Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Salud Pública
versión impresa ISSN 0124-0064
Rev. salud pública vol.17 no.1 Bogotá ene./jun. 2015
https://doi.org/10.15446/rsap.v17n1.36202
http://dx.doi.org/10.15446/rsap.v17n1.36202
Artículo/Investigación
Healthcare plans and consumer perceptions of healthcare institutions
Regímenes de salud y percepciones del consumidor acerca de las instituciones de salud
Ana M. Arboleda-Arango
Department of Marketing and International Business. ICESI University, Cali, Colombia. amarboleda@icesi.edu.co
Received 19 December 2012/Sent for Modification 5 July 2013/Accepted 15 Jun 2014
ABSTRACT
Objective This study evaluates the effect of healthcare insurance plans on consumer perception of trust in a healthcare institution, and the mediating effect of trust on consumer loyalty towards an institution.
Method The study was conducted at a healthcare institution in Colombia where a total of 841 patients responded to a questionnaire.
Results A structural equation model shows that individuals who have a pre-paid healthcare plan have a stronger evaluation of trust compared to those who hold a regulated healthcare plan (i.e., subsidized and contributory plans). In turn, trust positively predicts consumers' loyalty towards an institution. The relationship between the patients' healthcare plans and their degree of loyalty towards healthcare institutions is completely mediated by their perception of trust towards the institution.
Discussion A greater perception of trust is explained by having a medical plan that provides consumers with more flexibility, allowing them to select their health provider at a premium price. Although health institutions do not control healthcare regimes, these affect consumers' trust in their service. Institutions cannot modify characteristics of the regime, but they can promote a trustworthy environment to strengthen consumers' loyalty to the institution.
Key Words: Trust, health insurance, Colombia (source: MeSH, NLM).
RESUMEN
Objetivo Este estudio evalúa el efecto de los planes de salud hacia la percepción de confianza del consumidor en una institución de salud y el efecto mediador de la confianza hacia la lealtad del consumidor de dicha institución.
Metodología Este estudio fue realizado en una institución de salud en Colombia donde un total de 841 pacientes contestaron un cuestionario estructurado.
Resultados Un modelo de ecuaciones estructurales muestra que los individuos que tienen medicina prepagada tienen una evaluación más fuerte de su confianza en la institución en comparación con aquellos que tienen un plan de salud con mayores regulaciones (i.e., subsidiado y contributivo). A su vez la confianza predice positivamente la lealtad del consumidor hacia una institución. La relación entre el plan de salud del paciente y su grado de lealtad hacia la institución está totalmente mediada por su percepción de confianza hacia la institución.
Discusión Una mayor percepción de confianza se explica al tener un plan de medición que dé a los consumidores mayor flexibilidad, permitiéndoles elegir su prestador de servicios de salud a un mayor precio. Aunque las instituciones de salud no controlan los regímenes de salud, estos afectan la confianza del consumidor en el servicio. Las instituciones no pueden modificar las características del régimen, pero pueden promover un ambiente de confianza para fortalecer la lealtad del consumidor hacia la institución.
Palabras Clave: Confianza, seguro de salud, Colombia (fuente: DeCS, BIREME).
Relationships among patients and health care providers may change as national governments and citizens look for the "best" path to an affordable, accountable, and competitive healthcare system. This transition may obviously raise concerns and may even generate mistrust among customers regarding policies and the services provided by healthcare institutions (1). Thus, the purpose of this study is to analyze to what extent a healthcare insurance plan with more or less coverage predicts consumer perceptions of trust in a healthcare institution, and in turn, to what extent trust predicts their level of loyalty towards an institution.
The relationship between insurance coverage, trust, and loyalty can be useful for understanding consumer perceptions about the actual service provided by a healthcare institution. In a broad sense, this study can also provide some hints as to how healthcare policies, in terms of coverage, may be accepted or rejected by individuals once they are implemented. Behind this practical implication, there is now a major ongoing debate as to what extent the healthcare industry should be regulated or to what extent the industry should flow on free market principles. Under the first option, all individuals benefit from a healthcare system that is regulated by the government and supported by citizens' contributions (mainly through taxes). The first option, a regulated system, makes all taxpayers responsible for the cost and restricts the benefits so that the largest number of people who are part of the system are able to benefit. Under the second option, a competitive system, each individual can decide to purchase and benefit from a healthcare insurance package. This competitive scenario provides individuals not only the possibility of choosing, but also the responsibility for their decision.
The Colombian healthcare system has been recognized for offering a combined model that uses market mechanisms to manage health-funding provisions. However, it also recognizes the need to regulate individual memberships and the extent of contributions (2). Hence, in the Colombian healthcare system it is possible to observe three types of insurance policies: namely, pre-paid medical insurance, a mandatory health plan, and a mandatory subsidized health plan. The goal of having this set of policies is to increase the number of citizens who are affiliated and receive healthcare services, while still encouraging competition among organizations that affiliate individuals and provide health services and giving citizens the option of having more control over their health care.
Individuals can decide to acquire a pre-paid medical insurance policy where they are able to select a healthcare provider of their preference; individuals willing to have this type of plan choose to pay a premium price. On the other end, a mandatory subsidized health plan provides health coverage to individuals who do not make a contribution because they are not employed and belong to the lowest income class. The government subsidizes this type of plan. The system also offers an intermediate alternative, a mandatory and contributory healthcare plan, where individuals and their families benefit from a healthcare insurance plan that they pay together with their employers.
In comparative terms, the pre-paid plan is the most competitive scenario where individuals are free to pay for and choose their health care service. The intermediate plan has a lower premium, but individuals do not have the freedom to choose their health care provider. The subsidized plan (a completely regulated scenario) provides basic healthcare coverage at no cost to the patient. These three different scenarios have given rise to a debate that many countries are now facing, acknowledging the need to provide healthcare coverage and at the same time deciding whether this cost should be a responsibility of each individual or of the government through taxpayers (3).
In short, this study uses the case of the Colombian healthcare system that has three kinds of insurance policies. These policies provide patients with more or less control over the coverage and healthcare providers. The experience individuals have with these policies is expected to predict their perception of trust in a health provider organization and, in turn, their loyalty towards such an organization.
Trust and Healthcare Coverage
Trust is a psychological state in which an individual, perceiving some level of vulnerability, while at the same time expecting some future benefits, decides to rely on a person or an organization (4). The perception of trust means that an individual believes there is and accepts some level of vulnerability hoping that another individual has good intentions (5). Consistently, trust has also been defined though dependability and benevolence (6, 7). Dependability means that a party is considered reliable, and benevolence means that a party is willing to protect the interests and well-being of the other.
Thus, despite the perceived vulnerability and uncertainty, an individual chooses to rely on a relationship. This apparent contradiction is explained as an adaptation process because, by trusting, an individual anticipates there might be a risk, acknowledges what has been learned from previous experiences, and decides to engage in a relationship hoping it will be positive. In fact, even if a problem arises, a trustworthy relationship allows parties to deal with the problem as functional and the relationship may continue (8).
These definitions show the importance of trust for the healthcare industry; trust is the solid link between healthcare providers and patients (9). Although patients feel that the outcome of treatment is uncertain, they trust healthcare providers to be knowledgeable of such treatment and to place a significant effort aiming at the best possible outcome. Therefore, the patient's perception of trust may depend on the experience they have had with other healthcare providers. However, the service provided by a health institution differs depending on the type of healthcare coverage an individual has. Individuals who pay an extra premium for an insurance policy have the freedom to choose their health provider as well as more extended coverage compared to regulated policies. Along these lines, a healthcare policy for which individuals pay a lower premium implies more restrictions on coverage and health providers (contributory plan). Regulated health policies have more restrictions and fewer possibilities to provide extended coverage to all patients (subsidized plan).
H1: Health insurance policies with wider coverage are related to stronger consumer perceptions of trust in a health provider institution such that:
H1a: individuals with a premium health plan have a stronger perception of trust when compared to others.
H1b: Individuals with a contributory health plan have a stronger perception of trust when compared to others.
Loyalty
Loyalty is an expression of customer preference for an organization and a customer's decision to continue as clients in the future. Loyalty is observed through customers' recommendations, positive communication in relation with the organization, and future purchases or revisits (10,11). If customers perceive an organization to be trustworthy, they may consider maintaining a long-term relationship (12). Thus, customers' perceptions of trust lead them to expect to be loyal or remain with an organization through expressions of their positive behavioral intentions (13).
H2: the stronger the perception of trust, the higher the level of loyalty a costumer will hold for a health provider institution.
METHOD
Procedure and Sample
This study surveyed patients from a clinic in Colombia. Individuals were asked to participate voluntarily in the study by responding to a questionnaire while they were in the waiting room. In total, the survey was administered to 950 patients. 11 % [109] of these surveys were unusable, which gives a response rate of 89 % [841 surveys]. The sample consisted of 328 (39 %) men and 513 (61 %) women, with an average age of 31.7 years (SD=15,8). Participants were individuals who were: a. Scheduled for an outpatient consultation (62.5 %; 526); b. Hospitalized but not isolated because of their health condition (14.1 %; 119); c. Undergoing a laboratory test or an imaging examination (6.7 %; 56); or, d. Waiting for a priority consultation (16.6 %; 140). Finally, the sample included patients with three types of healthcare coverage. 2.3 % of the patients [246] had a pre-paid plan, 65.6 % [552] belonged to the contributory system, and 5.1 % [43] belonged to the subsidized system.
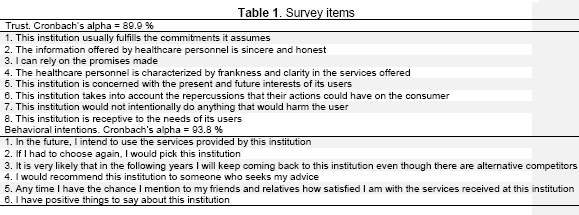
Survey Measures. The questionnaire first asked patients to evaluate their perception of trust for an organization (14,15). This was followed by behavioral intention items evaluating consumer loyalty (Table 1). Finally, the questionnaire inquired about the respondents' demographic information and type of insurance plan.
The dependent variable, namely loyalty, consisted of the two following behavioral intentions: revisit intention and word of mouth. Each of these scales had three items (16). Both trust and loyalty constructs were measured on a five-point Likert scale. The study used two control variables, namely age (measured in number of years) and gender (coded one for males, and zero for females). Finally, healthcare coverage was dummy coded using two variables: Pre-paid medical plan (coded one; zero=o.w.) and Contributory medical plan (coded one; zero, o.w.).
RESULTS
The analysis was run using R (SEM package) and involved performing a structural equation analysis to determine the mediating effect of trust between patients' healthcare plans and their loyalty towards a health institution.
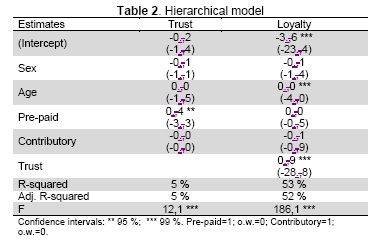
The first model predicts consumer trust in an organization as a function of their healthcare plan, controlling for sex and gender (Table 2).
This trust model shows that having a pre-paid medical plan, instead of another type of plan, positively predicts a greater perception of trust towards a healthcare institution, thus supporting hypothesis 1a. Conversely, the perception of trust of individuals affiliated to a contributory plan is not significantly different from those who hold a subsidized or pre-paid medical plan, failing to support hypothesis 1b. Based on these two results it can be inferred that individuals with a subsidized health plan have a lower perception of trust in health institutions compared to those with a pre-paid plan. Yet, they have a similar perception of trust when compared to those with a contributory plan.
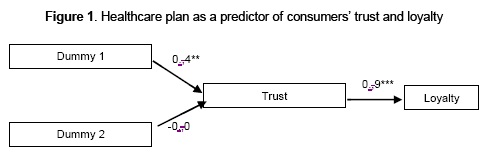
The second model predicts consumers' loyalty as a function of their perception of trust and their type of health plan. This loyalty model indicates a significant increment in R-square (R=53 %). The results yield a significant beta for trust as a predictor of loyalty, thus supporting hypothesis 2. Additionally, after accounting for consumers' perception of trust, the type of healthcare plan an individual has does not have a direct effect on their loyalty to an institution. Consistently, a Sobel test was performed for evaluating whether or not the effect of having a pre-paid medical plan on loyalty significantly decreased after incorporating trust to the model (17). The results of the Sobel test support the mediating effect of trust in that they show that there is a significant path between having a pre-paid medical plan and loyalty, but this relationship becomes not significant after accounting for the mediating effect of trust.
In summary, the results show that, compared to individuals who have regulated healthcare plans (contributory and subsidized), those with a pre-paid medical plan have a greater perception of trust in health provider institutions. Additionally, no relationship is observed between the type of healthcare plan and patients' loyalty towards a health institution. This complete mediation shows that it is their perception of trust what explains patients' loyalty (Figure 1).
DISCUSSION
Countries from around the world are now facing the challenge of finding a more efficient and equitable healthcare system because their population is aging, employers' costs are increasing, and medical equipment and technology are improving. Successfully implementing changes in a healthcare system may depend on creating conditions that enable a high degree of collaboration and trust between healthcare providers and their patients (18). Moreover, since individuals who demand a healthcare service are likely to feel vulnerable, patients' perceptions of trust is a construct that must be assessed, particularly at a time when healthcare institutions are facing day-to-day issues and challenges, just like those who depend on the healthcare system.
Thus, patients may bias their evaluation of healthcare institutions based on their previous experience with and on the characteristics of the healthcare system in their country (19). This may occur not because the institution has some control of the health plans, but because of patients' expectations. Consistently, this study shows that the type of health plan a patient holds explain patients' perception of trust towards a healthcare institution. This finding is analyzed by comparing the three types of health plans offered by the Colombian healthcare system. These plans have three levels of patient responsibility with regard to payment and coverage. A pre-paid medical plan demands more responsibility from consumers, a contributory plan is an intermediate alternative in which individuals pay for health insurance that equals 12 % of their salary, and a subsidized plan does not require any payment from patients, rather services depend on government resources.
Based on these types of healthcare plans, results provide evidence to say that a greater perception of trust is explained by having a plan that provides consumers with more flexibility, allowing them to select their health provider at a premium price. Additionally, individuals who hold either a contributory or a subsidized health plan have a relatively lower perception of trust. However, there is not enough evidence to support the assertion that either of these plans has a negative effect on consumer trust. Additionally, the relationship between the consumers' healthcare plan and their degree of loyalty towards their healthcare institution is completely mediated by their perception of trust towards the institution.
Although health institutions do not control and cannot modify characteristics of the healthcare regimes, these affect consumers' trust of their service. In this sense, previous studies show that institutional and private efforts tend to be a source of trust, whereas government interventions in health issues tend to be a source of mistrust (20, 21). Thus, the healthcare system characteristics and regulations seem to predetermine consumers' expectations, influencing their perception of trust in the service. Health institutions must compensate for the overall perceptual bias by promoting cooperation between patients and health providers. A trustworthy environment will strengthen consumers' loyalty to the institution
This study is based on the Colombian healthcare system, one that has made important efforts in an attempt to provide healthcare coverage to the largest number of citizens while incorporating free market competitive characteristics. However, there are several social and contextual factors that future studies may address that are unique to every country and can influence individuals' evaluation of a health institution or a healthcare system (22). Each government must decide on a proper balance between competitive free-market and regulated plans.*
REFERENCES
1. Marsh RE. The health care industry and its medical care providers: relationship of trust or antitrust? DePaul Business & Commercial Law Journal. 2010; 8(3): 251-73. [ Links ]
2. González-Rossetti A, Ramírez P. Enhancing the political feasibility of health reform: the colombia case. Data for Decision Making project. [Internet]. Available from: https://www.hsph.harvard.edu/ihsg/publications/pdf/lac/Colombiafinal-pp2.PDF. Retrieved april 2015. [ Links ]
3. Heller PS. Who will pay? Washington, D.C.: International Monetary Found; 2003. [ Links ]
4. Kramer RM. Trust and distrust in organizations: emerging perspectives, enduring questions. Annual Review of Psychology. 1999; 50:569-98. [ Links ]
5. Rousseau DM, Sitkin SB, Burt RS, Camerer C. Introduction to special topic forum: not so different after all: a cross-discipline view of trust. The Academy of Management Review. 1998; 23(3):393-404. [ Links ]
6. Doney PM, Cannon JP. An examination of the nature of trust in buyer-seller relationships. The Journal of Marketing. 1997; 61(2):35-51. [ Links ]
7. Hosmer LT. Trust: the connecting link between organizational theory and philosophical ethics. The Academy of Management Review. 1995; 20(2):379-403. [ Links ]
8. Morgan RM, Hunt SD. The commitment-trust theory of relationship marketing. The Journal of Marketing. 1994; 58(3):20-38 [ Links ]
9. Gilson L. Editorial: building trust and value in health systems in low- and middle-income countries. Social Science & Medicine. 2005;61(7):1381-4. [ Links ]
10. Karatepe OM. Customer complaints and organizational responses: the effects of complainants' perceptions of justice on satisfaction and loyalty. International Journal of Hospitality Management. 2006; 25(1):69-90. [ Links ]
11. Zeithaml VA, Berry LL, Parasuraman A. The behavioral consequences of service quality. The Journal of Marketing. 1996; 60(2):31-46. [ Links ]
12. Ganesan S. Determinants of long-term orientation in buyer-seller relationships. The Journal of Marketing. 1994; 58(2):1-19. [ Links ]
13. Garbarino E, Johnson MS. The different roles of satisfaction, trust, and commitment in customer relationships. The Journal of Marketing. 1999; 63(2):70-87. [ Links ]
14. Flavián C, Guinalíu M. Consumer trust, perceived security and privacy policy: Three basic elements of loyalty to a web site. Industrial Management and Data Systems. 2006; 106(5):601-20. [ Links ]
15. Kumar N, Scheer LK, Steenkamp J-BEM. The effects of supplier fairness on vulnerable resellers. Journal of Marketing Research. 1995; 32(1):54-65. [ Links ]
16. Maxham JG, Netemeyer RG. Modeling customer perceptions of complaint handling over time: the effects of perceived justice on satisfaction and intent. Journal of Retailing. 2002; 78(4):239-52. [ Links ]
17. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004; 36:717-31. [ Links ]
18. Davis SB, Robinson PJ. Health Care Providers Under Pressure: Making the Most of Challenging Times. Journal of Health Care Finance. 2010; 37(2):49-55. [ Links ]
19. Mizrahi S, Vigoda-Gadot E, Cohen N. Trust, participation, and performance in public administration: an empirical examination of health services in Israel. Public Performance & Management Review. 2009. 33(1):7-33. [ Links ]
20. Abelson J, Miller FA, Giacomini M. What does it mean to trust a health system?: A qualitative study of Canadian health care values. Health Policy. 2009; 91(1):63-70. [ Links ]
21. Taylor-Gooby P. Trust, risk and health care reform. Health, Risk & Society. 2006; 8(2):97 - 103. [ Links ]
22. Gilson L. Trust and the development of health care as a social institution. Social Science & Medicine. 2003; 56(7):1453-68. [ Links ]