Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Salud Pública
Print version ISSN 0124-0064
Rev. salud pública vol.12 suppl.1 Bogotá Apr. 2010
Health Systems Governance for Health Equity: Critical Reflections
Gobernanza de sistemas de salud para logar equidad: reflexiones críticas
Ronald Labonté
Institute of Population Health, University of Ottawa. Canada rlabonte@uottawa.ca
Received 15th July 2009/Sent for Modification 23th December 2009/Accepted 18th January 2010
ABSTRACT
This article addresses several issues pertinent to health systems governance for health equity. It argues the importance of health systems using measures of positive health (well-being), discriminating in favour of historically less advantaged groups and weighing the costs of health care against investments in the social determinants of health. It cautions that the concept of governance could weaken the role of government, with disequalizing effects, while emphasizing the importance of two elements of good governance (transparency and participation) in health systems decision-making. It distinguishes between participation as volunteer labour and participation as exercising political rights, and questions the assumption that decentralization in health systems is necessarily empowering. It then identifies five health system roles to address issues of equity (educator/watchdog, resource broker, community developer, partnership developer and advocate/catalyst) and the implications of these roles for practice. Drawing on preliminary findings of a global research project on comprehensive primary health care, it discusses political aspects of progressive health system reform and the implications of equity-focused health system governance on health workers' roles, noting the importance of health workers claiming their identity as citizens. The article concludes with a commentary on the inherently political nature of health reforms based on equity; the necessary confrontation with power relations politics involves; and the health systems governance challenge of managing competing health discourses of efficiency and results-based financing, on the one hand, and equity and citizen empowerment, on the other.
Key Words: Governance, government, primary health-care, community participation, social conditions, poverty, public health practice, healthcare systems (source: MeSH. NLM).
RESUMEN
El artículo toca diferentes aspectos relacionados con la gobernanza de sistemas de salud para lograr la equidad. Examina la importancia de los sistemas de salud que utilizan medidas de salud positiva (bienestar) y se concentran a favor de los grupos históricamente en desventaja, ponderando los costos de la atención en salud con respecto a la inversión en los determinantes sociales de la salud. Se advierte que el concepto de gobernanza podría debilitar el papel de gobierno, con efectos distorsionadores, mientras enfatiza la importancia de dos elementos de una buena gobernanza (transparencia y participación) en los sistemas de decisión en salud. Se hace la distinción entre la participación como una labor voluntaria y como un ejercicio de derechos políticos, preguntado sobre el supuesto de que la descentralización de los sistemas de salud necesariamente significa empoderamiento. Se identifican cinco roles de los sistemas de salud que apuntan a temas de equidad (educador, vigilante, gestor de recursos, desarrollo comunitario, desarrollo de asociaciones y abogacía/catalizador) y las implicaciones de estos roles en la práctica. Considerando los hallazgos preliminares de un proyecto de investigación global sobre atención primaria en salud integral, discute los aspectos políticos de la reformas progresivas de los sistemas de salud y las implicaciones de la gobernanza de los sistemas de salud enfocados en la equidad sobre la salud de los trabajadores, haciendo notar la importancia de los reclamos de los trabajadores por su identidad como ciudadanos. El artículo concluye con un comentario sobre la inherente naturaleza política de las reformas basadas en equidad; la necesaria confrontación con las relaciones políticas involucradas; y el desafío que significan para la gobernanza los discursos de la competencia gerenciada de eficiencia y financiamiento basado en resultados, de una parte, y la equidad y el empoderamiento ciudadano, por otra parte.
Palabras Clave: Gobernanza, gobierno, atención primaria de salud, participación comunitaria, condiciones sociales, pobreza, sistemas de salud (fuente: DeCS, BIREME).
In examining governance for health equity, several questions immediately arise. What do we mean by health? How do we define equity? What constitutes governance? Beneath these questions is a more challenging one: What role does community participation play in governance? And at a more fundamental level: How can health systems respond to unequally allocated determinants of health? What role does comprehensive primary health care play in such a response? How do politics and ideology shape health systems reform? What are the implications for health workers? This article offers some personal reflections on these questions. It draws, in part, on thirty years experience in public and community health in many parts of the world; and findings-to-date from a recent research program studying how comprehensive primary health care can better promote health equity (1).
The Question of Health
Health systems are dominated by measures of death, disease and disability. This is due partly to positive health experiences being difficult to measure, but there is a paradox: people with a disability or a disease (especially when chronic) often report feeling healthy. This paradox has underpinned numerous efforts to define 'positive' health in terms of peoples' capabilities, from the World Health Organization's operationally troublesome: 'state of complete physical, mental and social well-being and not merely the absence of disease and infirmity' (2); to the Ottawa Charter's utilitarian: 'resource for everyday life' (3) to the Bangkok Charter's subordinating qualification: 'a determinant of quality of life...encompassing mental and spiritual well-being' (4). Biomedical constructs of positive health which emphasise normal physical functioning do not offer much improvement: How are deviations from the norm defined?
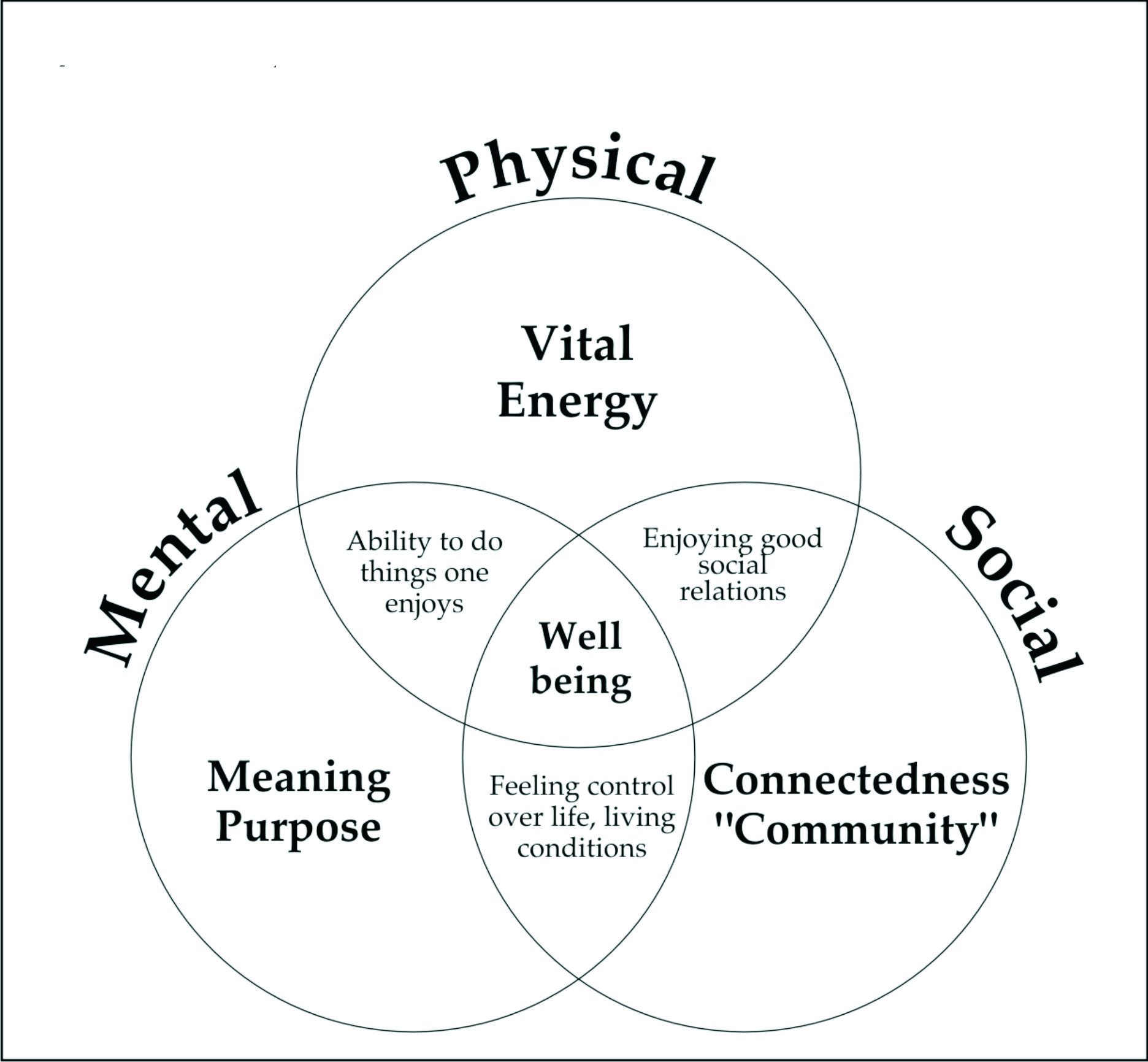
Despite these definitional difficulties and on the assumption that what is measured is what gets noticed, some routine diagnosis of how 'well' a population is doing becomes as important to track as how long, disease-free and minimally disabled (or disability-enabled) people are able to live. Population surveys frequently use 'self-rated health' as a proxy measure for well-being, but other dimensions of health are also worth assessing. Some years ago, based on a review of the literature, I created a simple model of the key domains of positive health. By chance (not design) these mapped conveniently against the WHO's triad of physical, mental and social well-being (Figure 1).
There is an evidence-informed argument around this model: to be healthy, one needs a sense of meaning or purpose in life, connection to others in community and physical vitality or energy. One also needs some control over one's life and living conditions, a function of both community connectedness (social solidarity enhancing the means of control) and personal meaning (knowing what is important to control). The hedonistic aspect of health, the ability to do things one enjoys, intersects between personal meaning (what one finds pleasurable) and physical vitality (the ability to participate). Finally, capacity for good social relationships requires a base upon which to draw (community connectedness) and energy (physical vitality) with which to engage (5).
The implication of this model (which makes no claim to universalism but some claim to heuristic usefulness) is that health systems, the workers within them and the services and programs they offer have an obligation to account for how they assist people to flourish across a range of dimensions. The model also infers two other health system responses: participation in the creation of alternative social indices of well-being that counter the well-known limitations of the narrowly economic measures comprising the GDP (see for example the new 'Canadian Index of Well-Being' (6); and attention to the quality of the relationships that occur between health care workers and patients, and more broadly between health systems and the communities they serve. Disrespectful relationships and poor services, often an effect of under-resourced public health systems, are two of the most frequent reasons why even poor people will choose a private provider over a public facility despite the cost (1,7).
The Question of Equity
Equity is a normative judgement of what is fair. Applied to health, it is an assessment of whether inequalities between individuals or population groups in measures of health are significant in size and number of people affected, preventable through policy or other intervention and not an effect of freely-chosen risk. Health inequities almost invariably reside in social inequities (8) that reflect systems of social stratification: class, gender, ethnoracial background, geography and various forms of discrimination or 'social exclusion'. Underpinning the concept of equity is social justice, which is argued to be a universal concern since all social arrangements, to be legitimate and to function, must give some attention to social equality (9). There are two principle theories of social justice:
The first, and politically dominant, theory holds to the importance of ensuring that everyone 'plays by the same rules' - there is no discrimination. Fairness is judged by equality in process. The second, and politically challenging, theory holds to the importance of ensuring that rules work to minimize preventable differences in outcomes between the players (10).
Equal opportunity (the first theory) for unequal people, however, will only result in unequal outcomes. To be just, equal opportunity requires a disproportionate provision of public goods and capability resources for those whom history's conquests and today's political institutions place in highly unequal initial conditions. In effect, opportunity must be more than equal; it must discriminate positively in favour of those groups who start the 'game' of social and economic life with fewer resources:
A better understanding of the importance of inequality of opportunity in the determination of inequality of outcomes may change attitudes towards redistribution. People dislike and consider unfair inequalities associated with differences in circumstances, which many argue should be compensated for by society (11). There are at least four equity implications for health systems. First, it is well known that better-off urban groups often benefit disproportionately in access to public health services, especially given their already lower burden of disease (12). Health systems need to 'pay the equity premium' (13) to benefit more those in greater need. Second, this cost must be weighed against investments to make more equitable access to other social determinants of health (e.g. water and sanitation, housing, employment, education, early childhood development, transportation, safety/security, social protection) (8,14). Third, equity in access to both health systems and social determinants of health can be improved through single-payer, progressively funded public programs that minimize out of pocket expenditures by the poor and redistribute more fairly opportunities for health (15). In advanced economies, social democratic states that invest heavily in public programs, including but not restricted to health services, generally experience lower rates of poverty, and better and fairer population health outcomes (16,17). Fourth, improving primary health care (PHC), which favours poorer, sicker populations, is more health-equitable than improving tertiary care, which favours wealthier, healthier populations (1,7,18).
The Question of Governance
How health systems might be reformed or strengthened to improve health equity raises the matter of governance, a term of recent coinage and mixed implications.
To critics, the idea of governance risks undermining the role of government in policy and program activity by passively or actively promoting decision-making by a polycentric blend of 'stakeholders', often dominated by powerful individual and corporate actors. This model of governance derives from new public management theory, and is consistent with the neoliberal principle that states should 'steer ' but not 'row' (direct but not do) (19). The implied danger is that the 30 percent or so of overall global economic product that is presently generated through government services provision will become increasingly contracted to private, for-profit companies (20,21). While (perhaps) temporarily set-back by the global recession and renewed contractual protectionism (e.g.: 'Buy America') (22) for the past two decades there has been a concerted effort to open all government procurement contracts to unfettered global competition. Such competition under skewed capacities in the private services market is likely to lead to 'disequalizing' economic (and hence related health) effects within and between nations (23).
To proponents of the concept, however, governance is broader than its neoliberal imputation, with an empowering community/citizen potential insofar as it refers to all forms of organized decision-making towards shared social goals, and not merely to acts of government. This, in turn, demands an opening of government processes to greater and more real-time forms of public input (24). The key attributes against which 'good' governance is generally appraised are: transparency, participation, representation, accountability and resource mobilization (25). Each has implications for how decisions in health systems are made, although only the first two are considered in this brief article.
Transparency: There are three levels at which transparency in health systems decision-making is critical for health equity. At the local level, there must be access to information about health (negative or positive) and its key social determinants. In many poorer countries such information is not available simply because it is not routinely gathered; witness the large number of births that continue to go unrecorded (7). In other instances the information may be available but inaccessible, either to local level health services or to the community members they serve. Or, when accessible, the information is presented in a technical manner that is alien to community members and retains power amongst professionals/experts who then interpret it (26). At a national level, there is access to the deliberations surrounding health system policies, and to documentation of the policies themselves. More elusive, and linking the national to the global, are the constraints placed on many developing countries through aid, multilateral financing for health and global financial markets. Decisions by donors and global health initiatives are rarely fully transparent and their disbursements do not necessarily correspond with the needs or interests of recipient governments (27). There is a long history of conditional or recommended health system reforms associated with loans or grants from the World Bank and International Monetary Fund; and an even longer history of poor transparency and unequal decision-making power within these institutions (24,25). A neglected influence on health system reform is the role of global financial markets (including bond-rating agencies) which assess the credit-worthiness of nations that, in turn, affects their cost of borrowing. Countries developing policies seen as insufficiently market-friendly (such as increasing public health and social protection spending, or progressivity in taxation) may be given a poor rating, in some instances prompting them to abandon such policies (23).
Participation: Lack of transparency is associated with poor processes of participation that inhibit citizens' efforts to hold health systems accountable. Community participation is an oft-cited component of effective PHC, including sustaining demand for equitable service access and program activities, especially after short-term (often external) funding ceases (1). It is also associated with improved health outcomes, although the quality of such evidence remains poor (1). Moreover, in any consideration of improved participatory mechanisms, three issues immediately arise.
First: participation in what? While an active citizenship is seen as healthier (participation as an end in itself) (28), participation is always in relation to some task or purpose. In Canada and the United States, community participation in primary health care often arose in response to inadequate access to services, or to specific threats to community health (1); it was an expression of political rights or entitlements. In many poorer countries subject to international aid or loans for health system reform, participation often meant (and sometimes still means) voluntary labour to build or maintain facilities, assist in basic care provision or share in the cost of the service; that is, it is promoted to fill gaps in financing rather than to exercise the right to influence policy-making (1) In wealthier nations, citizen participation in established services often became little more than encouraging people to attend specific health education or health promotion programs developed by health authorities with little or no input from local residents (26). Health system governance should not prejudice one form of participation over the other (political activism vs. volunteer labour, program decision-maker vs. recipient) but to ensure multiple means that allow people to choose what, and how, they engage with their health systems.
Second: participation by whom? This question concerns who is meant by 'community.' Community has several dimensions: geographic (the most commonly invoked), affinity (self-defined group membership) and idealized (locally inclusive solidarity) (10,26). But there is rarely an inclusive geographic community and, instead, multiple affinity communities within any given area that often stretch beyond local boundaries. Community for health systems often is little more than the catchment area of a given service, whose borders may change with political whim and bear little or no relationship to how people consider their sense of identity (26). Or community is constructed by reference to 'target groups' whose targeting is defined by health authorities on the basis of statistical risk and not by citizen sensibility. There is a need, then, for health systems to consider carefully the implications of 'community,' the most precise meaning of which is simply that of a group of people for whom membership forms part of their identity. Apart from very small villages, some triage is required in selecting which groups community health workers seek to organize or support for their participation, whether in programs, services or political actions. This demands greater reflexivity and transparency for how health systems make such a determination; and touches on the need to examine the representativeness of community participants themselves. Given primary health care's concerns with equity, it also means removing financial or other barriers to participation, and special efforts to elicit the voices of the most marginalized people or groups.
Third: participation where? Just as community is often idealized, so, too, it is often seen as the best locus for health system decision-making. The closer to the daily lives of people, the more responsive to local needs are programs or services; therein lays the defence for health system de-centralization. While tightly centralized systems can choke local innovation, there is actually little empirical evidence that de-centralized health systems perform better on most metrics of health outcomes (29). There is also a risk that de-centralization becomes a means of offloading financial responsibility for services to local levels, in the guise of increasing community authority (30). Without careful disbursements by need, wealthier areas (better organized and politically positioned or connected) may capture more of the de-centralized resources; or in the case of community insurance schemes entrench or multi-tiered levels of care stratified by geographic wealth. Equitable local participation in health systems thus requires conduits to central levels of political decision-making, if potentially inequitable constraints of decisions made at that level are to be avoided, or at least challenged (26).
The Question of Health System Responsiveness
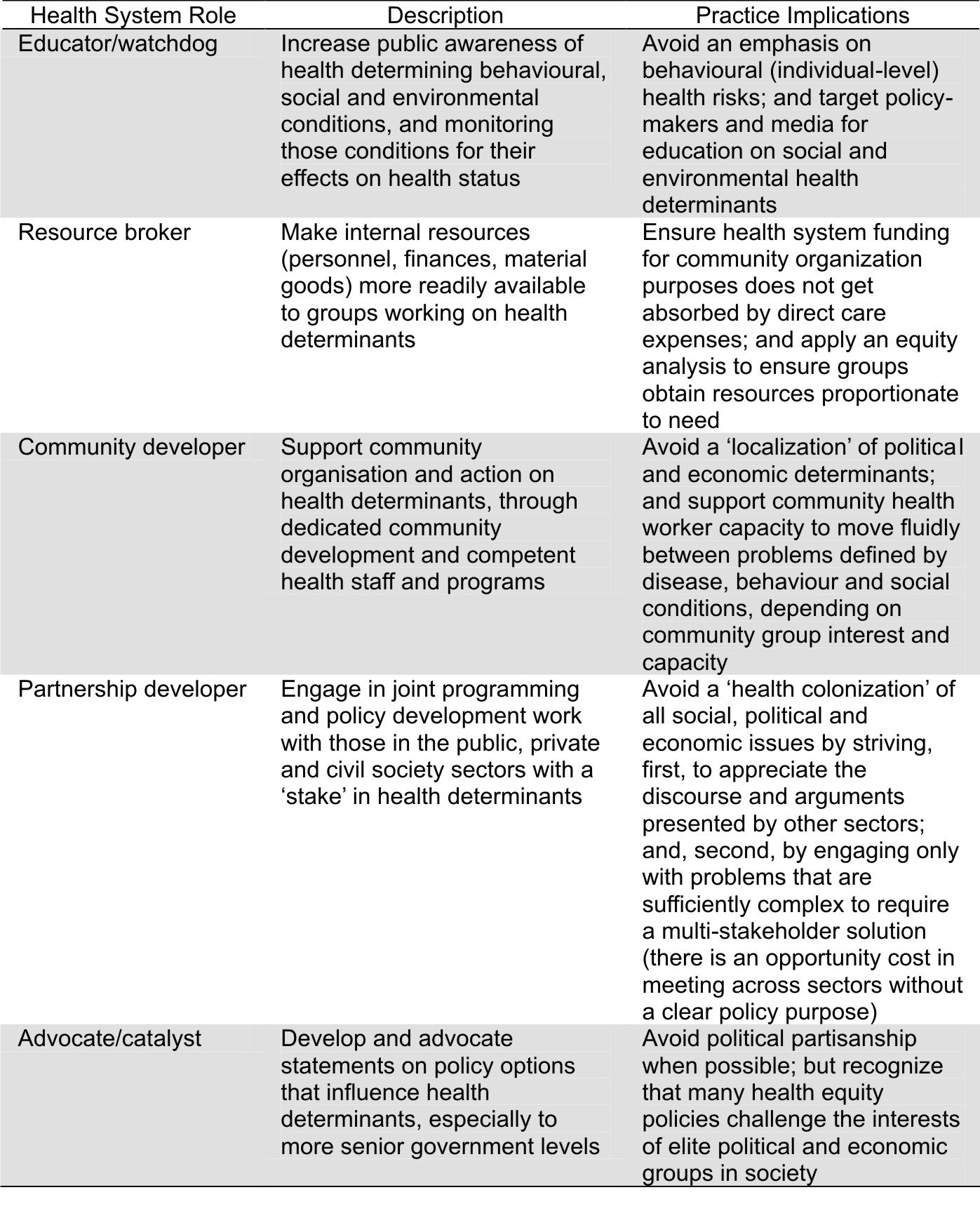
How health systems go about supporting a more politicized form of participation addressing not only health care access, but improved equity in the social determinants of health, raises the issue of responsiveness. Box 1, based on a study of population health capacity in Canada, summarizes five health system roles and some of the practice implications associated with them.
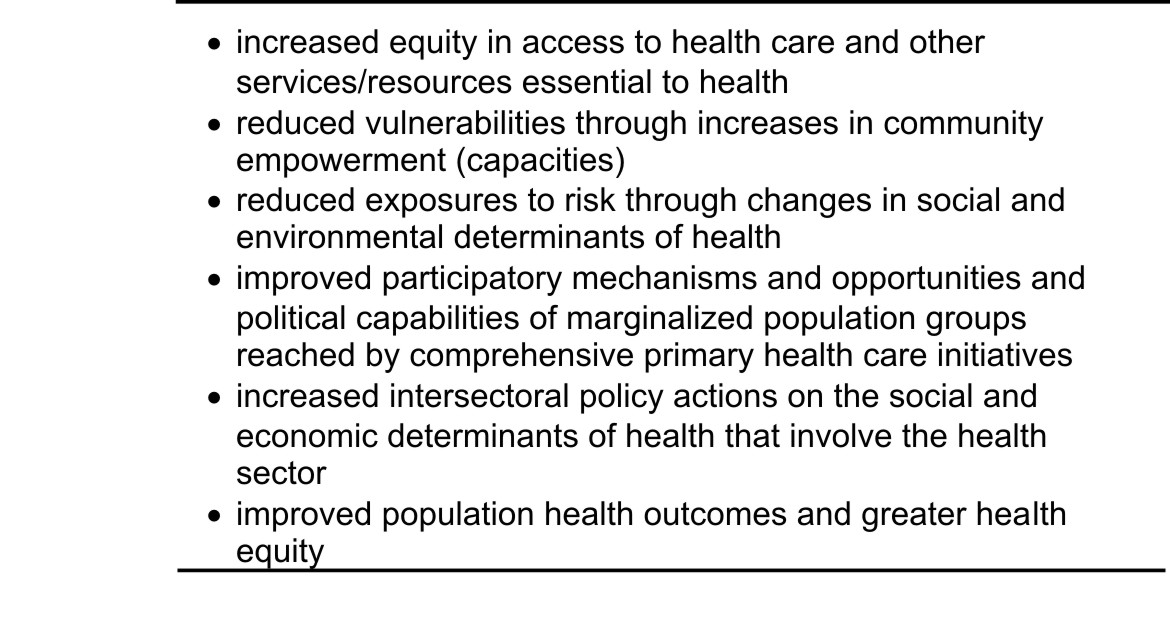
The final point in this Box, concerning the issue of politics in health systems' efforts to promote more equitable health-determining conditions, was highlighted by evidence of comprehensive primary health care experiences, notably in South Asia and in Latin America. The narrative review of scientific and grey literature sought evidence for health systems' responsiveness to a range of outcomes that were based on the cumulative experiences of over a dozen senior PHC researchers representing every region of the world (Box 2).
A review of South Asian grey literature found that programs fell into three types: those that primarily emphasized community involvement in health care services; those that saw PHC as including income generation, agriculture and other service sectors; and those that saw PHC as a means to engage communities in a more far-reaching empowerment project (1). Programs sponsored by non-governmental organizations were more likely to align with the last two approaches and less likely than government programs to prioritize only basic care provision. Both gave some attention to the social determinants of health, although country wide government programs less so. In sum, non-governmental programs were generally more responsive to the political claims of citizens than were governmental programs.
Similar experiences were recounted in North America, where community health centres that were born in struggles for access and empowerment sometimes settled into more service delivery and less community mobilization with increased public funding and government oversight (1). This is not an insuperable problem, since explicit health system mandates for community empowerment and health advocacy, together with protected funding for such activities, can retain a vibrant health activism in keeping with the outcomes listed in Box 2 (26). But such mandates are politically neutral. The Latin American component of our study found that comprehensive PHC was more likely (and more effective) 'in countries that included political commitments to equity, a legal or constitutional right to health guaranteed by the state, and where policy clearly identified primary care, community participation and intersectoral action as PHC components' (1). Such commitments are associated more with social democratic than with conservative political parties. Efforts to make PHC more comprehensive have sometimes become sites of political struggle and repression, as was the case in some Central American countries during the 1980s and 1990s, occasionally leading to dangerous working environments for those committed to a comprehensive vision of PHC (1).
The Question of Health Worker Role
The experience of community health workers committed to outcomes of equity under periods of political repression begs comment on the implications of a comprehensive PHC for practice. Box 1 in broad strokes identifies a number of working styles associated with improved equity that health systems should increasingly embrace. But providing respectful (as well as effective and efficient) care remains the bedrock of, and political legitimacy, for health systems. Most health workers will not function as social animateurs, nor need they be; moreover, most lack the skills to do so (26). Ensuring that some health workers can and do occupy the role niches in Box 1 suffices.
But there has long been an artificial divide in the community health literature between 'health systems' and 'community' and between 'health worker' (regardless of health system role) and 'citizen,' which can be laid to rest through a brief re-consideration of the idea of participation. Two anecdotes illustrate the point being made.
In the first, a health worker engaged community groups in a process of drafting a policy report on housing as a public health issue. The groups had been looking for an entry into policy influence and believed this presented an opportunity. But after several meetings to revise the recommendations (seen by the health system as too provocative) the community groups quit the process with feelings of being used or manipulated. They had not been; the health worker had been genuine with the invitation. But the health worker has also confused participation in a bureaucratic process of evidence-gathering with participation in a political process of policy-demands. Government departments rarely make bold policy statements. Citizens groups hold that entitlement. But government departments can provide good evidence supporting citizen demands. The participatory agenda thus becomes a strategic one: how do health workers and health systems engage with community groups in a process of social change, in which the powers and authority of their respective positions are brought separately, but in concert, to bear on the policy issue?
In the second, after a long participatory day of learning about community participation in health, one of the attendees confronted me with the question: 'But how can we get our community members to be more interested in participating in our programs and activities?' None of the content or lessons generated during the day had found a place to stick with this health worker. In an effort to have her answer her own question (believing people usually are repositories of knowledge that awaits only the right interrogative) I replied simply: 'What motivates you to participate in local programs and activities?' Her face looked even more puzzled, and the question answered itself. To affirm it, I asked for a show of hands of health workers who had recently engaged in some volunteer, community good activity. Of seventy attendees, perhaps ten hands were raised. The workshop ended with my statement: 'Until you as health workers become active citizens, you will never understand how to invite citizens to become active participants.'
Health workers are citizens, regardless of their functional role within health systems. Our ability to promote greater health equity is not simply a function of our jobs. It is a responsibility of our citizenship.
Conclusion
Working through the main ideas in this highly condensed article, what general conclusions might be drawn?
First, promoting health equity is an inherently political act. 'Politics' has a long etymological history that began with cities (polis) and their citizens (polites), evolving in use to refer to governing decisions (policies) that are wise, prudent and judicious. The heart of politics is citizenship and the right of people to participate in collective decisions that affect their lives. This right, in turn, rests on people determining which collective decisions are important to their lives. Too often health workers and health systems have defined these decisions as individualized lifestyle choices rather than systemically structured inequalities ('social determinants').
Second, political acts involve power, inevitably so when equity (fairness) and changes in existing systems of social stratification begin to define health system goals. In terms of fairness, publicly-financed primary health care disproportionately benefits poorer groups in access, outcome and economic redistribution (31). But to be effective, PHC needs sufficient financing based on a cross-subsidy from rich to poor and from healthy to sick: i.e., progressively financed universal insurance. Achieving such financing can challenge the economic power of elite groups. To attend to changing inequalities in social determinants of health, PHC must strive for comprehensiveness: 'paying the equity premium' to ensure services are accessible by need, protecting resources for community organization and action, working across government and state/civil society sectors in 'healthy public policy' formation and advocating against elite group power that may threaten progressive health change. These actions, too, require in the argot of social activists, 'speaking truth to power'. Therein lays the possibility of a more comprehensive PHC.
Third, there are many examples of where these actions have been attempted; although few where they have become characteristics of whole health systems. Strategies for advancing towards PHC-oriented health systems that are both equitable and comprehensive are known. So, too, are the main enabling contexts: political leadership supportive of social democracy, organized civil society, champions within public health bureaucracies, pluralistic media, cross-class solidarity (champions within elite groups). Where these are lacking, health workers face an ethical imperative to help in their creation. I refer to it as an ethical imperative since failure to do so is likely to lead to a morally indefensible increase in health disparities.
Fourth, while some low- and middle-income countries, including several in Latin America, are increasing the breadth of universality in coverage and depth of their PHC orientation, others, including some high-income countries, are increasing the role of private markets in financing and delivery. Even as health has risen dramatically in global policy debate, the financial crisis is threatening reductions in aid or other multilateral transfers for health (of importance to least developed countries); or a triage of health assistance based on the national security or economic self-interests of donor nations. A discourse of improving health system effectiveness and efficiency co-exists and challenges one premised more on health system equity. Within the same country or region, one can find health policy pronouncements calling for reductions in social inequities while imposing results-based funding models; proclaiming the importance of 'money for what is valued' while espousing the necessity of 'value for money'; holding health as a human right while engaging in trade talks to commodify its global exchange. The most important health systems governance challenge of the moment may well be negotiating these competing health frames.
Fifth and finally, other challenges loom larger on the horizon: the world-wide rise in chronic disease, no longer supplanting infectious disease in a mythical epidemiological transition but co-existing in multiple burden; the greying of the world, with increasing age-dependency ratios in developing, as well as developed, countries; the frailty of the (still dominant) neoliberal global economic model to be sustainable, whether in terms of health, environment or poverty reduction; and the arrival of climate change.
Enumerating these challenges is easy; planning for them is not. That these challenges are not exclusive to health systems or health workers offers some comfort. It also underscores the importance of strengthening health system capacities in the roles identified in Box 1. In such actions lies the optimism essential to any healthful future, a state of being that I have come to regard less as a personal disposition than as a fundamental of effective politics.
REFERENCES
1. Labonté R, Sanders D, Baum F, Schaay N, Packer C, Laplante D, et al. Implementation, Effectiveness and Political Context of Comprehensive Primary Health Care: Preliminary Findings of a Global Literature Review. Australian Journal of Primary Health 2008; 14(3): 58-67. [ Links ]
2. World Health Organization (WHO). Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. New York; 19-22 June, 1946. [ Links ]
3. World Health Organization (WHO). Ottawa Charter for health promotion. Ottawa: World Health Organization, Health and Welfare Canada, Canadian Public Health Association; 1986. [ Links ]
4. World Health Organization (WHO). The Bangkok Charter for Health Promotion. Geneva: World Health Organization; 2005. [ Links ]
5. Labonté R. Health Promotion and Empowerment: Practice Frameworks. Toronto: Centre for Health Promotion/Participation; 1993. [ Links ]
6. The Canadian Index of Wellbeing [Internet]. Site: http://www.ciw.ca/en/Home.aspx Accessed July 9 2009. [ Links ]
7. World Health Organization (WHO). Primary Health Care: Now More Than Ever. Geneva: World Health Organization; 2008. [ Links ]
8. Commission on Social Determinants of Health. Closing the Gap in a Generation: Health equity through action on the social determinants of health (final report). Geneva: World Health Organization; 2008. [ Links ]
9. Sen A. Inequality Reexamined. Oxford: Oxford University Press; 1992. [ Links ]
10. Labonté R, Laverack G. Health Promotion in Action: From Local to Global Empowerment. London: Palgrave Macmillan; 2008. [ Links ]
11. De Barros RP, Ferreira FHG, Vega JRM, Chanduvi JS. Measuring Inequalities of Opportunities in Latin America and the Caribbean. Washington: The World Bank; 2009. [ Links ]
12. O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M [Internet]. Analyzing Health Equity Using Household Survey Data,.Washington: The World Bank; 2008. www.worldbank.org/ analyzinghealthequity (Last accessed July 9 2009). Labonté - Governance for health equity 76 REVISTA DE SALUD PÚBLICA · Volumen 12 sup (1), Abril 2010 [ Links ]
13. de Savigny D, Kasale H, Mbuya C, Reid G. Fixing Health Systems. Ottawa, ON: International Development Research Centre; 2005. [ Links ]
14. Labonté R. Health care spending as a risk to health. Canadian Journal of Public Health 1990; 81(4): 251-2. [ Links ]
15. Gilson L, Doherty J, Loewenson R, Francis V [Internet]. Challenging inequity through health systems: Final Report of the Knowledge Network on Health Systems, World Health Organization Commission on Social Determinants of Health; 2007. Site: http://www.who.int/social_determinants/resources/csdh_media/hskn_final_2007_en.pdf. Accessed July 9 2009. [ Links ]
16. Navarro V, Shi L. The political context of social inequalities and health. In: Navarro V (Ed.) The political economy of social inequalities: Consequences for health and quality of life Amityville, NY: Baywood; 2002. pp. 403-418. [ Links ]
17. Lundberg O, Ygnwe MA, Stjarne MK, Bjork L, Fritzell J. NEWS: The Nordic Experience Welfare States and Public Health. Stockholm, Sweden: Centre for Health Equity Studies; 2008. [ Links ]
18. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank Quarterly. 2005; 83(3):457-502. [ Links ]
19. Osborne D, Gaebler T, Reinventing Government: The Five Strategies for Reinventing Government. New York: Penguin; 1993. [ Links ]
20. Labonté R. Globalization, Health and the Free Trade Regime: Assessing the Links. In: Harris R, Seid M (Eds.) Globalization and Health. Boston: Brill; 2004.pp. 47-72. [ Links ]
21. Alford J, O'Neill D (Eds). The Contract State: Public Management and the Kennett Government. Melbourne: Deakin University Press; 1994. [ Links ]
22. Baldwin R, Evenett S (Eds) [Internet]. The collapse of global trade, murky protectionism and the crisis: Recommendations for the G20, London: Centre for Economic Policy Research, Vox.EU.org; 2009. Site: http://www.voxeu.org/index.php?q=node/3199 Accessed March 23, 2009. [ Links ]
23. Labonté R, Blouin C, Chopra M, Lee K, Packer C, Rowson M et al [Internet]. Towards healthequitable globalisation: Rights, regulation and redistribution. Final Report of the Globalization Knowledge Network, World Health Organization Commission on Social Determinants of Health. 2008. Site: http://www.globalhealthequity.ca/electroniclibrary/GKNFinalJan82008.pdf Accessed July 9 2009. [ Links ]
24. Lee K, Koivusalo M, Ollila E, Labonté R, Schrecker T, Schuftan C et al [Internet]. Globalisation, global governance and the social determinants of health: A review of the linkages and agenda for action. Globalization Knowledge Network, World Health Organization Commission on the Social Determinants of Health. 2008. Site: http://www.globalhealthequity.ca/projects/ proj_WHO/index.shtml Accessed July 9 2009. [ Links ]
25. Lee K, Koivusalo M, Ollila E, Labonté R, Schuftan C, Woodward D. Global governance for health. In Labonté R, Schrecker T, Packer C, Runnels V, editors. Globalisation and Health: Pathways, Evidence and Policy. London: Routledge; 2009. pp. 289-316. [ Links ]
26. Labonté R. A Community Development Approach to Health Promotion. Edinburgh: Health Education Board of Scotland/Research Unit in Health and Behaviour Change; 1998. [ Links ]
27. Taylor S [Internet]. Aid and health. Globalization Knowledge Network, World Health Organization Commission on the Social Determinants of Health. 2008. Site: http://www.globalhealthequity.ca/projects/proj_WHO/index.shtml Accessed July 9 2009. [ Links ]
28. Labonté R, Laverack G. Capacity Building in Health Promotion: For Whom? And For What Purpose? Critical Public Health 2001; 11(2):111-27. [ Links ]
29. Bossert T, Beauvais J. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy and Planning 2002; 17(1):14-31. [ Links ]
30. Labonté R. Community, community development and the forming of authentic partnerships. In: Minkler M (Ed.) Community Organizing and Community Building for Health (2nd edition). New York: Rutgers University Press; 2003. p. 82-96. [ Links ]
31. Yazbeck A. Attacking inequality in the health sector: a synthesis of evidence and tools. Washington: World Bank; 2009. [ Links ]