Background
Acute mediastinitis (AM) is the inflammation of the connec tive tissue and fat surrounding the mediastinal structures. It is a high-mortality entity, more frequent in young people and predominantly in males1-4. Conditions associated with AM are variable and include: postoperative complications from ster notomy, head and neck infections, esophageal perforation and extension of osteomyelitis of underlying structures1,5,6. Isolated cases of AM by hematogenous dissemination have been described6,7). The identification of suggestive findings in the images in a context of compatible clinical manifestations and associated predisposing factors, result in an AM diag nosis. The early surgical approach is the cornerstone in the management of the entity6,8.
Case presentation
58-year-old man with history of gouty arthritis self-medi cated with steroids and NSAIDs (Dexamethasone 8 mg and diclofenac 75 mg intramuscularly every 3-4 days) for approxi mately 10 years. He consulted the emergency department due to polyarticular pain, fever, asthenia, adinamia and in flammatory changes in the medial region of the leg and left internal malleolus with a 15-day evolution. Upon admission, fever and soft tissue swelling in the ankle were evidenced, associated with leukocytosis with neutrophilia and an in crease in the amount of inflammatory phase reactants. Due to the suspicion of septic arthritis, antibiotic treatment with Piperacilin Tazobactam and Vancomycin was initiated (after the collection of blood cultures) (Table 1 and 2). X-rays of the left knee and ankle did not show any alteration in the bone structures. Magnetic resonance imaging (MRI) of the left leg showed collection in the anteromedial region of the left thigh, between the planes of the adductor muscles and the vastus intermedius. In blood cultures, methicillin-sensitive Staphylo coccus Aureus was isolated after 24 hours. Transesophageal echocardiogram ruled out vegetations or thrombi, valvular alterations and showed preserved systolic and diastolic func tions. Two days after admission, left ankle arthrotomy and abscess drainage were performed in the dorsum of the foot and anteromedial region of the left thigh.
Table 1 Results of blood tests carried out during the course of the illness. 1: admission paraclinical evaluations, 2: 48 hours later and 3: 72 hours after admission.

Table 2 Results of paraclinical evaluations performed during hospitalization.

ALAT: alanine aminotransaminase, ASAT: aspartate aminotransferase, TP: prothrombin time, BUN: blood urea nitrogen, CRP: C-reactive protein, HBA1c: glycosylated hemoglobin, HIV: human immunodeficiency virus.
Due to clinical deterioration, complementary studies were carried out, including: thorax radiography in which me diastinal widening was evidenced (Fig 1) and computerized tomography (CT) of the chest that defined mediastinal co llections with air bubbles inside, alteration in mediastinal fat density and pleural effusion (Fig 2). With tomographic ima ge suggestive of mediastinitis and signs of clinical deterio ration, mediastinal collection drainage was performed with right thoracoscopic approach (two ports, in supine position), with initial finding of serohematic pleural effusion (500 cc). Initial opening of anterior mediastinal pleura, with drainage of purulent collection of 100 cc and mediastinal fat necro sis. In the debridement the superior vena cava was injured and repaired. Subsequently, the posterior mediastinal pleura was opened, with drainage of 300 cc of purulent material, followed by washing and drainage of mediastinal spaces with thoracostomy tubes.
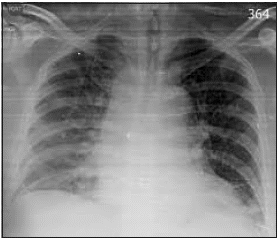
Figura 1 Portable Chest X-ray. Mediastinum widening. Opacity of the right hemithorax related to pleural fluid.

Figura 2 Chest CT scan. A and B. Axial cuts. Transcompartmental mediastinal collections, with air bubbles and increased mediastinal fat density. Free bilateral pleural fluid, of greater right volume. C. Coronal reconstruction. Anterior mediastinal collection (retrosternal).
Extension studies showed no infection in face, or neck com partments. Methicillin-sensitive Staphylococcus aureus was isolated in all cultures.
The clinical evolution after drainage of infectious focuses and antibiotic therapy was satisfactory with oxacillin at a dose of 2 grams every 4 hours intravenously for 3 weeks.
Discussion and conclusions
Mediastinitis is the inflammation of the connective tissue and fat surrounding the mediastinal structures. The entity is asso ciated with high mortality (12 to 47%)1-3,9) and mainly affects young people, with higher prevalence in men (4:1 ratio)4. Mediastinitis is classified into acute and chronic. In general, acute mediastinitis (AM) is related to bacterial infections and chronic mediastinitis (CM) is associated with granulomatous infections such as histoplasmosis and tuberculosis. The con ditions most frequently associated with acute mediastinitis include: postoperative complications of sternotomy (mainly cardiovascular surgery), head and neck infections (descen ding necrotizing mediastinitis), esophageal perforation (spontaneous, foreign-body, or iatrogenic), and extension of osteomyelitis from adjacent bone structures (sternum and sternoclavicular joint)1. Isolated cases of mediastinitis due to hematogenous dissemination have been described7.
The diagnosis of AM associated with deep sternal wound in fection is considered in patients with fever, chest pain or ster nal instability and purulent discharge from surgical wound, mediastinal widening in imaging studies, microbiological isolation in mediastinal cultures, or histological findings of mediastinitis3. The incidence of AM associated with sterno tomy is reported to be between 0.5% and 2.2% of cardiac surgeries, with mortality up to 14%10. Risk factors for sternal infection following cardiac surgery have been identified, such as advanced age, obesity, renal impairment, diabetes, hyper glycemia in non-diabetics3, heart failure, chronic obstructive pulmonary disease, smoking, ventricular assist devices, fema le gender11, nasal colonization by S. aureus5, and early percu taneous tracheostomy12.
AM associated with esophageal perforation presents a cli nical triad of retrosternal pain, vomiting and subcutaneous emphysema and is associated with close to 20% mortality. In relation to esophageal perforation, it can be related to fore ign bodies (fishbone or chicken bone) or iatrogeny (endos copic or transesophageal procedures); it is characteristically located in the Killian triangle, the cricopharyngeal region and the esophagogastric junction. Other causes of AM associated with esophageal perforation include spontaneous perfora tion or Boerhaave’s syndrome (8-33%), neoplasms (20%)13,14, penetrating trauma, and the dehiscence of esophageal anas tomosis sutures (30%)5.
Necrotizing descending mediastinitis (NDM) is defined as the extension to the mediastinum of head and neck infections. The initial clinical manifestation corresponds to the base en tity and later on it is treated with systemic manifestations.
Neck collections can condition airway obstruction by extrinsic compression. The extension to the mediastinum of cervical infections can be anterior, lateral or posterior (through the retropharyngeal space). The most frequent causes of NDM include odontogenic focus infection (36%-47%), pharyngeal infection (33%-45%) and cervical infection (15%). The mor tality associated with NDM varies between 15% and 30%4,15. The risk factors associated with the entity are considered diabetes mellitus, oral glucocorticoid consumption and heart failure. In 13% of patients no comorbidity or associated fac tors are identified and the microbiological isolation is usually polymicrobial, with a predominance of gram-positive bacte ria, followed by anaerobic bacteria15.
Among the causes of acute mediastinitis, hematogenous dis semination is the one listed most often. There are not avai lable data related to incidence or prevalence of AM of this nature. Isolated reports of AM related to extrathoracic septic arthritis, in intravenous drug users or immunocompromised to a certain degree, are described in the literature. The confir mation of the entity is supported by the concomitant micro biological isolation of the peripheral and mediastinal focus6,16.
In relation to the clinical manifestations of AM, these are va riables and are initially related to the entity or base condi tion; as the disease progresses, hypotension, shock, sepsis and requirement of vasopressors are manifested, identifying the comorbidities (diabetes, obesity, COPD, cardiac surgery, osteoporosis and smoking) as factors that can condition va riations of the clinical condition3.
Radiological alterations are related to the presence of AM and the underlying entity or condition. The imaging ma nifestations common to the different etiologies of AM in clude increased attenuation of mediastinal fat, mediastinal collection(s), extraluminal air, mediastinal lymph nodes, pericardial and pleural effusion. Postoperative AM includes widening of the mediastinal radiolucent band (related to sternotomy diastasis), rupture or displacement of the sternal fixation wires and sclerosis and/or fragmentation of the ster num. The presence of collections or extraluminal air beyond the 14th postoperative day of sternotomy suggests AM6,17,18. In patients with AM secondary to esophageal perforation the main findings are thickening of the esophageal wall, perie sophageal collections, pneumomediastinum and extravasa tion of the contrast medium into the mediastinum19,20. In patients with NDM, alterations in imaging studies correspond to basal infection (collections in the neck compartments), with caudal extension to the mediastinum, subcutaneous emphysema, subcutaneous cellular tissue edema, and mani festations related to mediastinitis6,21,22.
In the management of AM the fundamental pillar is early surgical drainage, with approaches that vary according to the etiology of the entity. Measures of general support are also considered, as well as resuscitation by goals in patients with septic shock, early advanced airway management (in necrotizing descending mediastinitis) and broad-spectrum antibiotic therapy with coverage for Staphylococcus aureus, Gram (-) bacteria, gastrointestinal and anaerobic. There is no consensus regarding the duration of antibiotic therapy. The empirical antifungal coverage decision is recommended if 3 of the following conditions are met: Septic shock, female sex, previous upper gastrointestinal surgery and broad-spectrum antibiotic in the last 48 hours8.
In conclusion, the case presented is relevant because of the low frequency of reports available in the literature of acute mediasti nitis due to hematogenous dissemination. In this patient, the ri gorous search for an explanation for the clinical deterioration in spite of the orthopedic management, a correct interpretation of the images and an appropriate surgical management yielded an excellent outcome in spite of the patient’s comorbidities. Consi dering the high mortality of the entity related in most cases to a late diagnosis, a fast and efficient multidisciplinary exercise that allows opportune management is indispensable.














