Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Salud Pública
Print version ISSN 0124-0064
Rev. salud pública vol.11 no.3 Bogotá May/June 2009
Instituto Nacional de Enfermedades Respiratorias "Emilio Coni". labconi@yahoo.com.ar, suimaz@yahoo.com.
ABSTRACT
Objectives Determining private doctors' (PD) knowledge and practice regarding tuberculosis (TB) control issues and exploring the availability of TB drugs in private pharmacies (PP) in a low incidence setting in Argentina (Santa Fe).
Methods A questionnaire was applied to random sample of 87 PPs and 61 PDs, proportionally assigned according to the local distribution of specialists and general practitioners. Their knowledge and practice were explored regarding the symptoms, diagnosis and case management of pulmonary TB, as defined and specified by Argentinean TB management guidelines.
Results Although most PDs were aware of the main symptoms presented by TB, they were unlikely to ask for a microscope examination for a person suffering persistent cough. More than 30 % of PDs considered X-ray before "microscope examination of stained sputa" for TB diagnosis. PDs had significantly lower levels of knowledge regarding the symptoms and diagnostic procedures for TB compared to those who combined public and private work. Most PDs (91,3 %) referred their TB patients to a public facility for treatment. Accordingly, very few TB drug prescriptions were managed in PPs.
Discussion Addressing mismanagement of TB patients in the private sector does not appear to be a problem in Santa Fe in terms of treatment (although being considered crucial for effective TB control) because most PDs are aware of the TB programme which appears to be comprehensive and accessible. The private sector's main aim should be to improve its skills regarding TB diagnosis.
Key Words: Tuberculosis, health knowledge, attitude, practice, private sector, Argentina (source: MeSH, NLM)
RESUMEN
Objetivos Determinar prácticas y conocimientos de los médicos privados (MP) acerca del control de la tuberculosis (TB) y explorar la disponibilidad de drogas anti-TB en farmacias privadas (FP) en un entorno de baja incidencia de TB de Argentina.
Métodos Se realizó una encuesta por cuestionario sobre una muestra aleatoria de 87 FP y 61 MP, asignados proporcionalmente según la distribución local de médicos especialistas y generalistas. Se investigaron conocimientos y prácticas en relación a síntomas, diagnóstico y manejo de casos de TB, según lo especifican las normas.
Resultados Aunque la mayoría de los médicos conocían los principales síntomas, era poco probable que solicitaran exámenes microscópicos de esputo (EME) en pacientes con tos persistente. Más del 30 % de los MP priorizaron la radiografía de tórax por encima del EME para el diagnóstico de TB. Los médicos que sólo trabajaban en el sector privado tuvieron niveles significativamente más bajos de conocimientos que los que trabajaban tanto en el sector público como privado. La mayoría de los MP (91,3 %) referían sus pacientes para tratamiento a un servicio público. Concordantemente, el número de recetas de medicamentos anti-TB manejados por las FP era muy pequeño.
Discusión Si bien se considera que, la búsqueda de una solución para el manejo inadecuado de casos en el sector privado es crucial para un control efectivo de la TB, en Santa Fe, éste no parece ser un problema importante, ya que la mayoría de los MP conocen el Programa de Control, que aparece como accesible. El principal objetivo del sector privado debería ser mejorar sus habilidades para el diagnóstico.
Palabras Clave: Tuberculosis, conocimientos, actitudes y práctica en salud, sector privado, Argentina (fuente: DeCS, BIREME)
The success of the DOTS (Direct Observed Treatment – short course) strategy (1) depends on a particular health-care system's ability to identify and follow-up tuberculosis (TB) suspects. Health systems' inability to diag-nose and treat TB has been shown in many studies (2-6).
Argentina is considered to be a country having a medium level TB notification rate. The National TB Programme (NTP) promotes free TB diagnosis and supervised treatment. In addition to the NTP, each of the country's 24 jurisdictions has its own Provincial TB Programme which is responsible for implementing health policies, these being mainly delivered through a structured network of government units. Health-care is also delivered by social health insurance which is mandatory for the salaried labor force and the private sector. Social insurance health-care is mainly delivered by private providers which are contracted to attend the insured population. Methods commonly used for documenting the private sector's role in TB control consist of semi-structured interviews of private doctors (PDs) and drug-retailers. Most of these studies have been performed in high TB prevalence countries (7-10). Zerbini (11) has shown that in Argentina patients first consulting a private doctor had longer delays in TB diagnosis than those who attended a public setting. Private-public mix (PPM) is a strategy which is strongly recommended by the WHO to reinforce TB control. TB programme-private sector interaction studies will help create an evidence base for achieving an effective PPM and in devising more effective strategies and guidelines. To the best of our knowledge, apart from Bolivia, private sector knowledge and practice in the region has not been documented to date.
Our objective was to determine PD knowledge and practices in Santa Fe city, Argentina, regarding the symptoms, diagnosis and case management of pulmonary TB (pTB). The availability of TB drugs in private pharmacies (PPs) was also explored.
Setting
Santa Fe city, having a TB incidence rate of about 14/100 000 population in 2006 (12), is the capital of Santa Fe province, the third largest jurisdiction in Argentina, taking the number of inhabitants into account. In Santa Fe province, 62 % of the hospitals are in private hands (12); percentage health expenditure from private sources has been around 50 % (14). Contrary to the public sector, private services are heterogeneous. Although non-specific measures have been designed within the NTP to target TB cases already identified by the private sector, there is no formal participation of PDs in TB control.
Survey of PDs
A cross-sectional study was conducted in 2007 on PDs working in Santa Fe city. The PDs were randomly selected from three strata of physicians: GPs, infectious disease specialists and pulmonologists, registered by the medical societies. Sample size was calculated by using 50 % as an estimated frequency for the variables which would be analysed, since this percentage allows the largest possible sample size to be calculated for a determined level of confidence (15). The least reliable sample size was 71, considering that the number of doctors registered in the three medical societies was 134, using 95 % confidence interval (CI), 10 % error and 25 % non-responding rate. The sample size resulted in 58 GPs, 3 infectious disease specialists and 10 pulmonologists, taking into account the doctors' proportional distribution according to specialty. PDs working for the TB programme, doctors who had no private work and those who had participated in the pre-test were all excluded. Information from 61 PDs was analysed (48 GPs, 3 infectious disease specialists and 10 pulmonologists).
An appointment was made with each doctor. Verbal informed consent was obtained and anonymity was assured. The following were investigated: whether they had ever seen TB suspects in their practice, how they diagnosed pTB, whether they referred the patients or treated them themselves and how they possibly treated pTB. Answers to questions about pTB symptom knowledge were regarded as being correct if 3 of the 9 major TB symptoms mentioned in NTP guidelines were identified. Knowledge of diagnostic procedures was regarded as being correct if microscopy was ranked higher than X-ray and other laboratory tests. The smear-positive pTB regime was regarded as being correct if it followed NTP guidelines. Subjects were also asked about supervising drug taking, tracing patients who missed appointments and contact tracing. Data regarding doctors' age, qualification, time spent in practice and whether they additionally worked in a public facility was also collected.
Survey of PPs
A random sample of 99 of the 600 officially registered pharmacies in Santa Fe city was taken; 50 % was considered as an estimated frequency for the variables which would be analysed when calculating sample size (using 95 % CI, 10 % error and 20 % non-responding rate). Contacts were made with the local branch of the Pharmacists' College before beginning the study to discuss the investigation's objectives. The questionnaire which was sent to the PPs by post had sections concerning general information (age, tine spent in practice), availability of drugs, number and type of prescriptions received during the last 12 months, sales of rifampicin (R) for uses other than TB and advice given by vendors when receiving an anti-TB drug prescription. 87 responses were obtained from the 99 questionnaires sent out.
Statistical analysis
Epi Info (version 6.04) was used for statistical analysis. The Kruskal-Wallis test was used for comparing groups of continuous variables. Potential factors for suboptimal knowledge of symptoms, diagnosis and treatment were analysed and OR indicated (95 %CI); data regarding PDs' age was stratified as <40, 40-49 and ³50, whereas experience was analysed as £10, 11-19 and ³19. Logistical regression was used for controlling the effect of modification and confounding.
PPs
Of the 87 pharmacies that participated, 65 (74,7 %) had at least one anti-TB drug in stock and 50 (77 %) of them only had R; all the remaining pharmacies had isoniazid (H) but only two carried ethambutol (E) and pyrazinamide (Z). However, 83 of the PPs indicated that they could get all the drugs from the wholesalers in a very short time.
Five of the PPs (5,7 %) reported having received at least one prescription containing H, E or Z during the last year; overall, 6 prescriptions had been received by the 87 PPs, 0.1 on average per year.
Only 15 PPs (17,2 %) were aware of the NTP; 12 of those who replied in the affirmative expressed their knowledge concerning NTP norms. Nevertheless, when the pharmacists were asked about their attitude when receiving an anti-TB prescription, none of them referred patients to a public service. NTP awareness or of the norms was not associated with the pharmacists' ages or their duration in practice (Kruskal Wallis, p>0,05).
Fifty-six PPs (64,4 %) said that they remembered having received prescriptions containing only R during the last year. When they were asked, about the most frequent diagnosis indicated in the prescriptions, 21 PPs answered that they did not remember; the remaining 35 said that the most common indications were respiratory diseases (12 PPs), treating methicillin-resistant Staphylococcus aureus infections (12 PPs), prophylactic therapy against Neisseria meningitidis (8 PPs) and brucellosis (3 PPs).
PDs
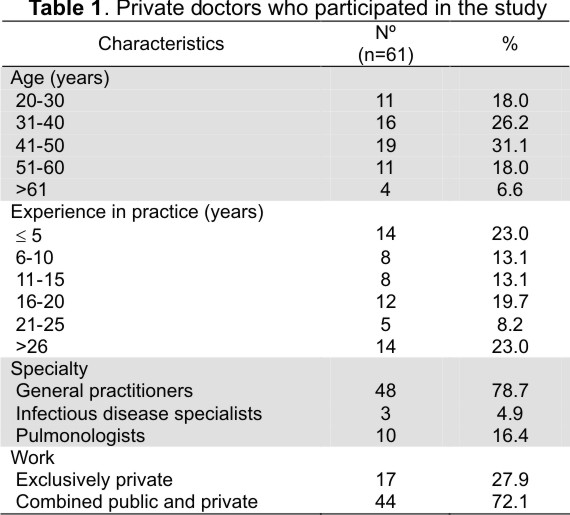
Table 1 gives the background characteristics for the 61 doctors who were interviewed. The answers given to the questions are described below.
Investigation advice for pTB suspected (TBS) patients
Fifty (82,0 %) of the 61 PDs referred to a combination of at least 3 of the 9 main symptoms mentioned in the NTP guidelines. The majority of PDs were aware that cough was the main symptom of TB but fewer (30 % or less) knew that blood in sputum, night sweats, asthenia, dyspnoea and chest pain could also be associated with TB (Table 2).
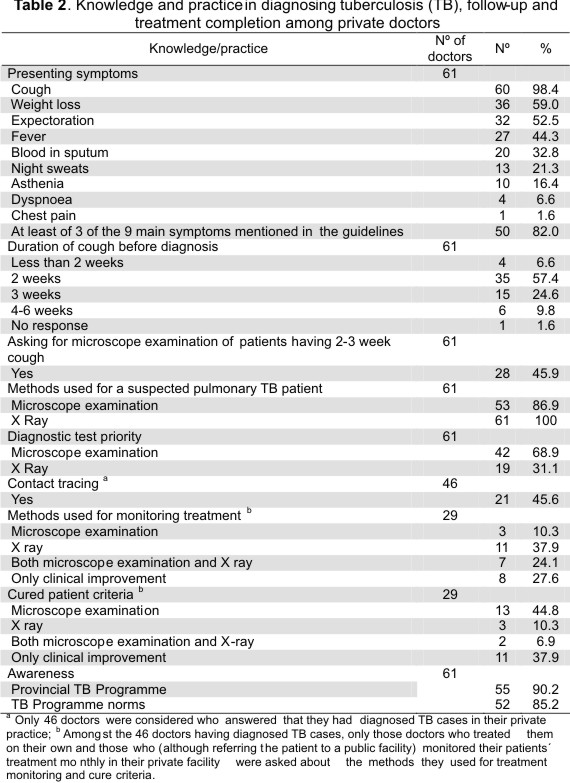
Although the vast majority of PDs (88.6 %) considered that TB should be suspected if cough lasts 2-4 weeks, most of them (54.9 %) said that they did not systematically evaluate people having persistent cough by microscope examination of sputa in their practice. Furthermore, when we asked them to rank the different diagnostic tests for TB, only 42 doctors (68.9 %) put the " microscope examination of sputa" before any other test.
Treatment regime used by PDs for smear-positive pTB patients
Seven (11,5 %) of the 61 PDs who had never treated patients on their own did not specify the regime used; the remaining 54 indicated 16 combinations of two or more of the five first-line drugs, namely streptomycin (S), H, R, E and Z prescribed for different periods of time. Only 24 (44,4 %) PDs indicated the NTP-recommended chemotherapy regime and duration. Although drugs were prescribed by another 12 PDs for the correct period of time, the regime was not in accordance with the guidelines. Another 11 (20,4 %) prescribed drugs for longer periods than necessary, whereas 7 (13,0 %) indicated drugs for shorter periods than required. Direct observation of medicine taking was mentioned by only 36 PDs (66,7 %).
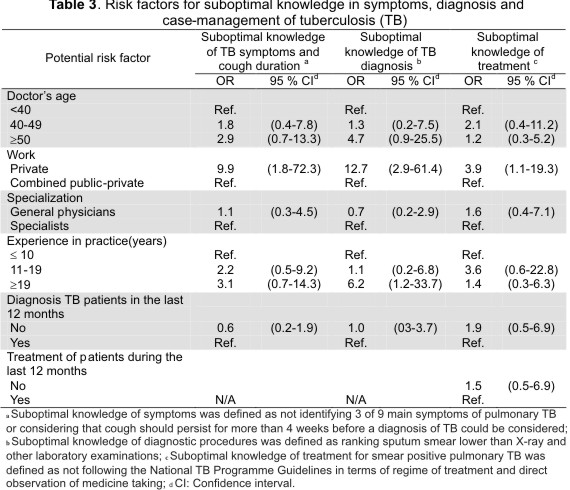
Factors for suboptimal knowledge of symptoms, diagnosis and treatment Suboptimal knowledge of pTB symptoms and treatment was more common amongst doctors working exclusively in the private sector (9.9 OR: 1.8-72.3 95 % CI for symptoms and 3.9 OR: 1.1-19.3 95 %CI for treatment) than for those working in both public and private sectors. Time spent in practice and sector of work were independently associated with suboptimal knowledge of diagnosis in simple analysis. However, after allowing for confounders, sector of work was the only variable associating knowledge of diagnosis with a more common suboptimal knowledge amongst those PDs working in the private sector than amongst those working in both public and private facilities (Table 3).
Treatment/referral of tuberculosis patients
Only 4 (8,7 %) of the 46 PDs who said that they had ever diagnosed TB patients preferred to treat patients on their own, whereas 42 referred their patients to a public facility; 25 (59,5 %) of these 42 PDs, besides referring the patients, preferred to attend them monthly in their private facilities for monitoring treatment progress.
Treatment monitoring, outcome and patient compliance in private practice
Questions about methods used for treatment monitoring and completion were only asked of those PDs who treated on their own (4 PDs) and those who, although referring patients to a public facility, monitored their patients' treatment in their private facilities (25 PDs). Out of these 29 doctors, only 10 (34,5 %) and 15 (51,7 %) PDs would advise in sputum, with/without other tests, for treatment monitoring and as criterion for stopping treatment, respectively (Table 2).
Regarding patient compliance, only 8 (27,6 %) PDs reported that all of their TB patients had completed treatment. Four (13,8 %) PDs admitted that some of their patients had not completed treatment, whereas the rest (17 PDs, 58,6 %) answered that they were not sure about treatment completion. When they were asked about the mechanisms for tracing defaulters, 14 said that they telephoned patients or the TB programme and the other 15 said that they did not have any mechanism for tracing the defaulters.
When PDs were asked for their perceptions of the most common cause of patient's treatment default, 23 PDs considered that, "patients did not realize the importance of regular treatment," 13 that "patients got better very soon and did not feel the need to continue so long a treatment," 11 said that digestive problems
were the main cause, 11 put the responsibility on other social reasons (poverty, ignorance, being illiterate), whereas only three mentioned "poor service quality" as being the main cause.
The percentage of PPs selling TB drugs is a less-than-perfect proxy for the quantity of drugs sold because a small number of PPs could still account for relatively large quantities of the drugs sold in the market. Only 6 % of the PPs in our study had been receiving anti-TB prescriptions during the last 12 months. However, compared to studies in Asia (10) or Bolivia (16), in which such percentages rose to 60 % and 25 %, respectively, this still suggests a much smaller TB drug market. Quantifying the number of TB drug prescriptions during a period of time, through interviews with pharmacists, is prone to recall bias if no records are kept, as is usually the case. An average 0.1 prescriptions/year was estimated in our sample of 87 PPs, a small figure to remember precisely out of all prescriptions filled during a year. However, comparison with studies in Vietnam and India (in which the figures rose to 1.3 (10) and 9.3 (8) prescriptions/month on average) indicates the little importance of the TB drug market. On the other hand, because R is prescribed for uses other than anti-TB treatment, the availability of H, E or Z might reflect the quantity of TB treatments taken outside the programme. Only 2 out of 87 PPs (2 %) had a full course of treatment in stock. Nevertheless, 95 % of PPs indicated that they could get all TB-drugs from the wholesalers in a short time, thus demonstrating that even if the TB-drug market is not currently of importance, the ease of gaining access to them constitutes a threat for the NTP. Furthermore, R should be reserved for TB to limit the risk of developing resistance. In Saudi Arabia, where R is widely prescribed for non-TB uses, R resistance has been rising and contrasts with the low resistance to E and H which cannot, by law, be dispensed in PPs (17). The fact that no other TB drug was available in most PPs in our sample suggests that R is being mainly sold for non-TB use, thereby constituting a problem which needs to be tackled with prescribers.
Our results showed that although most PDs were aware of the main TB symptoms, they were unlikely to ask for a sputum examination for a person having persistent cough. A possible explanation for such low suspicion could be that TB is hardly encountered in private practice as Santa Fe is already a low-medium incidence region which would mean that PDs consider other, more common, respiratory conditions, instead of TB. The percentage of TB cases detected in a population amongst TBS depends on both TB prevalence and case-finding activity intensity. People attending public centres in Argentina, which are free of charge, tend to be poorer than those attended in private facilities. It is thus expected that TB would be more frequent among those attending the public facilities than among people who consult the private sector; consequently, if case-finding intensity was similar, the percentage of TB cases detected among TBS would be higher in public facilities than in private ones. Nevertheless, it was found that the figures from private and public facilities were similar when using our public laboratory's data register (to which all public and most bigger private laboratories in Santa Fe refer samples) to calculate the number of TBS which were evaluated to find a TB case during the last two years, which would be in accordance with our previous suggestion about poor suspicion amongst PDs. Furthermore, in accordance with other studies (18-20), we have found that exclusively PDs have significantly lower levels of knowledge of symptoms and diagnosis compared to those who combined public and private work. One possible explanation for this difference is that public doctors would attend TB training courses (conducted by the TB programme) more frequently than doctors only working in the private sector. A recent controlled trial showed that educational interventions aimed at promoting TB screening were effective in increasing TB detection (21). Furthermore, less than 50 % of PDs who had diagnosed TB reported having studied their contacts, thereby complicating the identification of recently infected cases, or even the source of infection.
More than 30 % of PDs considered X-ray before "microscope examination of sputa" for TB diagnosis. Although 86.9 % of PDs declared that they also used microscope examination for a suspected pTB patient besides asking for X-ray; such overconfidence in X-ray may have bad implications for the NTP. Other studies (22-24) have also found that PDs did not consider microscopy crucial. Reliance on radiography for TB will result in both over-diagnosis and missed diagnoses of TB and other diseases (25).
In accordance with other studies (7,22,23,26,27), private sector treatment regimes were rarely in line with NTP standards. About a quarter of the PDs indicated regimes using more drugs or for longer periods than necessary, which can lead to increasing side-effects and adversely affects patient compliance. Furthermore, most PDs stated that they did not know whether their patients had completed treatment, putting the blame for default almost entirely on the patients themselves.
Our results also showed that sputum examination is being grossly under-used for treatment monitoring and completion. This is in complete contrast to NTP guidelines.
Radiographic assessment, although commonly used, has been shown to be unreliable for evaluating treatment (28).
Fortunately, the study also revealed that almost all PDs (91.3 %) who had ever diagnosed TB, referred patients to a public facility for treatment. This was in accordance with that found in the PP survey where very few TB prescriptions were managed. Hence, addressing TB patient mismanagement in the private sector in terms of treatment does not appear to be a problem in Santa Fe although it is considered crucial for effective TB control in any setting, especially because most PDs are aware of the TB programme, showing high confidence in public facilities for TB management.
Direct questioning about practice, as a substitute for other practice measurement methods, may have led to overestimating practice correctness. Moreover, it is likely that the non-respondents in our study had less correct knowledge and practice. There was not enough background information on the non-participants to indicate bias. Both of the above-mentioned biases would tend to show better conformity with the guidelines than reality. However, this would not change the study findings which indicated that PDs' reported compliance with the NTP is generally low.
Reinforcing knowledge is the traditional solution and is indeed one of the basic requirements which should be addressed. More cooperation is thus advisable between the NTP and postgraduate TB training course deliverers. Our findings have thus suggested that the private health sector's main aim in Santa Fe should be to improve skills regarding TB diagnosis, where the TB control programme is already comprehensive and accessible; this would reduce diagnosis and treatment delays (11) §
Acknowledgements. The authors are grateful to the College of Pharmacists and the General Practitioners, Infectious Diseases and Pulmonologists Societies of Santa Fe.
1. WHO. What is DOTS? A guide to understanding de WHO-recommended TB control strategy known as DOTS. Geneva: WHO; 1999 (Document WHO/CDS//CPC/TB/99.270). [ Links ]
2. Pehme L, Rahu K, Rahu M, Altraja A. Factors related to health system delays in the diagnosis of pulmonary tuberculosis in Estonia. Int J Tuberc Lung Dis 2007;11:275-281. [ Links ]
3. Mirsaeidi SM, Tabarsi P, Mohajer K, Falah-Tafti S, Jammati HR, Farnia P, et al. A long delay from the first symptom to definite diagnosis of pulmonary tuberculosis. Arch Iran Med 2007;10:190-193. [ Links ]
4. Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. Int J Tuberc Lung Dis 2002;6:789-795. [ Links ]
5. Rao VK, Iademarco EP, Fraser VJ, Kollef MH. Delays in the suspicion and treatment of tuberculosis among hospitalized patients. Ann Intern Med 1999;130:404-411. [ Links ]
6. Golub JE, Bur S, Cronin WA, Gange S, Baruch N, Comstock GW, Chaisson RE. Patient and health-care system delays in pulmonary tuberculosis diagnosis in a low-incidence state. Int J Tuberc Lung Dis 2005;9:992-998. [ Links ]
7. Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis 1998; 2:324-329. [ Links ]
8. Rajeswari R, Balasubramanian R, Bose MS, Sekar L, Rahman F. Private pharmacies in tuberculosis control - a neglected link. Int J Tuberc Lung Dis 2002; 6:171-173. [ Links ]
9. D´Hashim R, Hassany F, Hussain N, Iqbal Z, Irfanullah A, Islam N, et al. Front-line management of pulmonary tuberculosis: an analysis of tuberculosis and treatment practices in urban Sindh, Pakistan. Tuber Lung Dis 1996; 77:86-92. [ Links ]
10. Lönnroth K, Lambregts K, Nhien DT, Quy HT, Diwan VK. Private pharmacies and tuberculosis control: a survey of case detection skills and reported anti-tuberculosis drug dispensing in private pharmacies in Ho Chi Minh City, Vietnam. Int J Tuberc Lung Dis 2000;4:1052-1059. [ Links ]
11. Zerbini E, Chirico MC, Salvadores B, Amigot B, Estrada S, Algorry G. Delay in tuberculosis diagnosis and treatment in four provinces of Argentina. Int J Tuberc Lung Dis 2008;12:63-68. [ Links ]
12. INER "Emilio Coni". Ministerio de salud de la República Argentina. Notificación de casos de tuberculosis en la República Argentina. Santa Fe; 2007 (Document PRO.TB.Doc.Tec.07/07). [ Links ]
13. Ministerio de Salud de la Nación Argentina. Indicadores Básicos 2006.Buenos Aires:OPS; 2007. [ Links ]
14. Ventura G, Montiel L, Falbo R, Tobar F. El gasto en salud en Argentina y su método. Buenos Aires: Instituto Universitario; 2000. [ Links ]
15. Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies. A Practical Manual. Geneva: World Health Organization; 1991. [ Links ]
16. Lambert ML, Delgado R, Michaux G, Volz A, Van der Stuyft P. Tuberculosis control and the private health sector in Bolivia: a survey of pharmacies. Int J Tuberc Lung Dis 2004;8:1325-1329. [ Links ]
17. Al-Hajjaj MS, Al-Kassimi FA, Al-Mobeireek AF, Alzeer AH. Progressive rise of Mycobacterium tuberculosis resistance to rifampicin and streptomycin in Riyadh, Saudi Arabia. Respirology 2001;6:317-322. [ Links ]
18. Singla N, Sharma PP, Singla R, Jain RC. Survey of knowledge, attitudes and practices for tuberculosis among general practitioners in Delhi, India. Int J Tuberc Lung Dis 1998;2:384-389. [ Links ]
19. Shah SK, Sadiq H, Khalil M, Noor A, Rasheed G, Shah SM, et al. Do private doctors follow national guidelines for managing pulmonary tuberculosis in Pakistan? East Mediterr Health J 2003;9:776-788. [ Links ]
20. LoBue PA, Moser K, Catanzaro A. Management of tuberculosis in San Diego County: a survey of physicians' knowledge, attitudes and practices. Int J Tuberc Lung Dis 2001;5:933-938. [ Links ]
21. Peabody JW, Liu A. A cross-national comparison of the quality of clinical care using vignettes. Health Policy Plan 2007;22:294-302. [ Links ]
22. Portero JL, Rubio M. Private practitioners and tuberculosis control in the Philippines: strangers when they meet? Trop Med Int Health 2003;8:329-335. [ Links ]
23. Chakaya JM, Meme H, Kwamanga D, Githui WA, Onyango-Ouma WO, Gicheha C, et al. Planning for PPM-DOTS implementation in urban slums in Kenya: knowledge, attitude and practices of private health-care providers in Kibera slum, Nairobi. Int J Tuberc Lung Dis 2005;9:403-408. [ Links ]
24. Mahendradhata Y, Utarini A, Lazuardi U, Boelaert M, Stuyft PV. Private practitioners and tuberculosis case detection in Jogjakarta, Indonesia: actual role and potential. Trop Med Int Health. 2007;12:1218-1224. [ Links ]
25. Koppaca R, Bock N. How reliable is chest radiography. In: Toman's tuberculosis. Case detection, treatment and monitoring. 2nd edition. Geneva:WHO; 2004. [ Links ]
26. Nshuti L, Neuhauser D, Johnson JL, Adatu F, Whalen CC. Public and private providers' quality of care for tuberculosis patients in Kampala, Uganda. Int J Tuberc Lung Dis 2001;5:1006-1012. [ Links ]
27. Ollé-Goig JE, Cullity JE, Vargas R. A survey of prescribing patterns for tuberculosis treatment amongst doctors in a Bolivian city. Int J Tuberc Lung Dis 1999;3:74-78. [ Links ]
28. Santha T. How can the progress of treatment be monitored. In: Toman's tuberculosis. Case detection, treatment and monitoring. 2nd edition. Geneva: WHO; 2004. [ Links ]














