Introduction
Scorpionism - a generic name given to accidents with scor pions - occurs commonly in tropical and subtropical regions (Abroug et al., 2020), representing a serious public health problem, due to its high incidence and clinical relevance. Worldwide, it is estimated that in 2019 there were around 1.2 million accidents and 3500 deaths annually (SBMT, 2019). In Brazil, between 2007 and 2018, approximately 927 thousand cases of entanglement by scorpions were reported, resulting in 972 deaths (Brasil, 2019; Furtado et al., 2020).
The main genus of scorpion found in Brazil is Tityus. Tityus se rrulatus (yellow scorpion) the most prone to the production of serious accidents and with potential evolution to death in country (Brazil, 2009). Such scorpions are investigated - for example, in research units, such as the Butantan Institute - with the aim to produce serum to neutralize the action of the venom and to investigate the eviction reactions in human or ganism (Batista, 2016). In about 95% of cases, involvement is restricted to the location where the bite occurs. However, po tentially serious accidents can occur, especially at extremes ages (infants and the elderly) and in those situations in which there is a delay between entanglement and access to hospital care (Abroug et al., 2020; Carmo et al., 2019). Despite the le sions produced by scorpionic toxins, such components have been studied - with promising results - for the treatment of morbid conditions in human medicine.
Considering these brief notes, the present article aims to present the main clinical characteristics of scorpionism, also emphasizing the diagnosis, differential diagnoses, treatment and prevention of this condition.
Scorpions in Brazil
In Brazil there are four scorpion families: Buthidae, Bothriuri dae, Chactidae e Hormuridae (Bravo & Calor, 2014). The Ti tyus genus, belonging to the Buthidae family, presents the biggest species number in the country, totaling fifty-four. Among these species, it is possible to highlight the main responsible for serious accidents in Brazil, such as, Tityus se rrulatus, Tityus bahiensis, Tityus stigmurus, Tityus paraenses and Tityus silvestris (Figure 1 and Figure 2) (Reckziegel, 2013; Kuiava, et al., 2019).
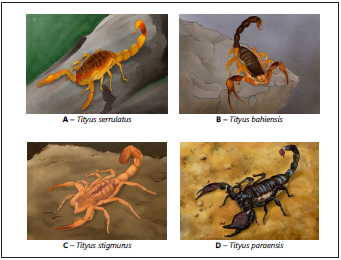
Figure 1 Species of scorpions of medica l importance in Brazil: A - Tityus serrulatus; B - Tityus bahiensis; C - Tityus stigmurus; and D - Tityus paraensis. Prepared by Ademir Nunes Ribeiro Júnior.
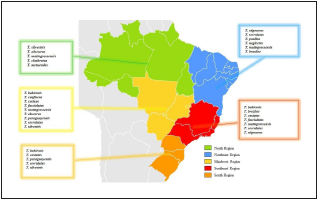
Figure 2 Distribution of the main species of the genus Tityus, in Brazil. Prepared by Ana Clara Miranda Gomes. Sources: Brazil e Porto (2010); Carvalho et al. (2017) ; Lira et al. (2021); Lourenço (2002).
Tityus serrulatus (Figure 1A) species is popularly known as ye llow scorpion due to the yellow color of its legs, pedipalp and metasome. It is approximately 7 cm long, dark brown in color on the back of the prosome and the metasome, and dor sal serration on the 3rd and 4th segments of the metasome, the latter being more robust in the male than in the female. This species’ reproduction is paternogenetic, with the fema le being able to reproduce about 160 offspring throughout her life. This is the species that causes the largest number of serious accidents and deaths in the country. Due to its high and rapid proliferation - and good adaptation to urban environments - it is usually found in the Northeast, Midwest, Southeast and South regions (Brazil & Porto, 2010).
Tityus bahiensis (Figure 1B) - also known as brown or black scorpion - is about 7 cm long, has brown legs and pedipalps, dark metasoma and back of the prossoma and mesosome, legs and pedipalps with dark spots. The male’s pedipalp of the tíbia is larger than female’s. Unlike T. serrulatus, this spe cies has no serrations in the metasome (Puorto, et al., 2017). It represents the second biggest cause of serious accidents in Southeast Region, mainly among children. It is possible to find it, equally, in the Midwest and South (Dias, 2016).
Tityus stigmurus (Figure 1C) is known as a yellow scorpion from the Northeast, it is about 7 cm long, yellow legs, pedipalp and metasome, and, unlike, T. serrulatus, has a longitudinal band, dark on the back of the mesosome, with two smaller bands on the sides, followed by a triangular spot on the back of the prossoma (Puorto et al., 2017). In addition, this species has a dorsal serration in the 3rd and 4th follow-up of the metasome and reproduction is paternogenetic, male has a thinner pedi palp and greater metasome than the female. It can be found in the Southeast and Northeast regions, responsible for the highest number of accidents (Silva et al., 2016).
Tityus paraensis (Figure 1D), popularly known as black scor pion from the Amazon, is black in adulthood and is about 9 cm long. In young phase, it has appendages and brown body, stained with dark, which can be confused with other species of Amazonian scorpions. It is found in the Midwest and North regions, causing many accidents mainly in Pará and Amapá (Brazil & Porto, 2010).
Tityus silvestris is between 2.5 and 4.5 cm long and has a ye llowish-brown color with spots on the body, legs and palps, except for the last segment of the tail and telson. In addition, it has a thorn under the stinger. This species can be found in the Midwest and North regions, especially in Pará and Ama zonas (Coelho et al., 2016).
Biochemistry of venom and scorpionism pathogenesis
It is estimated that there are about 100,000 components in the scorpion venom; however, only a small part of it’s bio chemical diversity is known (Triches, 2017). The constitution of the venom depends on the species, life habits and the geographic distribution of the animals. The venom - usually separated into two parts, a water-soluble and a water-inso luble - is produced in the pair of glands located in the tel son. Only the soluble part is considered toxic, containing in addition to neurotoxic proteins, lipids, enzymes, nucleosides, nucleotides, free amino acids, peptides and carbohydrates. The insoluble portion, on the other hand, is non-toxic, and is composed of mucoproteins and membrane debris (Reckzie gel & Pinto, 2014; Nencioni et al., 2018; Galvani, 2019).
The production and storage of the scorpion venom are as sociated processes with considerable energy expenditure, so that the amount of venom inoculated can be manipulated by the arthropod, according to the threat level (Abroug et al., 2020; Ismail & Abd-Elsalam, 1988). This fact probably expla ins the mild clinical manifestations in 95% of victims stung by scorpions (Abroug et al., 1999; Abroug et al., 2020).
The venom, after being inoculated in a victim, stimulates the sodium channel receptors in nonspecific nerve endings, causing cell membrane depolarization and intense release of catecholamines and acetylcholine, which act in different parts of the body and, consequently, generate the majority of clinical manifestations (Weiss, 2018).
The main manifestation is local pain, which can vary in inten sity and is characterized by a burning or a prickling sensation. Hyperemia, scarification, pruritus, hyperesthesia, paraesthesia, edema, sweating and piloerection are also described (Abourazzak et al., 2009; França et al., 2015; Reis et al., 2019). Some of the clinical findings are the result of the type IV hypersensiti vity reaction, evidencing the influence of the immune system on the development of local symptoms (Reis et al., 2019). One can also mention the action of hyaluronidases and metallo proteinases, which degrade the extracellular matrix of the skin, and vasoactive amines that favor increased blood flow to the affected region, intensifying hyperemia and edema (Abourazzak et al., 2009; Reis et al., 2019; Machado, 2016; Pucca et al., 2015; Rahmani & Jalali, 2012).
To analyse scorpion’s venom, it can be extracted from the telson, through maceration in saline solution or by electric shock. This last method allows the animal to stay alive and only the venom is obtained, unlike maceration. Initially, tox ins from the venom were studied in order to find antidotes for accidents caused by these venomous animals. Subse quently, it was observed that the poison could be used as a medicine, which is still under investigation, as will be seen in part 2 of this manuscript (Hassan, 1984; Oguiura, 2004; Bernardes-Oliveira, 2019).
The components of scorpion venom can be classified into two distinct groups of peptides: (1) those that have a disulfi de bridge in their molecular structure - the bridge-disulfide peptides (PPD) - and (2) those that do not have disulfide bridges in their structure - non-bridge-disulfide peptides (PNPD) (Almaaytah & Albalas, 2014; Furtado et al., 2020). PNPDs are known for their antimicrobial activity, for being bradykinin enhancers, and for modulating the immune res ponse (Almaaytah & Albalas, 2014; Furtado et al., 2020; Zhi jian et al., 2006). PPDs, in turn, are toxic components that act on ion channels, inducing the release of neurotransmit ters, cholinergics and adrenergics, which explain the rela ted symptoms; with sympathetic and / or parasympathetic effects. In addition, the peptides in this group are intrinsically associated with the induction of the inflammatory response (Pucca et al., 2015; Reis et al., 2019).
The main studies about the scorpion venom come from re search on species that cause serious accidents, such as T. serru latus and T. bahiensis (Lourenço & Eickstedt, 2009). The poison that is most investigated is the one of the species T. serrulatus, which some substances are already isolated and recognized.
The neurotoxins Ts1 (TsTX-1 or γ toxin), Ts2 (TsTXIII or III- 8), Ts3 (TsTX or Tityustoxin) and Ts5 (TsTX-V) act by binding to the post-ganglionic sodium ion channels, causing depo larization of membranes by Na + influx. The toxins Ts6 (Ts TXIV), Ts7 (TsTX-Kα or TsII-9), Ts8 (TsTX-Kβ or TsK2), Ts9 (Ts κ), Ts15 and Ts16 act in the post ganglionic potassium ion channels blocking the influx of K + for the cell, concentra ting in the extracellular medium. Therefore, the toxins Ts1, Ts2, Ts3 and Ts5 act in synergy with the neurotoxins Ts6, Ts7, Ts8, Ts9, Ts15 and Ts16 (Brites-Neto, 2019). The Ts4 peptide, also called TsTX-VI, causes hypersensitivity reaction, tearing and dose-dependent release of glutamate and GABA. The T peptide (Ts10) intensifies the activity of bradykinin, that is, the toxin inhibits the angiotensin-converting enzyme (ACE) that hydrolyzes bradykinin and prevents the conversion of angiotensin I to angiotensin II, in addition to inhibiting tissue kinase II. Despite not inhibiting ACE, hypotensins 1, 2, 3 and 4 accentuate the hypotensive action of bradykinin and, conse quently, cause vasodilation (Brites-Neto, 2019).
Typically, the toxicokinetics of the compounds present in the venom are described as rapid absorption and blood distribu tion, high tissue affinity and slow excretion. In young people, absorption and distribution are faster and elimination is slower than in older people. Thus, toxicokinetics depends on the individual’s age group, with symptoms worsening in young and old (Soto-Blanco & Melo, 2018).
Through the activation of Na+ channels, the neurotoxin Ts1 is capable of causing the depolarization of cell membranes and the release of catecholamines (adrenaline and norepinephri ne) and acetylcholine. Catecholamines mainly cause adrener gic effects by stimulating the sympathetic nervous system and acetylcholine stimulates the parasympathetic causing choli nergic symptoms. Catecholamines cause an increase in syste mic blood pressure, constriction of peripheral vessels, cardiac arrhythmias and, occasionally, acute pulmonary edema, heart failure and shock (Siqueira-Batista et al., 2004). Acetylcholine causes an increase in some secretions, such as nasal, lacrimal, salivary, bronchial, gastric and sweat, in addition to muscle spasms, trembles and decreased heart rate (Paz, 2020).
In addition to the neurotransmitters’ release, some venom toxins can directly stimulate sensitive nerves through sodium ion channels, releasing neuropeptides - similar to substance P - which sensitize other nerve fibers distant from the ino culation region and activate NK1 tachykinin receptors. This activation causes contraction of the intestinal smooth mus cle and inflammation. This occurs due to the activation of NK1 receptors in mast cells, which stimulate the release of inflammatory components, such as platelet activating factor (PAF), interleukins (IL-1, IL-2, IL-6 and IL-10) and leukotrienes. These components can cause pulmonary edema, due to in creased pulmonary capillary permeability, and hemodynamic dysfunctions, due to the increase in systemic blood pressure (Soto-Blanco & Melo, 2018).
Clinical aspects
The large number of scorpion accidents and the variety of existing species shows the importance of describing the signs and symptoms of the affected patients. Thus, mild forms up to severe pictures of scorpionism are reported. As the first symptom after the bite is local pain, markedly described among patients with immediate onset and varying its’ inten sity. The pain can be irradiated and accompanied by local or limb paresthesias, erythema, piloerection and sweating. It is the main complaint that motivates the search for medical as sistance, being described by the patient as burning, needles and / or throbbing (Brasil, 2009; Brasil, 2019).
Around two to three hours on average, the venom may cause systemic manifestations due to the sympathetic and parasympathetic excitation (Siqueira-Batista et al., 2004; Bra sil, 2019). Manifestations such as hypo or hyperthermia and deep sweating appear. Disorders of the gastrointestinal tract - such as nausea and vomiting, sialorrhea, abdominal pain and diarrhea - usually come up, and in severe cases, there are reports of acute pancreatitis in patients hospitalized for accidents with scorpions. Cardiovascular alterations are also described, such as bradycardia or tachycardia, hypotension or systemic arterial hypertension, arrhythmias and conges tive heart failure, which can cause acute pulmonary edema (enlargement of the cardiac area). Respiratory manifestations - such as tachydyspnea - can be aggravated by the occurren ce of acute lung edema. In addition, neurological findings can be expressed with great variety - depending on the toxi city of the venom and the affected sites -, with psychomotor agitation, drowsiness, mental confusion, hypertonia, tremors, miosis, mydriasis, priapism, muscle spasms, systemic pa resthesia and ataxia (Funasa, 2001; Albuquerque et al., 2018).
Due to the severe signs and symptoms, there are reports of death from the scorpion accident, the most common cau se of which is respiratory failure associated with circulatory shock, aggravated by dehydration and changes in hydroelec trolytic balance (usually related to exacerbated vomiting). In addition to the age, weight and health status of the patient - for example, the presence of pre-existing chronic diseases - medical analysis of the bite’s location and the patient’s glo bal status is extremely important (Amaral et al., 1991; 1993; Baldini et al., 2010; Elatrous et al., 1999; Geron et al., 1993; Hering et al., 1993; Karnad, 1998).
Diagnosis and laboratorial analysis
In scorpion accidents, the diagnosis must be established on clinical and epidemiological bases. The anamnesis must be detailed and the physical examination meticulous. It is im portant that the venomous animal, if possible, be captured and taken to the hospital, which may help to conduct the treatment (Brasil, 2001; Brasil, 2019).
There are tests that can be performed for the purpose of complementing the diagnosis and monitoring the clinical evolution and the appearance of complications, including biochemical tests, electrocardiogram, echocardiogram and chest radiography (Brasil, 2010; Brasil, 2019).
In moderate to severe cases, some changes in biochemical tests usually occur, with frequently high blood glucose, hy pokalemia and hyponatremia, high amylase, hemolysis and thrombocytosis, leukocytosis with a predominance of neu trophils and an increase in creatinokinase and its MB fraction. Troponin I can be harvested to see if there was damage to the heart muscle (Brazil, 2019).
Changes in the electrocardiogram commonly occur in ac cidents with T. serrulatus and can disappear within three to seven days. The most common events are ventricular ex trasystoles, sinus tachy / bradycardia, protruding U waves, atrial fibrillation and T wave inversion in several leads (Brasil, 2019). Like acute myocardial infarction, scorpionism can also show ST-sequence elevation / depression (Brasil, 2016). The echocardiogram is a method used to diagnose myocarditis in cases of scorpionism. The changes vary according to the degree of cardiac dysfunction, which depends on the severity of the case. The most commonly found echocardiographic changes are reduced ejection fraction, global left ventricular hypokinesia and mitral regurgitation (Campos et al., 2020).
A diffuse and alveolar interstitial pattern, expansion of the cardiac area and unilateral costophrenic sinus veiling, showing evidence of acute lung edema can be seen on chest radiography (Martins et al., 2018; Brazil, 2001).
Differential diagnosis
When there is no collection / identification of the stinging scorpion, it is necessary to establish a differential diagnosis as there are several clinical conditions in different diseases that present similar manifestations to scorpionism. Although there are studies that aimed to develop diagnostics by im munoassays to detect components of the venom in patient samples (Rezende et al., 1995; Chávez-Olórtegui et al., 1994; Martins et al. 2018), there is still no method available com mercially. Thus, a different diagnosis based on the signs and symptoms of different diseases is essential.
Accidents by other venomous animals are important to offer differential diagnoses. Poisoning by Lonomia obliqua differs from scorpion in that it has a burning sensation at the con tact site, in addition to promoting hemorrhagic disorders, such as hematuria, intense bruising, epistaxis, among others (Silva, 2007; Franco et al., 2020). When the suspect is a centi pede accident, it is necessary to assess the heart and respira tory rate, since, in these morbid events, these parameters are within the expected, physiologically, different from what oc curs in the scorpionic accident (Graça et al., 2008). In the case of an accident by Micrurus (true coral), the characteristic that can help differentiate an accident by scorpion is paresthe sia, and in the elapidic accident paralysis of different muscle groups can occur, which can even compromise the mecha nics ventilation (Brasil, 2001; Siqueira-Batista et al., 2020).
Araneism - that is, accidents by spiders - must be taken into account, since these animals are spontaneously found inside or around houses. Among all spider species, the most impor tant for human medicine are Phoneutria ("armadeira spider"), Latrodectus (black widow) and Loxosceles (brown spider) (Santana et al., 2020a). The wound caused by some of these spiders can be differentiated from the injuries caused by scorpions, since the Loxosceles sting has a central bubble that usually evolves into necrosis (Santana et al., 2020b, Barish & Arnold, 2018). When it comes to Phoneutria bites, local symptoms are often similar to those of scorpion accidents and are sometimes indistinguishable (Salvatierra et al., 2018; Santana et al., 2020a; Santana et al., 2020b). The crotalic accident (rattlesnake) does not present pain at the site of the bite (when present, the pain is considered mild), in addition to progressing with minor ede ma and, eventually, systemic disorders, such as sagging fa cial muscles, ophthalmoplegia, dysgeusia, dysphagia, among others (Brasil, 2001; Siqueira-Batista et al., 2020).
In botulism, for example, there are similar manifestations to those of the scorpion accident; however, one of the outstan ding characteristics of botulism is the preservation of cons cience, differing from accidents by scorpions, which tend to cause confusion (Brasil, 2006; Gomes et al., 2008). Myasthenia gravis can also be considered a differential diagnosis; howe ver, the patient becomes asthenic with routine and repetiti ve activities, in addition to reporting a worsening at the end of the day / night, and improves with stillness; in addition, another difference between these two diseases is due to the time of evolution, since myasthenia gravis progresses with a subacute / chronic evolution, different from injuries by scor pions (Branco, 2011; Bizarro et al., 2017).
Insect bites produce - eventually - similar manifestations to those described in scorpion breeding, but, except in severe allergic reactions, those pictures do not usually evolve with systemic involvement (Barish & Arnold, 2018). Dystonic reac tions, induced by medication, present as alterations involun tary muscle contractions and repetitive movements of sprain; the history of drug ingestion can help differentiation (Barrei ra & Magaldi, 2009).
Another disease that must be taken into account is tetanus. However, this condition presentes a few symptoms like mus cle hypertonia, trismus, in addition to contractures and pain in the back and limbs (Brasil, 2019). Acute pancreatitis leads to nausea, vomiting and severe abdominal pain, which are the most common symptoms of this disease; it is highlighted that scorpionism itself can provoke such a picture (Carneiro & Siqueira-Batista, 2004; Sepðlveda et al., 2019). Organo phosphate toxicity can manifest, clinically, in a similar way to injuries caused by scorpions; the distinction can be sought in terms of the possibility of exposure to such compounds (Vinhal & Soares, 2018).
Treatment
The first conduct of action to be taken after the scorpion bite is to wash the area with soap and water. Then, the vic tim must seek or be taken immediately to the health servi ce for the assessment and observation of symptoms (Brasil, 2009). Most accidents with scorpions fall under mild cases, so treatment will depend on the clinical manifestations ob served in the patient. It is worth mentioning that it is harmful and contraindicated to use a tourniquet, apply heat, squeeze, cut or place any substance on the wound site (Brasil, 2016). Medical management in mild to moderate cases involves the use of symptomatic drugs for local pain relief, the use of analgesics, such as dipyrone or meperidine, depending on the intensity of the pain, orally or parenterally, associated with local blockage by infiltration with 2% lidocaine without vasoconstrictor (Ciruffo, 2012). In moderate to severe cases, the stay in the hospital can vary from hours to days of hospi talization, requiring the administration of other medications such as metoclopramide, venous fluid therapy and correction of hydroelectrolytic, acid-base disorders and systemic arte rial hypertension (Campos et al., 2020). It is also important to maintain electrocardiographic monitoring in the first 24 hours after admission (Cupo et al., 2003; Cupo, 2017).
Isolated signs and symptoms such as sweating, nausea, tachy cardia, vomiting and tachypnea may occur in moderate cases. In severe cases, a drastic worsening of the clinical picture may occur, with emphasis on the occurrence of incoercible vomi ting, dehydration, intense sweating, drooling, periods of pros tration - alternating with agitation -, shock, heart failure, acute lung edema and coma (Cupo et al., 2003; Ciruffo et al., 2012; Carmo et al., 2019). The administration of anti-scorpion serum (SAE), intravenously, is reserved for such contexts. It’s possible to acquire more information and to obtain the anti-scorpion serum by phone and emailing to Butantan, the information are available below: Customer Service (SAC): +55 0800 701 2850 e-mail: sac@butantan.gov.br (Table 1).
Table 1 Number of ampoules of antiscorpionic or antiaracnidic serum (Loxosceles, Phoneutria, Tityus) specific according to the severity of the accident.
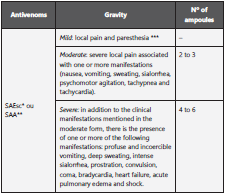
*SAEsc: antiscorpionic serum;
**SAA: antiaracnidic serum (Loxosceles, Phoneutria, Tityus);
***Observation time of children bitten: 6 to 12 hours.
Source: adapted from Health Surveillance Guide, 2019.
The serum that is supplied to the municipalities is only avai lable in hospitals linked to the Unified Health System - in portuguese Sistema Único de Saúde (SUS) (Brasil, 2019). In health facilities where the SAE is missing, antiaracnidic serum (ARS) may be used.
Ecology and epidemiology of scorpionism
Scorpion species are present in almost all terrestrial ecosys tems, with the exception of tundra, high latitude taiga, boreal areas and in some high altitude areas (Polis, 1990; Brazil & Porto, 2010). Most species have specific habitat conditions and presumed and localized in ecological and biogeographic patterns (Lourenço & Eickstedt, 2009).
These animals generally have nocturnal habits. They can be found in rocks’ openings, trees’ barks, decaying trunks, un der rocks and leaves, and inside burrows and caves, protec ting themselves from their natural predators (Soto-Blanco & Melo, 2018). In these places, temperature, humidity and the number of prey are decisive requirements for the installation and increase in the number of scorpions. In tropical regions, they are more frequent in periods with higher temperatures, especially when it rains. Scorpions are sitting-predators, and to catch prey, use sensory structures. If the prey is reluctant, the scorpion uses the venom to immobilize it and begins the digestion process. Despite pricking the prey, in some cases, scorpions do not inoculate the venom. In urban areas, the se venomous animals can be good predators of arthropods, which are sometimes harmful to humans, such as insects and spiders (Brasil, 2009).
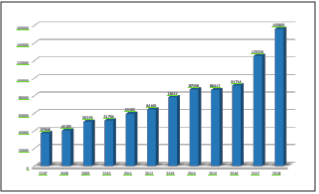
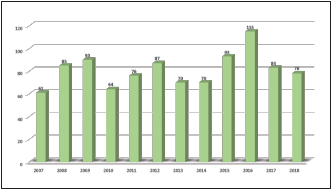
In Brazil, between 2007 and 2018, 1,899,795 accidents by venomous animals were reported in the Notifiable Disea ses Information System (SINAN), of which 2,972 evolved to death (Figure 3A). Among accidents with venomous animals, the scorpion accident presented the greatest increase in the number of cases, from 37,368 notifications in 2007 to 155,859 in 2018, (Brasil, 2019) demonstrating that it was the accident with venomous animals with the highest incidence: 75.2 per 100,000 inhabitants. In this period, from 2007 to 2018, there were 927,750 cases and 972 deaths (Figure 3B).
The most occurrences of accidents with scorpions occurs among males, aged from 20 to 39 years. Women and children may present a more severe clinical condition, as they usua lly have lower body weight. In Brazil, most events are light; however, the severity of accidents depends on some factors, such as: species and quantity of inoculated venom and age of the victim (Brasil, 2016).
Prophylaxis and control
Prophylaxis and the control of scorpionism - in the world and in Brazil - are extremely important to avoid serious disloca tions. For this reason, the dissemination of information - in cluding the scorpion’s ways of life - is extremely useful for the population to act in the control of accidents. It is always ne cessary to pay attention to clothes, shoes, bath / face towels and carpets by shaking them before use. Keep beds and cribs distanced from walls and floor, avoid accumulating debris and leave gardens without maintenance (Teixeira et al., 2017). When practicing services for handling construction materials, wood, gardens and others, it is always necessary to use Per sonal Protective Equipment (PPE) such as gloves and boots. Surveillance for control needs continuity and commitment, since scorpions are able to survive in adverse conditions for prolonged periods including climatic variations, even insecti cides harmful to it (Brasil, 2016). It is of great importance that these prophylaxis and control measures are applied both in rural and urban areas (Brasil, 2016; Brasil, 2009).
Final considerations
Accidents involving scorpions should deserve attention from health professionals, considering the variety of existing species - with significant capacity to adapt to the environment -, the annual number of occurrences and the pathophysiological ac tions of venom relationed to Homo sapiens. This article addresses scorpion accidents, common events in Brazil, focusing on clinic, diagnosis and treatment, with a main focus on presenting up-to-date information on the conduct of these morbid conditions.
In addition, it should be noted that the subject is often little dis cussed in health courses, reflecting on an often unsafe service by health professionals. The information covered in this study will allow a broad understanding of scorpionism, in its various aspects epidemiological, physiological, diagnostic and thera peutic promoting the discussion on the topic and enabling the establishment of a safe and scientifically based service.