Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Salud Pública
versión impresa ISSN 0124-0064
Rev. salud pública v.12 n.2 Bogotá mar./abr. 2010
John J. Arteaga-Guerra, Virginia Cerón-Souza and Ana C. Mafla
Dentistry School, Universidad Cooperativa de Colombia, Pasto, Colombia. john.arteaga@correoucc.edu.co, virginia.ceron@correoucc.edu.co, ana.maffla@correoucc.edu.co
Received 13th August 2009/Send for Modification 1th April 2010/Accepted 20th April
ABSTRACT
Objective The aim of this study was to determine the dynamic between periodontitis and stress and the incidence of preterm birth (PTB), low birth weight (LBW) and preterm low birth weight (PLBW) in pregnant women from Pasto, Nariño, Colombia.
Methods Forty-six women who attended to "Hospital Local Civil" localized in the city were involved. Periodontal clinical evaluation, pregnancy outcome variables and a stress scale were collected. Data were analyzed using descriptive and analytic statistics.
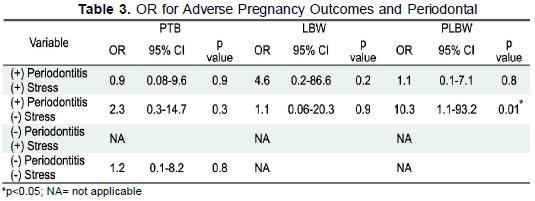
Results The incidence of PTB was 13 %, of LBW was 4.3 %, and the occurrence of PLBW was 21.7 %. Our findings showed that the presence of periodontitis and stress all together increase the risk of LBW babies (OR=4.6; 95 % CI: 0.2-86.6). Regarding, periodontitis and stress interaction, the risk of PTB (OR=0.9; 95 % CI: 0.08-9.6) and PLBW (OR=1.1; 95 % CI: 0.1-7.1) decreased in the presence of these two variables, although their values were higher in the absent of stress (PTB, OR=2.3; 95 % CI: 0.3- 14.7 and PLBW, OR=10.3; 95 % CI:1.1-93.2).
Conclusions The periodontal disease in this study was associated with PTB, LBW and PLBW. However, their risk depends on the physiological changes produced by stress.
Key Words: Pregnancy, periodontal diseases, psychological stress, physiological stress, preterm birth, infant low birth weight (source: MeSH, NLM).
RESUMEN
Objetivo El objetivo de este estudio fue determinar la dinámica entre periodontitis, estrés y la incidencia de nacimientos prematuros (NP), de bajo peso al nacer (BPN) y de prematuros y bajo peso al nacer (NPBP) de mujeres embarazadas de Pasto, Nariño, Colombia.
Materiales y Métodos Un total de 46 mujeres que asistían al Hospital Local Civil de la ciudad fueron incluidas. Una evaluación clínica periodontal, variables sobre el parto y una escala de estrés fueron registradas. Los datos fueron analizados usando estadística descriptiva y analítica.
Resultados La incidencia de NP fue 13 %, de BPN de 4,3 %, y la ocurrencia de NPBP de 21,7 %. Nuestros hallazgos muestran que la presencia de periodontitis y estrés en conjunto incrementan el riesgo de BPN (OR=4,6; IC al 95 % : 0,2-86,6). De acuerdo, con la interacción entre periodontitis y estrés, el riesgo de NP (OR=0,9; IC al 95 % :0,08- 9,6) y NPBP (OR=1,1; IC al 95 %: 0,1-7,1) disminuyó en la presencia de las dos variables, aunque sus riesgos fueron más elevados en la ausencia de estrés (NP, OR=2,3; IC al 95 %: 0,3-14,7 y NPBP, OR=10,3; IC al 95 % :1,1-93,2).
Conclusión La enfermedad periodontal en este estudio estuvo asociada con NP, BPN y NPBP. Sin embargo, su riesgo depende de los cambios fisiológicos producidos por el estrés.
Palabras Clave: Embarazo, enfermedades periodontales, estrés psicológico, estrés fisiológico, nacimiento prematuro, recién nacido de bajo peso (fuente: DeCS, BIREME).
The target of reducing infant mortality by at least two-third before 2015 is one of the major international agreed-upon goals. It is important to emphasize that infant breastfeeding and infant mortality are complex development indicators. In this sense, developed countries such as United States monitor the low birthweight infants as a priority, since it is one of infant mortality causes (1). Low birthweight thus defines a heterogeneous group of infants: some are born early, some are born growth restricted, and others are born both early and growth restricted. It is generally accepted that being born with low birthweight is a disadvantage for the baby. In addition, short gestation (preterm birth) is the main cause of death, morbidity and disability (2). In Colombia, in 2008 the <5 year-old infant mortality rate was 18.7 per 1 000 live births (3). According to mortality causes, in 2000, the World Health Organization (WHO) reports that 62.1% of deaths in these infants are due to neonatal causes in our country (4). A study published in 2001 in Cali, Colombia shows 19.5 % infants had low birthweight, and 70 % among them were associated with perinatal death (5).
Currently, dentistry is involved with this public health problem, since in the last years there is a setting association between systemic diseases and oral health problems, especially with periodontal disease (6,7). Different studies in the field of periodontal medicine have focused on an association between maternal periodontitis and adverse pregnancy outcomes, such as pre-eclampsia (8), preterm birth and low birth weight (9,10). On the other hand, risk factor such as stress is also associated with preterm birth, low birthweight (11) and preterm birth low birthweight infants. Stress is defined as the perception of discrepancy between environmental demands (stressors) and individual capacities to fulfill these demands (12). In addition, one of the hormones produced mainly in response to physical or psychological stress is cortisol. In this sense, a study by Cury et al. (13), in 2007 found that increased levels of cortisol can lead to more destruction of the gums and bone due to periodontal diseases which may increase the risk of preterm birth (PTB), low birthweight (LBW) and preterm lowbirthweight (PLBW) babies.
Few studies have examined the relationship among maternal periodontal disease, stress, PTB, LBW, and PLBW. For this reason the aim of this study was to investigate the dynamic of these three variables as markers for future adverse pregnancy outcomes in pregnant women from Pasto, Nariño, Colombia through a case-control study. It has designed to determine if an exposure or several exposures are associated with an outcome. In this research, we identify the cases, a group known to have the outcome, and the controls a group known to be free of the outcome. Then, look back in time to learn which subjects in each group had the exposure (s), comparing the risk of the exposure in the case group to the control group.
The study was carried out between June 2008 and April 2009. During this ten months study, there were 112 deliveries at the Delivery Room at the "Hospital Local Civil" in Pasto, Nariño, Colombia. Eligible participants were selected within 48 hours of delivery in the postpartum period according to the accessibility and availability of women. The study population consisted of 46 sequential systemic healthy women between 18 and 34 years of age, which had had a vaginal partum. The exclusion criteria were: mothers who did not sign the written informed consent, smoked, consumed alcoholic drinks in a great amount, took drugs, had an age >35 years, or other medical diseases, and pregnant woman who did not prenatal medical care visits. According to periodontal disease, mothers who had combined periodontal endodontic lesions. Regarding stress, woman with no education, primary school or less than junior high school education were not included. The study was approved by Ethics Committee of Universidad Cooperativa de Colombia-Pasto (Act No. CE004-07). A questionnaire was used to record demographic data, current obstetric histories, and information concerning to the delivery
Oral Hygiene, Gingival Bleeding and Periodontal examination. For scoring buccal and lingual dental plaque, Quigley-Hein index modified by Turesky (QHI) (14) was taken. To score gingival bleeding for buccal and lingual surfaces, a Sulcus Bleeding Index (SBI) (15) and Bleeding on Probing (BOP) were assessed. (16). Periodontal examination was done by two dental clinicians. A William-Fox Hu-Friedy® periodontal probe was used. The data was collected on a periodontal chart. It included clinical attachment, and probing depth at 6 sites per tooth, i.e., mesiobuccal, midbuccal, distobuccal, mesiolingual, midlingual, and distolingual. A pregnant woman was regarded as having periodontitis if she had at least four teeth with PD >4 mm and CAL >3 mm at the same site (17). Participants having no >4 mm pockets of teeth were regarded as periodontally healthy.
Definition of PTB, LBW and PLBW. Preterm delivery implies labor that occurs at fewer than 37 complete weeks of gestation, and is generally accompanied by low birth weight, i.e., a birth weight <2500 g. (18). Gestational age was calculated from the first day of the last menstrual period, or based on the results of ultrasonic examination, which was provided in the first trimester of pregnancy. A low birth weight babies information was taken from clinical records after delivery.
Diagnosis of Stress. The participants were asked to complete a simple evaluation instrument a well documented perceived stress test (the PSS-10) (19) in a Spanish version (20). The authors want to mention that this version does not have previously been validated in Colombia. The PSS-10 is a selfreported measure of global stress and measures the extent to which people find their life unpredictable, uncontrollable, and overwhelming. It consists of ten questions rated on a 5-point Likert scale ranging from "never" to "very often" (range: items 0-4, total 0-40). The more perceived stress is present when the score is higher.
Statistical data analysis. Descriptive statistics were used to assess demographic variables, BOP and obstetric information. With respect to Quigley-Hein, Sulcus Bleeding Indexes and stress level, means, and standard deviations were calculated. The comparisons among means were analyzed through ANOVA. The odds ratios (ORs) and 95 % confidence intervals (CI) were obtained to indicate an association between PTB, LBW and PLBW and the potential risk factors such as maternal periodontitis and stress. There was used Chi2 test and the significance level was set at p <0.05. Statistical analysis was performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
We enrolled 46 (41 %) of 112 consented women at the end of the follow up period. They met the inclusion criteria. The reasons for exclusion were mainly due to age, smoking habits and who had medical problems such as gestational diabetes and risk for pre-eclampsia. The mean age of the subjects was 22.2 years, SD=3.41. Regarding subjects' socio-economic status, all of those had a low household income. According to group obstetric data, 25 (53.2 %) were primiparous. Six mothers (13 %) had PTB babies, 2 (4.3 %) had LBW babies and 10 (21.7 %) showed PLBW.
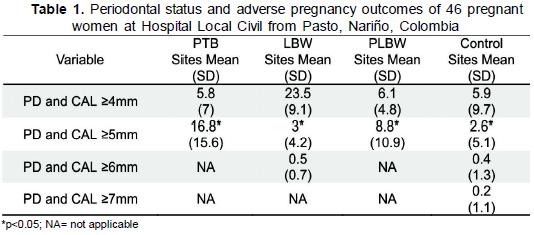
With respect to oral hygiene and gingival bleeding, these pregnant women showed a QuigleyHein Index (QHI) mean of 1.1; SD=0.6 and Sulcus Bleeding Index (SBI) mean was 1.4; SD=0.6. The percentage of BOP in these mothers was 85.4 %. The mean of sites with PD and CAL >5 mm per subject was greater in the PTB (p <0.05) and PLBW groups compared to the control group. The periodontal status of the sample is described in Table 1.
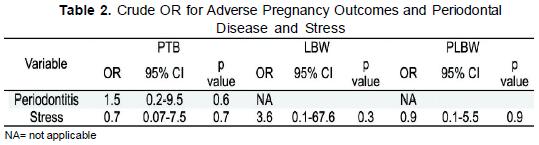
The frequency of maternal periodontitis was 32 (69.6 %) in the total group, 4 (12.5 %) in the PTB group, 2 (6.3 %) in the LBW group, 10 (31.3 %) in the PLBW and 16 (50 %) among women in the control group. The mean of perceived stress was 17.8; SD=5. The 21.7 % reported a higher perceived stress. Stress (OR=2. 95 % CI: 0.36-10.91; p=0.41) was associated with an increased risk for the development of periodontitis. The mean of sites with PD and CAL >4 mm per subject was greater in women with stress (9.2; SD=10.8; p=0.3). Maternal periodontitis was associated with PTB, while stress interacted with LBW (Table 2).
The 19.6 % had a (+) periodontitis and a (+) stress, 27 (58.7 %) presented a (+) periodontitis and (-) stress, 2 (4.3 %) showed a (-) periodontitis and (+) stress and 10 cases (21.7 %) had a (-) periodontitis and (-) stress. In table 3, maternal periodontitis has different risks of PTB, LBW and PLBW when interacts with stress. A lower PTB risk was observed when these subjects have higher levels of perceived stress, while a lower LBW was found when pregnant women did not experience stress. Individuals with periodontitis and no stress have an increase of PLBW risk.
Pregnant women experience metabolic changes that sometimes could alter their oral metabolism. These include alterations in the hormonal levels, microbial strains present in oral cavity, immune response and cellular metabolism (21). As a result, women may experience augmented gingivitis or pregnancy gingivitis beginning in the second or third month of pregnancy that increases in severity throughout the eighth month due to estrogen and progesterone levels increase in this period of time. (22).
Oral Hygiene, Gingival Bleeding and Periodontal Disease. Regarding oral hygiene, pregnant women had a QHI mean of 1.1; this value indicates that individuals had separate flecks of plaque at the cervical margin of the tooth. In addition, they showed a SBI score of 1.4 and a BOP of 85.4 %. The increase of bleeding is due to multiple changes of the circulatory system are characteristic during pregnancy, such as, vasodilatation and an increment in vascular proliferation (23). In this study, the mean of sites with PD and CAL >4 mm was higher in pregnant women with LBW babies (23.5) and of >5mm in PTB (16.8). Mafra-Siquiera et al. (24), in 2007 in a multiethnic group in low socioeconomic status observed that the highest mean of sites was in PD and CAL >4mm in PTB. The frequency of maternal periodontitis was 69.6 % this percentage was higher than one of Agueda et al. (25) study, where pregnant women presented 25.4 %. The PLBW had the highest prevalence of periodontitis (31.3 %). Socio-economic conditions can lead to different health outcomes. The study by Machuca et al. (26), in 1999 shows periodontal disease in pregnant woman has been associated with education and living in rural areas. Periodontitis had a slight association with PTB (OR=1.5; 95 % CI:0.2-9.5; p=0.6). This outcome is lower than the study by Bosnjak et al. (27) (OR=8.13; 95 % CI:2.73-45.9) or Lunardelli and Peres (28) (OR=2.6; 95% CI:1-6.9).
Stress. Stress is physical, mental or emotional response to events that causes bodily or mental tension, such as acute stressors that include unpleasant films, understimulation/work underload, overstimulation/work overload, unexpected or uncontrollable noise, prestige or status loss, electric shock, uncontrollable situations, physical illness, surgery, threats to self-esteem, and traumatic experiences; or chronic stressors like sleep deprivation, daily "hassles", work overload or underload, role strains, or social isolation (29). The mean of perceived stress in these pregnant women was 17.8; SD=5, this measure was higher than 16.8; SD=7.77 of female African American women (30). The 21.7 % showed a higher level of stress. Stress was associated with an increased risk for the development of periodontitis, which is consistent result with a previous report by Rosania et al. (31), in the same way; stress has also been associated with severity of periodontitis (32).
Stress did not interact with PTB, these results can be compared with the study by Hedegaard et al. (33), where there is no association between stress and PTB. It is well known that several substances are released during stress into the peripheral circulation that may influence negatively T biosynthesis such as 13-endorphin, glucocorticoids and catecholamines. However, stress may be a protective factor for preterm delivery, in stress experiences catecholamines plasma levels increases, this is why, there is a lower uterine contractile activity (34). Stress was related to LBW (OR=3.6). A study by Valladares et al. (35), in 2009, in Nicaragua showed that stressors provokes high levels of cortisol, which is associated with reduction of birthweight. Borders et al. (36), observed that multiple stress factors, including food insecurity OR=3.2; 95 % CI: 1.4- 7.2, a child with chronic illness at home OR= 3.4; 95 % CI: 1.5-7.9, increased crowding at home OR=2.7; 95 % CI 1.3-5.6, unemployment OR 3.1; 95 % CI: 1.2-7.9, and poor coping skills OR=3.8; 95 % CI: 1.7-8.7, were significantly associated with a low birthweight delivery. Furthermore, catecholamines secretion may compromise placental function, particularly if placental insufficiency already exists. The exposure to stress in the last trimester is particularly likely to lead to low birthweight through premature delivery. Uterine smooth muscle has a variable response to secretion of catecholamine during pregnancy that depends on hormonal climate. As term is approached stress is less likely to promote contractility and may even inhibit it. The timing of exposure to stressful events must also be important in this respect (37).
Periodontal disease, Stress and Adverse Pregnancy Outcomes. Periodontal disease, stress and pregnant adverse outcome dynamic depend on the presence or absent of stress. Our findings show that the presence of periodontitis and stress together increase the risk of LBW babies (OR=4.6). It has observed that "anemia of chronic diseases" (ACD) is a form of anemia which occurs in chronic infections, chronic inflammatory process, or tumor formation and is not the results of dysfunction of bone marrow cells. ADC develops despite adequate iron and vitamin intake (38). In these sense, Hutter et al. (39), show that patients with periodontitis who had lower levels of erythrocytes and hemoglobin were not due to iron or vitamin deficiencies. The Castaldi et al. (40) study, in 2006 reports that anemia increases the risk of LBW (OR=1.74; 95 % CI: 1.03-2.94; p=0.02) and Kidanto et al. (41), in 2009 also associate the anemia severity with an increase of LBW with OR=1.9 and OR=4.2 for very LBW. In response to stress, blood flow to the uterus is restricted and the fetus receives fewer nutrients, and those nutrients may have low levels of proteins because of periodontitis which may result in much more frequency of low birthweight.
In comparison with other studies, the OR of PLBW (10.3) in this report was higher than the investigation by López et al. (42) (OR=4.7 95 % CI:1.29- 17.13) or Khader et al. (43) (OR=4.2 95 % CI:2.62-6.99). Regarding, periodontitis and stress interaction, the risk of PTB (OR=0.9) and PLBW (OR=1.1) decreased in the presence of both, although their ORs were higher in the absent of stress (PTB, OR=2.3 and PLBW, OR=10.3). Diverse studies have suggested the levels of PGE2 and IL-1β inflammation mediators in gingival crevicular fluid were related to adverse outcomes pregnancy like PLBW (44,45). In addition, stress may be related to psychoneuroimmunologic changes, at risk health behavior, or a combination of both. Negative emotions prompt the release of polypeptides from the sympathetic noradrenaline-transmitting and sensory peptidergic nerve fibers and from endocrine glands. In turn, these hormones help to regulate immune responses triggered by bacterial antigens. In particular, the hypothalamus releases corticotropic - releasing hormone, which then stimulates the release of adrenocorticotropic hormone from the pituitary. In response, the adrenal cortex produces cortisol (CORT), and glucocorticoides (GCs) that helps to regulate inflammatory responses and lymphocytic activity (46). In this sense, stress may regulate the periodontitis inflammation mediators and to be a protective factor for PTB and PLBW.
In pregnancy period, it is possible that pregnant women may need certain stress levels to regulate different aggressors produced by the organism, among them periodontal disease. Stress promotes survival because it forces organisms to adapt to rapidly changing environmental conditions. This group of pregnant woman had higher stress levels in comparison with other women. The under developed countries enviroment is characterized by low income, unemployment, food insecurity, or diseases in the family that lead to stressful situations. For this reason, when a pregnant woman's response to stress is inadequate or when the stress is too powerful, problems may result such as LBW. The implication of these findings encourage to a keener assessment of stress experienced by women during their pregnancies. Further researches with different methods are necessary to establish and support the interactions of these variables in pregnant women, in order to control adverse pregnancy outcomes.
Acknowledgments: We thank to M.D. Alexander Jojoa for his explanations about pregnancy physiology, to Psychologist Edwin Luna Tascón, Department of Psychology, Universidad de Nariño, for his assistance in pregnant women group stress diagnosis. We are very grateful to students of dentistry Oswaldo Chicaiza Guerrero and Byron Chávez Arcos for enabling and supporting collection of periodontal diagnosis, and Comité Nacional para el Desarrollo de la Investigación (CONADI) at Universidad Cooperativa de Colombia for its financial support.
1. Organización Mundial de la Salud (OMS). Objetivos de Salud del Milenio: caminos hacia el futuro. [Internet]. Available from: http://www.who.int/whr/2003/chapter2/es/index3.html . Retrieved December 2008. [ Links ]
2. Wilcox AJ. On the importance - and the unimportance - of birthweight. Int J Epidemiol. 2001;30:1233-41. [ Links ]
3. Ministerio de la Protección Social. Organización Panamericana de la Salud (OPS). Situación de Salud en Colombia. Indicadores Básicos - 2008. [Internet]. Available from: http://www.minproteccionsocial.gov.co/VBeContent/NewsDetail.asp?ID=15895IDCompany=3 . Retrieved January 2009. [ Links ]
4. World Health Organization (WHO). Mortality and burden of disease indicators. Colombia-2000. Retrieved December 2008. [ Links ]
5. Ortiz EI. Estrategias para la prevención del bajo peso al nacer en una población de alto riesgo, según la medicina basada en la evidencia. Colomb Med. 2001;32:159-62. [ Links ]
6. Sacannapieco FA. Position paper of American Academy of Periodontology: periodontal disease as a potential risk factor for systemic disease. J Periodontol. 1998;69:841-50. [ Links ]
7. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809-20. [ Links ]
8. Contreras A, Herrera JA, Soto JE, Arce RM, Jaramillo A, Botero JE. Periodontitis is associated with preeclampsia in pregnat women. J Periodontol. 2006;77:182-8. [ Links ]
9. Scannapieco FA, Bush RB, Paju S. Periodontal disease as a risk factor for adverse pregnancy outcomes. A systematic review. Ann Periodontol. 2003;8:70-8. [ Links ]
10. Mokkem SA, Molla GN, Al-Jewair TS. The prevalence and relationship between periodontal disease and pre-term low birth weight infants at King Khalid University Hospital in Riyadh, Saudi Arabia.J Contemp Dent Pract. 2004;5:40-56. [ Links ]
11. Dailey DE.Social stressors and strengths as predictors of infant birth weight in low-income African American women. Nurs Res. 2009 ;58:340-7. [ Links ]
12. Malach-Pines A, Keinan G. Stress and burnout in Israel police officers during Palestinian uprising (intifada). Int J Stress Manage. 2007;14:160-74. [ Links ]
13. Cury PR, Araújo VC, Canavez F, Furuse C, Araújo NS. Hydrocortisone Affects the Expression of Matrix Metalloproteinases (MMP-1, -2, -3, -7, and -11) and Tissue Inhibitor of Matrix Metalloproteinases (TIMP-1) in Human Gingival Fibroblasts. J Periodontol. 2007;78:1309-15. [ Links ]
14. Cuenca-Sala E, Baca-García E. Odontología Preventiva y Comunitaria. Principios, Métodos y Aplicaciones. 2 Ed. Barcelona: Masson Editores; 2005. p.355. [ Links ]
15. Krüger KF. The Muhlemann-Son Sulcus Bleeding Index - its evaluation as a practice-relevant method for early recognition of periodontopathies using comparative measurements of the partial pressure of oxygen in the capillaries of the gingiva. Stomatol DDR. 1983;33:342-8. [ Links ]
16. Newbrun E. Indices to measure gingival bleeding. J Periodontol. 1996; 67: 555-61. [ Links ]
17. Lopez NJ, Smith PC, Gutierrez J. Higher risk of preterm birth and low birth weight in women with periodontal disease. J Dent Res. 2002;81:58-63. [ Links ]
18. World Health Organization (WHO). Low-birthweight newborns. Available from: http://www.who.int/whosis/indicators/2007LBW/en/index.html. Retrieved July 2009. [ Links ]
19. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385-96. [ Links ]
20. Remor E. Psychometric Properties of a European Spanish Version of the Perceived Stress Scale (PSS). The Spanish Journal of Psychology, 2006;9:86-93. [ Links ]
21. Amar S, Chung KM. Influence of hormonal variation on the periodontium in women. Periodontol 2000. 1994;6:79-87. [ Links ]
22. Löe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963; 21:533-51. [ Links ]
23. Lee RV. Symptoms produced by normal physiologic changes in pregnancy. In: Lee RV, Rosene- Montella K, Barbour LA, et al, editors. Medical care of the pregnant patient. Philadelphia: ACP-ASIM; 2000. p. 52-67. [ Links ]
24. Mafra-Siqueira F, Miranda-Cota LO, Costa JE, Amaral-Haddad JP, Quintão-Lana AM, Oliveira- Costa F. Intrauterine Growth Restriction, Low Birth Weight, and Preterm Birth: Adverse Pregnancy Outcomes and their association with Maternal Periodontitis. J Periodontol. 2007;78:2266-76. [ Links ]
25. Agueda A, Ramón JM, Manau C, Guerrero A, Echeverría JJ. Periodontal disease as a risk factor for adverse pregnancy outcomes: a prospective cohort study. J Clin Periodontol. 2008;35:16-22. [ Links ]
26. Machuca G, Khoshfeiz O, Lacalle JR, Machuca C, Bullón P. The influence of general health and sociocultural variables on the periodontal condition of pregnant women. J Periodontol. 1999;70:779- 85. [ Links ]
27. Bosnjak A, Relja T, Vuciáeviá-Boras V, Plasaj H, Plancak D. Preterm delivery and periodontal disease: A case-control study from Croatia. J Clin Periodontol. 2006;33:710-6. [ Links ]
28. Lunardelli AN, Peres MA. Is there an association between periodontal disease, prematurity and low birth weight? A population-based study. J Clin Periodontol. 2005;32:938-46. [ Links ]
29. Elliott CR, Eisdorfer C. Stress and human health: Analysis and implications of research. New York: Springer; 1982. 372p. [ Links ]
30. Simsa R, Gordona S, Garcia W, Clarka E, Monyea D, Callenderb C, et al. Perceived stress and eating behaviors in a community-based sample of African Americans. Eat Behav. 2008;9:137-42. [ Links ]
31. Rosania AE, Low KG, McCormick CM, Rosania DA. Stress, depression, cortisol, and periodontal disease. J Periodontol. 2009;80:260-6. [ Links ]
32. Arowojolu MO, Onyeaso CO, Dosumu EB, Idaboh GK. Effect of academic stress on periodontal health in Nigerians. Odontostomatol Trop. 2006;29:9-13. [ Links ]
33. Hedegaard M, Henriksen TB, Sabroe S, Secher NJ. Psychological distress in pregnancy and preterm delivery. Br Med J. 1993; 307: 234-9. [ Links ]
34. Lederman RP, Lederman E, Work BA Jr, McCann DS. The relationship of matermal anxiety, plasma catecholamines and plasma cortisol to progress in labour. Am J Obst Gynaecol. 1978;132:495-500. [ Links ]
35. Valladares E, Peña R, Ellsberg M, Persson LA, Högberg U. Neuroendocrine response to violence during pregnancy - impact on duration of pregnancy and fetal growth. Acta Obstet Gynecol Scand. 2009;88:818-23. [ Links ]
36. Borders AE, Grobman WA, Amsden LB, Holl JL. Chronic stress and low birth weight neonates in a low-income population of women. Obstet Gynecol. 2007;109:331-8. [ Links ]
37. Newton RW, Hun LP. Psychosocial stress in pregnancy and its relation to low birth weight. Br Med J. 1984;288:1191-94. [ Links ]
38. Loos BG. Systemic markers of inflammation in periodontitis. J Periodontol. 2005;76(11 Suppl):2106- 15. [ Links ]
39. Hutter JW, van der Velden U, Varoufaki A, Huffels RA, Hoek FJ, Loos BG. Lower numbers of erythrocytes and lower levels of hemoglobin in periodontitis patients compared to control subjects. J Clin Periodontol. 2001;28:930-36. [ Links ]
40. Castaldi JL. Bertin MS, Giménez . Lede R. Enfermedad periodontal: ¿es factor de riesgo para parto pretérmino, bajo peso al nacer o preeclampsia?. Rev Panam Salud Publica/Pan Am J Public Health 2006;19:253-58. [ Links ]
41. Kidanto HL, Mogren I, Lindmark G, Massawe S, Nystrom L.S. Risks for preterm delivery and low birth weight are independently increased by severity of maternal anaemia. Afr Med J. 2009;99:98-102. [ Links ]
42. López NJ, Smith PC, Gutierrez J. Periodontal therapy may reduce the risk of preterm low birth weight in woman with periodontal disease. A randomized controlled trial. J Periodontol. 2002, 73:911-24. [ Links ]
43. Khader YS, Ta'ani Q. Periodontal diseases and the risk of preterm birth and low birth weight: a meta-analysis. J Periodontol. 2005;76:161-5. [ Links ]
44. Konopka T, Rutkowska M, Hirnle L, Kopec W, Karolewska E. The secretion of prostaglandin E2 and interleukin 1-beta in women with periodontal diseases and preterm low-birth-weight. Bull Group Int Rech Sci Stomatol Odontol. 2003;45:18-28. [ Links ]
45. Konopka T, Rutkowska M, Hirnle L, Kopec W. IL-1beta and PGE2 production in whole blood and gingival fluid in women with periodontitis and preterm low birth weight. Ginekol Pol. 2004;75:352-60. [ Links ]
46. Breivik T, Thrane PS, Murison R, Gjermo P. Emotional stress effects on immunity, gingivitis, and periodontitis. Eur J Oral Sci. 1996;104:327-34. [ Links ]














