Background
Widespread use of combined highly active antirretroviral therapy (HAART), has improved HIV positive(HIV+) patients survival over the last decade1,2. Life expectancy has grown at least fifteen years in people living with HIV3, increasing patients lifespan4. In developed countries, almost half of deaths in HIV+ individuals with HAART therapy have a closer relationship to external factors than HIV infection itself5. For low-middle income countries where HAART coverage also is increasing, stemmed from a mix of chronic immune activation, medication side effects, coinfections, and the aging process itself, pose many challenges for addressing HIV as a public health problem6.
Longtime exposure to HAART may increase the risk of metabolic complications7, cardiovascular diseases8, hypertension9, hyperlipidemia10, renal disease11, reduced bone mineral density12 and drug-drug Interactions13. Comorbidities can occur not only related to HIV therapy and concomitant medications but to the infection itself; indirect causal relationships may appear because of risk factors shared among diseases14. In parallel, with survival increase of HIV+ patients, there has been a rise in the burden of AIDS and non-AIDS comorbidities, including overrepresentation of traditional risk factors15, and chronic immune activation and inflammation16.
Therefore, there is a need for a change in the clinical management and treatment of HIV infection, a situation that will put new demands on the health care system to evaluate the burden of disease and risk factors involved among people living with HIV17. The goal of this study was to determine the prevalence of comorbidities in a group of HIV+ patients attending two urban-based clinics in Colombia, as well as identify risk factors associated to variation in comorbidity-free years of this population, according to their age and whether they receive treatment or not for those comorbidities.
Material and methods
This was an observational, retrospective medical chart review study of adult HIV+ patients. A convinience sample of 669 medical charts were selected from HIV+ adults 18 years and older during the reference period (from July1, 2014-July30 2015), who were receiving medical care in two HIV clinical facilities: Recuperar: (“Centro de Medicina Física y Rehabilitación Recuperar SA IPS”), located in Cali, and SIES: (“Sociedad Integral de Especialistas en Salud SAS), that serves patients from Bogotá; Armenia and Medellin. The following patient data were collected from each clinical chart: sex, age, weight(Kgs), Body Mass Index (BMI) and documented diagnosis of one of the following conditions (clinical diagnosis previously reported by the health care professional in the clinical chart): type 2 diabetes mellitus(T2DM), dyslipidemia, high blood pressure, overweight, depression, lipodystrophy and use of tobacco, drugs and alcohol. In adittion, past or current use of prescription or over the counter drugs related to comorbidities were recorded from the same source. Score on the Framingham risk scale was also included 10. The study was submitted to the local institutional ethics committee “CAIMED” and approved in 2016.
Inclusion Criteria
Active charts of adult HIV+ patients, who were 18 years or older at the beginning of the reference period who had been receiving health care at that clinic for at least six months or longer.
Statistical analysis
Summary statistics for demographic and clinical characteristics, considering those patients who received or not treatment for their comorbidities and were under or over 50 years old. We examined the relationship between comorbidity-free years (time to diagnosis once entered to the cohort) through Kaplan-Meier bivariate analysis18 and Cox regression19. Potential confounders in the multivariate analyses were: age, sex, tobacco or alcohol use. The statistical package used for the analysis was STATA V.14.020.
Results
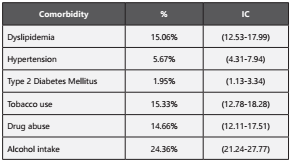
A total of 669 medical records were reviewed, 16.14% were 50 years or older and 476 (71.15%;95%CI:67.59%-74.46%) were males. 337 patients (50.37%) and 332 (49.63%) (p=0.846) were from Recuperar and SIES, respectively. Of the patients, 2.55% (95%CI:1.59%-4.07%) were overweight. Table 1 shows the percent distribution for the most common comorbidities. The most common comorbidity was dyslipidemia, followed by hypertension and T2DM. Table 2 shows information of patient characteristics by age (50±), receiving treatment for any comorbidity and center. Patients 50 years or older were more likely to have dyslipidemia, hypertension and T2DM than those under 50 years old. They were also more likely to have any comorbidity, and to have more years since HIV diagnosis and since starting treatment for HIV.
Table 2 Patient characteristics by age group (50±) and receiving treatment for any comorbidity. Variable Age Group Receiving T
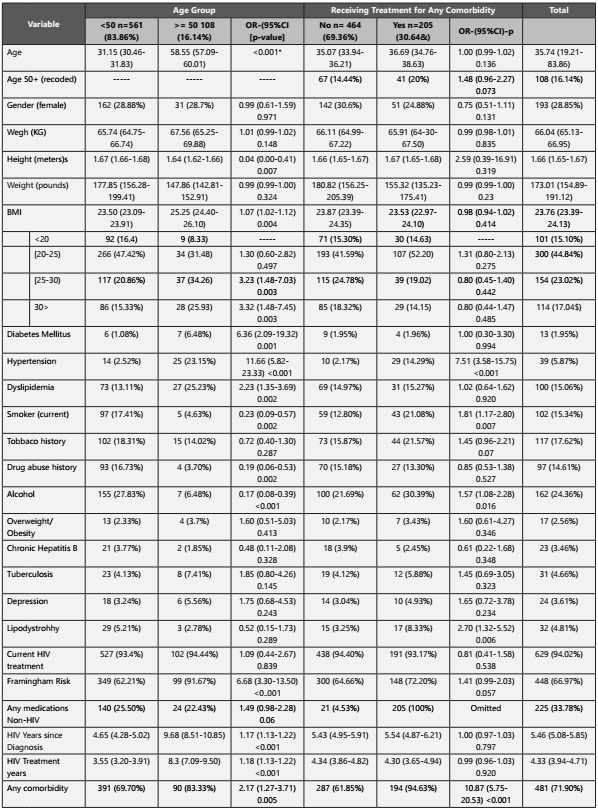
Regarding Framingham scale, the average score was 4.62(95%CI:3.91-5.34low risk). About medication use, 0.91%(95%CI:0.4-2.01%) of patients used anti-hyperglycemic agents, 5.77%(95%CI:4.22-7.84%) lipid lowering therapy, 3.95%(95%CI:2.7-5.74%) antihypertensive medication, 2.58%(95%CI:1.61-4.12%) proton-pump inhibitor, 0.6%(95%CI:0.22-1.61%) H2 blockers, 0.75%(95%CI:0.31- 1.81%) antacids, 0.91%(95%CI:0.4-2.01%) asthma medication, 5.31%(95%CI:3.83-7.32%) dietary supplements, and 25%(95%CI:21.82-28.46%) any other medication.
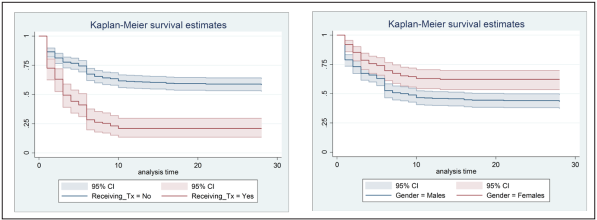
Average time from HIV diagnosis and starting treatment was 5.46 years (95%CI:5.08-5.85years) and 4.33 years (95%CI:3.94- 4.71years), respectively. 468 (69.96%) had at least one comorbidity with an average comorbidity-free time of 9.7 years (95%CI: 8.76-10.64). Females were found to live significantly more time with no comorbidities when compared to males 13.24years (95%CI 11.38-15.11 years) vs. 8.26 years (95%CI 7.21-9.32years), respectively(p<0.001).
A total of 6,492 patient-time years were analyzed to assess comorbidity-free years. Significant differences were observed when comparing patients under 50 years old with those 50 years and older: 136 events observed (comorbidities) versus 51 (p=0.001). Comorbidity-free years curves by of those receiving treatment versus those not receiving treatment and gender are shown in figure 1.
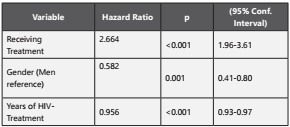
Older patients have had more opportunity to receive long-time HIV treatment due their age. Thus the more years on treatment, the less expected comorbidity-free years. Treatment administration was positively associated with risk of having co-morbidities, most likely due to the fact that once patients are diagnosed of any comorbidity, they may require chronic medication. Proportional risk assumption was adequately verified (p=0.200). Significant effects are showed in Table 3.
Discussion
This study included patients from two specialized HIV treatment centers. Patients over 50 years or with long-term medication use had a significantly higher risk of comorbidities. Women were at lower risk. 71% of the patients had at least one comorbidity, the most frequent of which were dyslipidemia, hypertension, lipodystrophy, tuberculosis and depression. Results are similar to other studies previously reported12.
Regarding age groups, significant differences were observed for those 50 years or older compared to younger counterparts regarding frequency of BMI, diabetes, high blood pressure, dyslipidemia, and tobacco, alcohol and drug use, as well as for the Framingham risk score21. These conditions are common in this population, regardless of HIV status, and are related with other symptoms, not recorded here, like decreased sexual desire, back pain, avoiding intimacy, skin changes and few help-seeking attitudes22. Women were found to have longer comorbidity-free periods, probably related to better health-seeking behavior as it has been reported before23.
Our results showed a significant association with life-style factors, such as smoking and alcohol use with lipodystrophy. This is probably related to psychological distress, economic or autonomy deprivation in HIV+ patients; however, this kind of outcomes has not been adequately studied in low-income countries24. Furthermore, receiving treatment acts like a risk factor for reducing time living free of comorbidities, probably because co-infections and side effects are prevalent among HIV+ patients attending healthcare facilities, or patients requiring some medications can exhibit a more complicated health condition or not healthy life-styles25.
There are several limitations for this study. First, it is a not general population-based study where only two care centers were included by means of a convenience sampling scheme. Therefore, the results may not be representative of all the people living with HIV in Colombia. Second, the information examined here is mainly from laboratory data that were accumulated during the clinical care consultation. Some other comorbidities were not systematically examined, such as malignancy. Third, we did not have an HIV(-) population for comparison in terms of the frequency of comorbidity. Therefore, it is not known whether the frequency of any comorbidity examined in this study is higher in HIV+ patients than in HIV(-) ones, although several studies have suggested that HAART and HIV infection may accelerate aging and increase risk of metabolic, cardiovascular and other chronic complications26. Finally, a high percentage of unrecorded data was found in the review of clinical records, which is why greater emphasis on clinical record documentation is recommended. Notwithstanding, this study serves to draw attention to the need to strengthen the comprehensive approach of the HIV+ patient, in addition to drawing attention to greater control of the clinical records.
These findings are consistent with previous reports and lead to consider the underlying processes the patients with HIV live with, producing multiple comorbidities, in particular chronic ones. This can be due to several factors, including poly-pharmacy, adherence, lifestyle behaviors, and drug-drug interactions. Comprehensive approaches to the management of other than HIV-related problems in the long-term are needed in HIV+ population27.
In conclusion, our results show that a significant proportion of the HIV+ people have multiple comorbidities that may in crease risk of other complications or reduced years free of illness and life-span. Issues of poly-pharmacy among the adults VIH+ need to be addressed to ensure adherence and minimize drug-drug interactions. Other preventive actions and initiatives are also recommended taking into account the similarity of some risk factors and the psychological and functional impact on this population28. Comprehensive approaches to the management of metabolic, cardiovascular and, in general non-communicable diseases are required in the long-term successful management of HIV+ elderly population.