care practices depend on the patient's motivation and will, as well as their coping skills, self-efficacy and perceived resources (Rose, Fliege, Hildebrandt, Schirop & Klapp, 2002).These researchers postulated that the sense of lost health resulting from the disease, together with the inconveniences and the cost of the treatment, increases the risk of anxiety and depression and the evaluation of personal resources to face the disease is negatively affected as a consequence (Browne, Nefs, Pouwer & Speight, 2015; Gonzalez et al., 2008; Nicolucci et al., 2013).
Explaining low self-care behavior in people with Type-2 DM entails thoroughly identifying the determinants of such behavior, which become risk factors to the adequate maintenance of one's health, since they are perceived as barriers to an effective personal management of the disease (López & Ávalos, 2013; Martín, 2003).
Given that chronic diseases are multifactorial in origin and treatment, prevention and control of such diseases need to be approached from a biopsychosocial perspective where all the relevant factors in connection with patients ' lifestyles are taken into account (Lalonde, 1974; Organización Panamericana de la Salud [OPS], 2014). The health psychology model states that people's health status and quality of life during a disease is a result of the interaction individuals establish with their environment. Environmental, personal, and cultural risk factors have an impact on human behavior, which in turn has a direct effect on the affective, cognitive and behavioral responses of all the participants in any health-disease process (Martín, 2003; Oblitas, 2008).
Achieving self-care among population suffering from Type-2 DM is a complex endeavor. Despite the availability of effective treatments, people fail to adequately adhere to such treatments and consequently start to present medical complications which have an impact on their quality of life and lead them closer to premature death (OMS, 2014). Given that the quality of life experienced during chronic diseases is, to a certain extent, determined by effective and sustained personal care, realizing and measuring conditions and factors affecting self-care behaviors is important. To this end, the present study sought to identify sociodemo-graphic and psychological variables related to self-care behavior and quality of life in Mexican adults with Type 2 Diabetes Mellitus
METHOD
Participants
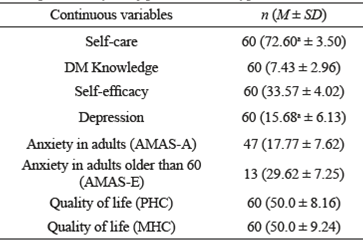
This study used a convenience sampling method with the following inclusion criteria: Mexican adults diagnosed with Type-2 DM more than six months before the study, registered at the Mexican Health Institutes (Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE, for its Spanish acronym) or Centro de Salud Jurisdicción N° 1 (SS, for its Spanish acronym)). All participants signed an informed consent form. The sample was composed of 60 people (93% women), with 10.32 (± 7.05) years since diagnosis. Schooling levels were as follows: no schooling 5%; up to 12 years of schooling 70%; 13 or more years of schooling 25%. Table 1 shows the descriptive analysis.
Instruments
Quality of life. The Short Form Health Survey (SF-36) measures perceptions about quality of life as related with health (HRQL), from two different approaches: physical health component (PHC) and mental health component (MHC). The results from its 36 items are represented with a 0 - 100 scale. The survey has an adapted for Mexico and standardized version, with reliability coefficients between α=.56 and α =.84 (Zúñiga, Carrillo-Jiménez, Fos, Gandek & Medina-Moreno, 1999). For the sample in this study, reliability ranged from α =.65 to α =.88.
Self-care. The Escala para Estimar Capacidades de Autocuidado (EECAC, for its Spanish acronym) measures perceived self-care skills and capabilities in general population. It consists of 24 test items, and the transformed scores range from 0 to 100 as related to a reference group. The EECAC was validated for Mexican population by Gallegos (1995); reported reliability was α=.81 (Landeros, 2003). A reliability of α =.82 was estimated for the sample in this study.
Knowledge about diabetes. The Diabetes Knowledge Questionnaire (DKQ-24) uses 24 test items to assess familiarity with diabetes. An internal consistency of α=.78 has been reported for the test, as well as construct validity, as demonstrated by its sustained sensitivity after a three-month intervention (García, Villagómez, Brown, Kouzekanani & Hanis, 2001). After an analysis, the present study ruled out 10 of the test items. Kuder-Richardson's formula 20 was used to estimate the internal consistency of the instrument after the items were removed, and a reliability coefficient of KR20=.78 was found.
Self-efficacy. The Escala de Autoeficacia General (EAG, for its Spanish acronym) evaluates the individual's perception of their own capabilities to deal with situations. It consists of 10 test items, whose summation ranges from 10 to 40 points and are interpreted based on a reference group. The theoretical validity ofthe construct was studied by comparing two countries (Mexico and Spain); the validity reported for Mexico was α=.86 (Padilla, Acosta, Guevara, Gómez & González, 2006). A reliability of α=.69 was estimated for the sample in the present study.
Depression. Beck Depression Inventory- Second Edition (BDI-II) evaluates depression intensity as a function of the disorder's symptomatic criteria. Total score ranges from 0 to 63 points, and the inventory consists of 21 test items. The adaptation in Mexican population reported a scores between .87 and .92 (González, Reséndiz & Reyes-Lagunes, 2015). The results obtained with the sample used by the present study indicated a reliability of α=.86.
Anxiety. The Adult ManifestAnxiety Scale-Adult Version (AMAS-A) and the Adult Manifest Anxiety Scale-Elderly Version (AMAS-E) (Reynolds, Richmond & Lowe, 2007), evaluate the level of anxiety in individuals by means of 36 and 44 test items respectively. They were validated and standardized for Mexican population with reliability coefficients between α=.62 and α=.68 (Reynolds et al., 2007). For thisstudy, reliability coefficients of a=.88 for the AMAS-A scale and a=.91 for the AMAS-E scale were obtained.
Procedure
After the protocol was presented and subsequently approved by the ethics committees in the public health organizations where the study was carried out, the participants who met the inclusion criteria were summoned. By means of a direct interview, all participants were informed about the purpose of the study, the contents of the measurement instruments, data confidentiality and ethical use of the results. The informed consent forms were signed by the participants, and sociodemographic data were collected inside the facilities of the participants' health care institutions. The battery of six psychometric tests was individually administered to the participants during a 45-minute session performed by the same member of the research group.
Data analysis
The data were statistically analyzed using the R software version 3.1.0 (Ihaka & Gentleman, 1996). Significance level was a priori set at 0.05. With the purpose of evaluating the influence of demographic factors, quality of life, knowledge about diabetes, self-efficacy, depression and anxiety on self-care, a backward stepwise multiple regression analysis based on the maximum model was performed (Venables & Ripley, 2003). Residual variance normality and homogeneity were estimated by the Shapiro-Wilk and Brown-Forsythe tests, respectively (Heiberger & Holland, 2004). The same analysis was carried out regressing all the variables under study including self-care to explain quality of life. The assumptions of homoscedasticity, normality, and self-correlation were verified.
Ethical considerations
Ethical practices were guaranteed by following the guidelines in the protocols used by the ethics committees with the participating institutions, and all subjects were informed about the procedure and purpose of the study and about the confidentiality of the data. The measurements and instruments to be used were also described to the participants. As part of the inclusion criteria used in the present study, all participants signed consent agreement forms.
RESULTS
What follows is a descriptive analysis of the variables measured with the tests administered to the participants; after that, the information about the minimum significant model for the response variables self-care and quality of life will be presented, considering their physical (PHC) and mental (MHC) components. The results for the explanatory variables and their relation with the response variable are also shown.
Self-care
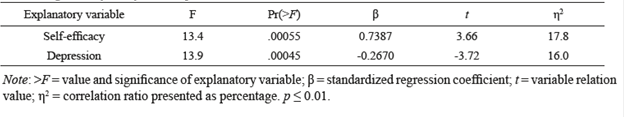
The linear regression analysis (see Table 2) revealed that the minimum significant model explains 33.9% of variance in self-care (F [2, 57]=14.6, p < .05, R2=0.34). The n2 analysis showed that self-efficacy explains 17.8% (β=0.74) and depression explains 16% (β=- 0.27) of total self-care variance; therefore, these variables remain as explanatory variables. Figure 1 shows the relation between both explanatory variables and the response variable.
Quality of life (physical health component)
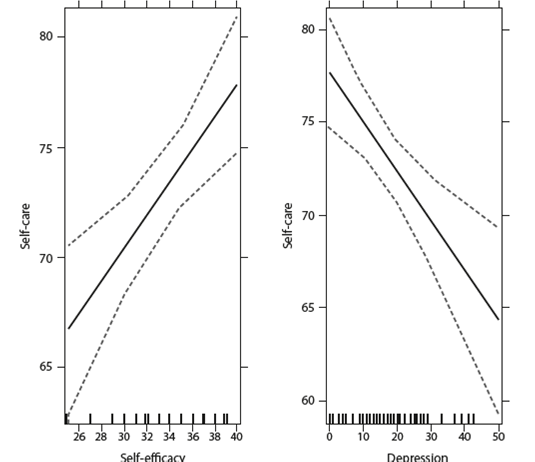
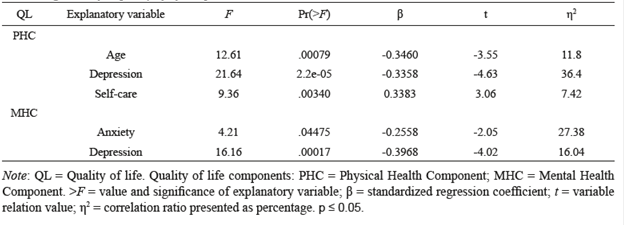
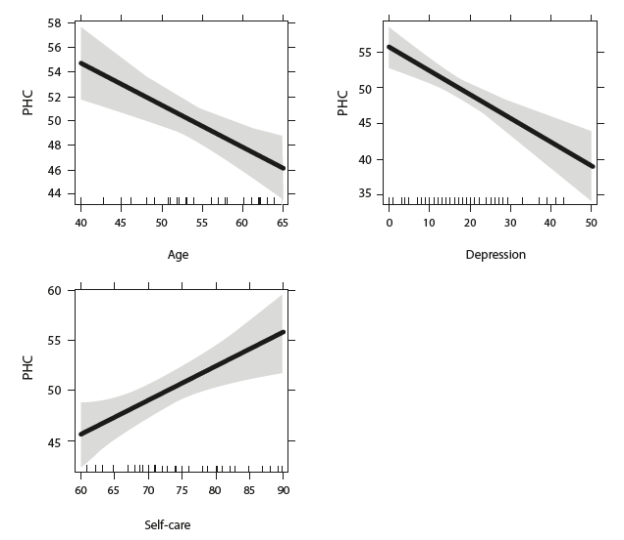
The linear regression analysis (see Table 3) revealed that the minimum significant model explains 56% of variance in PHC (F [3, 56]=23.4,p < .0.001, R2=0.56).
The η2 analysis showed that age explains 11.8%, depression explains 36.4% and self-care explains 7.42% of total variance while every explanatory variable remains unchanged. Figure 2 shows the relationship between the explanatory variables and the response variable.
Quality of life (mental health component)
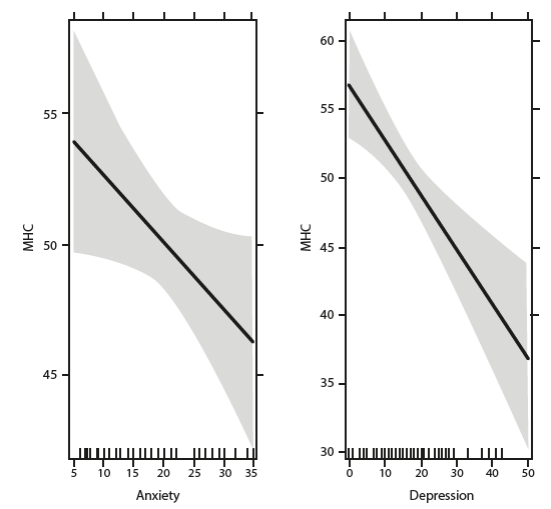
The linear regression analysis (see Table 3) revealed that the minimum significant model explains 43.4% of variance in MHC (F [2, 57]=21.9, p < .0.001, R2=0.434). The η 2 analysis showed that anxiety explains 27.38% of total variance and depression explains 16.04% of variance in MHC, while all explanatory variables remain unchanged.
Note: QL = Quality of life. Quality of life components: PHC = Physical Health Component; MHC = Mental Health Component. >F = value and significance of explanatory variable; β = standardized regression coefficient; t = variable relation value; η 2 = correlation ratio presented as percentage. p < 0.05.
Figure 3 shows the relationship between the explanatory variables and the response variable.
DISCUSSION
The steep increase in the development of comorbidities and premature death associated with Type-2 DM is alarming (OMS, 2014). In view of the evidence of low self-care among Mexican population (Compeán et al., 2010), identifying the sociodemographic and psychological variables that represent risk factors for lack of self-care and HRQL becomes necessary. Besides evidencing variables related to self-care and quality of life, the findings of this study allowed us to showcase the presence and influence of the psychological variables at play during the process of a physical disease.
Among the risk factors measured during this investigation, it was found that a negative perception of self-efficacy is significantly and inversely related to the presence of self-care behaviors. When people suffering from Type-2 DM perceive that they have enough personal and material resources to look after themselves, they tend to increase their self-care behaviors, which impact the therapeutic scope of the treatment, and consequently improve metabolic control (Rose et al., 2002; Sarkar et al., 2006).
The development of comorbidities, not only physical but also psychological ones, is expected during the course of a chronic disease as a result of its evolution and care. The actuality of a diagnosis, the patient's responsibility in their own recovery, and their compliance with treatments alter the person's emotional state, and they begin to develop symptoms associated with depression and anxiety that considerably affect their self-care capabilities (Rivas-Acuña et al., 2011). A poor emotional management in the presence of a chronic disease has a negative impact on the person's well-being and quality of life. As has been demonstrated by the present study, the appearance of depressive symptoms will significantly decrease self-care behaviors, especially treatment adherence (Browne et al., 2015; Gonzalez et al., 2008).
The existence of a chronic disease diagnosis and the many demands of the treatment make it difficult for people to adapt themselves to their new health status, which subsequently leads to a decrease in their quality of life. Studies on people with DM conducted in many countries have reported, as the present study has also found, a reasonably good perception of HRQL (Lau, Quareshi & Scott, 2004; Luyster & Dunbar-Jacob, 2011), yet insufficient as compared to the general population (Graham et al., 2007; Hervás, Zabaleta, De Miguel, Beldarrain & Diez, 2007). For instance, scores reported for Mexican population without a Type-2 DM diagnosis are PHC M=79 (SD=.2) and MHC M=76.7 (SD=.2) (Durán-Arenas, Gallegos-Carrillo, Salinas-Escudero & Martínez-Salgado, 2004); when compared with the results of the present study (PHC: M=50, SD=8.16; MHC: M=50, SD=9.24) those results show statistically significant differences for PHC (t (59)= 27.53, p < 0.001) and also for MHC (t (59)= 22.38,p < 0.001), which confirms that HRQL decreases considerably when a chronic disease such as Type-2 DM has been diagnosed.
As reported by other studies (Al Hayek, Robert, Al Saeed, Al Zaid & Al Sabaan, 2014; Hadi, Ghahramani & Montazeri, 2013; Newmann et al., 2014; Nicolucci et al., 2013) this research has shown that multiple personal variables such as self-care behaviors and the presence of depressive and anxiety symptoms, paired with sociodemographic factors such as age are significantly related (p < 0.001) with the mental and physical components of HRQL. In this regard, the DAWN2TM study (Nicolucci et al., 2013) showed that people with Type-2 DM perceive their quality of life as poor, and determined that anxiety and depression have a strong influence on such assessment.
This is a source of concern, since the prevalence of anxiety and depression among the general Mexican population is high: 6.8% and 4.8%, respectively (Demyttenaere et al., 2004); the situation worsens when we think that symptoms tend to exacerbate in the presence of a chronic disease and with the length of time since the diagnosis (Tovilla-Zárate et al., 2012). Fabián, Garcia, and Cobo (2010) showed the presence of anxiety symptoms (8%), depression symptoms (24.7%), or symptoms of both disorders (5.4%) in individuals with Type-2 DM, and highlighted that these disorders become obstacles for patients to adhere to medical treatments.
The results presented here evince that a satisfactory HRQL is available for people with Type-2 DM, since HRQL is related, for the most part, with variables that can be changed. The development of positive self-care behaviors is beneficial to physical health. Therefore, as long as people practice behaviors favorable to personal and responsible self-care and their depressive and anxiety symptoms are well managed, they will manifest HRQL. However, given that self-care behavior is determined by a positive perception of self-efficacy and by the absence of anxiety and depression symptoms, the task becomes complex, since, as shown by the DAWN2TM study (Nicolucci et al., 2013) those psychological ailments are not a priority for either the population or the health care system.
These findings become relevant when the variables related to self-care behaviors are revealed; as the results of many other studies have stressed (Compeán et al., 2010; Praveen, & Vittal, 2012), the level of self-care of people with Type-2 DM has an impact on long-term HRQL. Such negative impact is thus a result of poor self-care along time, which brings ill consequences to people's physical, social, and mental health. In Mexico, Type-2 DM is the first cause of disability, and it represents a considerable decrease in the number of years of healthy life that can be achieved without losing autonomy and functionality (Gómez Dantés et al., 2011).
When people face inevitable health complications, they not only impoverish their quality of life, but they also represent a serious coverage challenge for health care systems. The economic expenditure on DM in Mexico is already high, but in the future it will become insufficient, since the costs generated by the growing number of referrals due to increased incidence of DM and its comorbidities, low treatment adherence, and subsequent failure of the whole treatment are beyond the human and economic resources that could be allocated to health care (Arredondo & De Icaza, 2011).
Every person practices self-care to a certain extent, but sometimes that is not representative of the range of behaviors necessary to meet the demands of their health status. It is necessary to highlight that failing to initiate personal actions as well as actions involving the family and the health care system will make the personal attempt to manage the disease the main risk factor for experimenting poor quality of life (Nicolucci et al., 2013).
A limiting factor in the present study was the size of the sample, which could not allow for the generalization of the results. For future research in the area, we recommend the exploration of variables related to coping skills, motivation, social support and doctor-patient relations. Objective measurements by means of standardized tests with validation for the target population are also recommended, as well as the measurement of biochemical variables.
The methodological strength of this study is the simultaneous measurement of several variables that have been considered risk factors for lack of self-care and quality of life. Concerning clinical implications, it was found that psychological aspects such as depression and anxiety coexist with Type-2 DM, inhibiting self-care behavior and consequently deteriorating HRQL. It is also important to point out that programs addressing chronic diseases neglect the presence of mood disorders and their influence on the continuation or modification of risk behaviors (OMS, 2014). The results in this paper present useful information to be used in the design of interventions aimed at improving well-being and quality of life by engaging the adequate management of emotions as an intervention strategy and by having effective self-care as the foremost goal.











 texto en
texto en