Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista de Salud Pública
Print version ISSN 0124-0064
Rev. salud pública vol.18 no.1 Bogotá Jan./Feb. 2016
https://doi.org/10.15446/rsap.v18n1.45002
Incorporating equity issues into the development of Colombian clinical practice guidelines: suggestions for the GRADE approach
Incorporando equidad al desarrollo de guías de práctica clínicacolombianas: jheslavas@unal.edu.cosugerencias para la aproximación Grade
Javier H. Eslava-Schmalbach1, Vivian A. Welch2, Peter Tugwell2, Ana C. Amaya1, Hernando Gaitán1, Paola Mosquera1, Felipe Molina1, Fernando Peralta1, Sara Romero-Vanegas1, Rodrigo Pardo1 and Juan Pablo Alzate1
1 Universidad Nacional de Colombia, Bogotá, Colombia. jheslavas@unal.edu.co; acamayaa@unal.edu.co; hggaitand@unal.edu.co; paolamosquera@gmail.com; hfmolinal@unal.edu.co; fperaltap@unal.edu.co; sarajromerov@gmail.com; jpalzateg@unal.edu.co; jpalzateg@unal.edu.co
2 University of Ottawa. Ottawa, Canada. jheslavas@unal.edu.co; vivian.welch@uottawa.ca; maria.cannataro@uottawa.ca
Received 16th August 2014/Sent for Modification 10th January 2015/Accepted 8th November 2015
ABSTRACT
Objective To propose how to incorporate equity issues, using the GRADE approach, into the development and implementation of Colombian Clinical Practice Guidelines.
Methodology This proposal was developed in four phases: 1. Included a literature review and the development of a preliminary proposal about how to include equity issues; 2. Involved an informal discussion to reach a consensus on improving the first proposal; 3. Was a survey of the researchers' acceptance levels of the proposal, and; 4. A final informal consensus was formed to adjust the proposal.
Results A proposal on how to incorporate equity issues into the GRADE approach was developed. It places particular emphasis on the recognition of disadvantaged populations in the development and implementation of the suggested guideline. PROGRESS-Plus is recommended for use in exploring the various categories of disadvantaged people. The proposal suggests that evidence be rated differentially by giving higher ratings to studies that consider equity issues than those that do not. The proposal also suggests the inclusion of indicators to monitor the impacts of the implementation of CPGs on disadvantaged people.
Conclusions A consideration of equity in the development and implementation of clinical practice guidelines and quality assessments of the evidence would achieve more in the participation of potential actors in the process and reflect on the effectiveness of the proposed interventions across all social groups.
Key Words: Guideline; healthcare disparities; health care quality, access and evaluation (source: MeSH, NLM).
RESUMEN
Objetivo Proponer como incorporar temas de equidad en el desarrollo e implementación de guías de práctica clínica colombianas utilizando el acercamiento GRADE.
Metodología Esta propuesta fue desarrollada en 4 fases: una revisión de la literatura y desarrollo de una propuesta preliminar sobre como incluir temas de equidad, discusión informal para alcanzar un consenso que mejore la primera propuesta; una encuesta sobre los niveles de aceptación de la propuesta y un consenso informal final para ajustar la propuesta.
Resultados Se desarrolló una propuesta sobre como incorporar temas de equidad con el acercamiento GRADE. Este hace énfasis especial en el reconocimiento de poblaciones en desventaja al desarrollar e implementar guías. Se recomienda el uso del PROGRESS-Plus para explorar las categorías de las poblaciones en desventaja. La propuesta sugiere una calificación diferencial de la evidencia dando clasificaciones superiores a los estudios que toman en consideración temas de equidad. Esta propuesta también sugiere la inclusión de indicadores que monitoreen el impacto de la implementación de GPC en personas en desventaja.
Conclusiones Tener en cuenta la equidad en el desarrollo e implementación de las guías de práctica clínica y la evaluación de calidad de la evidencia puede lograr más en la participación de los actores potenciales del proceso y reflejarse en la efectividad de las intervenciones propuestas en todos los grupos sociales.
Palabras Clave: Guía; disparidades en atención de salud; calidad, acceso y evaluación de la atención de salud (fuente: DeCS, BIREME).
Hitherto, the importance of the use of unified systems for rating the evidence used in systematic reviews and to produce clinical practice guidelines has been suggested (1).
Although the accumulated evidence looks at both the benefits and harm to specific groups of individuals, the expected benefits and harm should be tested at the community level when these findings are used to build CPGs. At this point, equity becomes relevant in ascertaining whether the implementation and effectiveness are going to be as optimal as determined in the initial evaluation.
Braveman (1) defined equity in health as, "...the absence of disparities in health that are systematically associated with social advantage or disadvantage". Whitehead (3) defined health inequity as, "...differences in health which are not only unnecessary and avoidable but, in addition, are considered unfair and unjust". As a challenge associated with social justice, equity goes beyond individual evaluations of interventions. This requires an entirely different perspective, which becomes even more relevant if this evidence is used to develop Clinical Practice Guidelines (CPGs).
While clearly illuminating considerations regarding equity in the evaluation of CPGs, Oxman (4) did not mention the topic of how to deal with them in the development and implementation of those CPGs.
Given these considerations, thought needs to be directed toward how to use this evidence as the foundation for incorporating equity into the development and implementation of clinical practice guidelines. As a system for rating evidence, GRADE has gained increasing international acceptance for qualifying evidence that has either been included, or is going to be included, in systematic reviews or CPGs (5). Consequently, the objective of this paper is to develop a proposal regarding how to incorporate equity issues into the GRADE approach for the development and implementation of new CPGs.
METHODS
This perspective paper was developed in four phases. First, a critical review of the steps involved in the GRADE approach was undertaken; this led to suggestions from several authors about how to incorporate equity issues into the development, implementation, and/or evaluation of CPGs.
Next, an informal consensus was reached on the steps required, using the GRADE approach, for the inclusion of equity considerations into the development and implementation of CPGs (6). This consensus drew on both the critical literature review and the experience of the researchers. Then, a survey was conducted with experts and researchers from around the world to ascertain whether they agreed with the proposal, or not. A final consensus was reached after adjusting one item, which had been the object of disagreement. The selection of the experts and researchers surveyed was performed according to the authors’ convenience.
RESULTS
First approach following the literature review
Although the issue of equity has been discussed by authors for significantly more than 20 years, equity and equity in health have been practically missing from the discussion of how to develop CPGs.
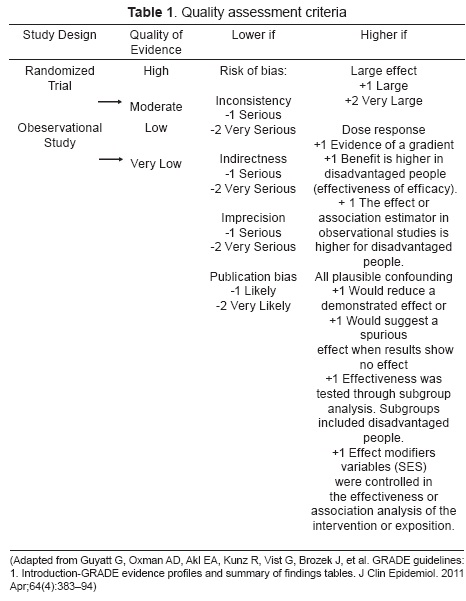
The general rationale of the comparisons in Table 1 is to relate dealing with equity issues to outcomes, values, and/or the preferences of the subjects, and the contexts (4) in which they are living. Differences or disparities in health can be related to basal risks, values, and the preferences of people (7), as well as the social determinants of health (context) (4,8).
In 2003, Aldrich was the first of the authors reviewed to write an approximation that attempted to consider the role of socioeconomic variables in the development of CPGs (8) (Table 1). In 2006, Oxman wrote a series of steps to use in considering equity issues in the development of CPGs. However, these steps were not connected with GRADE steps (4).
In 2007, Dans (9) recommended taking equity issues into account within CPGs; however, they neither provided suggestions about how to deal with these issues nor did they discuss how they affected the strength of the recommendations given in the CPGs. Similarly, Tugwell (7) published a paper focused on the knowledge translation of systematic reviews, which assumed barriers related to limitations in the implementation of their results. They suggested consideration of the modifiable barriers for the 6 P’s (public, patient, practitioner, policy-maker, press, and private sector), according to socioeconomic status in the equity-effectiveness step as well as in the implementation of the systematic review (7). Again, the implications of these evaluations for use in the development of new CPGs were not mentioned (Table 1). However, in 2011, Tugwell and another group developed a series of clinical practice guidelines, to use with refugees and immigrants (10), which included a methodological proposal with several steps that they suggested could be performed (Table 1). Even though these steps can be partially linked within the guidelines with the steps of GRADE, the authors did not specify these links.
Culyers (11) mentions equity issues in the context of health technology assessments. He suggests a series of steps that consider the role of the potential differences, in relationship to technology, among populations that are going to be assessed (Table 1).
The last column of Table 1 illustrates the first approach of how to incorporate and include equity issues into the GRADE steps. This proposal, combined with the literature review, was used to arrive at the informal consensus.
Suggested Steps
Equity considerations in the development of CPGs should be practical for users who want to employ this perspective for a new CPG. As mentioned above, with the explicit intention of addressing and diminishing health disparities in the population, the last column of Table 1 suggests steps to be considered in the development of a new CPG.
Steps 1 through 5 are taken from the preparatory steps proposed by Guyatt (6) in 2011, "Prioritize problems and establish review team and/or guideline panel." This involves learning the priority of the problems that a community has, and subsequently diagnosing the illnesses and disparities that need to be solved.
Steps 6 through 10 were taken from the GRADE steps of, "Defining the question and collecting evidence, rating evidence quality and grading recommendations." A modified summary presentation of the findings and recommendations is then suggested (Table 1). It provides particular relevancy to interventions that have an important role in reducing disparities. The final steps are those proposed by Guyatt.
Results of Informal Consensus
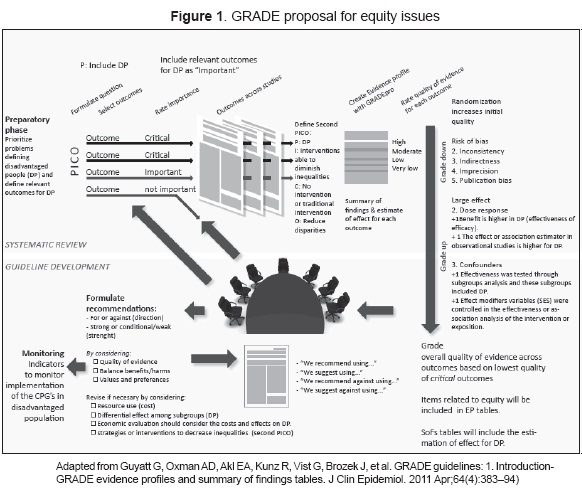
This model below is the result of our informal consensus.
1. Preparatory phase
a. Define disadvantaged people
A baseline quali-quantitative evaluation of existing disparities and inequalities should be done for the specific pathology and health indicators of the guideline. Its implementation should be in consideration of the variables from the context of the population. The first step is to arrive at either a formal or an informal consensus of experts to explore the potential disadvantaged population for the pathology on which the guideline is to focus. The second step is an epidemiologic analysis of inequalities and disparities. For this step, the inequality evaluation guidelines of Kunst and MacKenbach could be used (12) to ascertain the current disparities related to the CPG under development. Health indicators should be analyzed according to subgroups of the disadvantaged populations. The acronym PROGRESS-Plus, which stands for Place of residence (urban/rural), Race/Ethnicity, Occupation, Gender, Religion, Education, Socioeconomic status, Social capital plus Age, Disability and Sexual Orientation, should be considered (Welch, Tugwell (13)).
b. Define relevant outcomes for the disadvantaged population
The selection of health outcomes should be defined based on the quali-quantitative analysis of the inequalities and disparities of disadvantaged people, mentioned above, and the consensus achieved among experts from the health professions, the general community, and disadvantaged people. The relative importance of each outcome should be qualified using the GRADE methodology.
2. GRADE - Step 1: Defining the question and collecting evidence
The disadvantaged population and the outcomes defined in the preparatory phase should be included in the development of PICO questions, which ask about the effectiveness of the intervention under study. Interventions with greater effectiveness within the disadvantaged population or with evidence of effectiveness at reducing gaps among subpopulations should be prioritized.
A logic model, which includes social determinants of health, should be generated to understand the relationships among interventions, outcomes, effect modifiers, and contextual variables (4). Subsequently, search strategies can be performed.
A second PICO question specifically designed to look for interventions within which inequalities can be diminished should also be developed. The outcome of this question will be an inequality, while its intervention will be a public health intervention related to the specific pathology of the CPG. The data derived from this question can then be used to define or adjust recommendations and develop implementation strategies.
3. GRADE - Step 2: Rating the Quality of Evidence
The Cochrane checklist for testing the quality of evidence for an equity issue will be used with the evidence used in the systematic reviews (14).
The GRADE approach, which is modified when selected outcomes are relevant to disadvantaged people, will be used to rate the quality of primary studies. We suggest higher ratings for quality in the equity analysis under the following conditions:
- Effectiveness is tested through the analysis of subgroups, which include disadvantaged people.
- Benefits are higher for disadvantaged people (effectiveness of efficacy).
- The effect or association estimator in observational studies is higher for disadvantaged people.
- Effect modifiers variables (SES) were either controlled for effectiveness, or an association analysis of the intervention, or an exposition was undertaken.
The evidence and profiles of the evidence for each outcome should be summarized. If possible, summaries should include a subgroup analysis and the results of the qualitative/quantitative analysis should be conducted in the preparatory phase.
4. GRADE - Step 3: Recommendations
A comprehensive review of the quality of the evidence should be conducted before suggesting the recommendations. GRADE suggests three criteria for defining the strength and direction of recommendations: the quality of the evidence, the balance between desirable and undesirable outcomes, and the values and preferences of the patients. This consensus suggests including an evaluation of the impact of the intervention under the study on health inequalities. The differential effects among the subgroups of each of the categories suggested by GRADE should be considered. The recommendations generated from the answers to the second PICO question regarding measures for reducing inequalities and inequities should be considered. The results obtained from the second PICO question, investigating strategies or interventions to decrease inequalities, should also be considered in this step.
Economic evaluations should consider the costs and effects on disadvantaged populations while the models should include the subgroups of these populations. Although this type of analysis may increase the final effectiveness of the intervention, it will probably increase the costs associated with the strategy of focusing the intervention on a disadvantaged population.
5. Monitoring
Indicators for monitoring the implementation of the CPGs in disadvantaged populations should be stated and linked to strategies to follow-up and periodically test the impacts on the subgroups. An inequality/disparity analysis that variously uses either simple or complex methodologies, depending on the case, is recommended.
DISCUSSION
The clinical practice guidelines are an important tool in ensuring equity in health care, correlating with the needs in specific populations, seeking to improve the quality of care, and making health decisions. This can subsequently result in equal attention to both access and quality, and helping to eliminate and/or reduce avoidable or unfair factors.
Health equity has become an important issue that involves the consideration of many factors, including, among other, the delivery of health services, access to those services, and social participation.
WHO has embraced the elimination of health inequities as an important target and supports the dual goals of equity and efficiency for health services (4).
Clinical practical guidelines have clearly been promoted as tools to help improve the quality of the care provided (5,10). A combination of clinical practice guidelines and interventions, which can potentially reduce disparities, could be a phenomenal tool for policy makers who are interested in reducing health disparities in a given population. Incorporating equity issues into the developmental steps of CPGs will facilitate policy makers and researchers in taking the state of health disparities of any population into consideration where those CPGs are going to be included in the health system.
Therefore, we can conclude that a consideration of equity in the development and implementation of clinical practice guidelines and quality assessments of the evidence would achieve more in the participation of potential actors in the process and reflect on the effectiveness of the proposed interventions across all social groups. This would subsequently indicate that group differences must be considered for each social category, whether in diagnosis, monitoring, treatment, coverage, or adherence to patients, when the efficacy of a guide to clinical practice in specific communities can be evaluated. It is important to consider how best to support both the identification of/and the addressing of the needs for organizational changes in the development, implementation, and evaluation of clinical practice guidelines. In countries where inequalities are large, initial institutional, cultural, and political change may all be necessary.
Appropriate indicators that demonstrate the social and economic status of population groups should be developed. In addition, the impact of the guidelines on health inequities detected in developing the guide should also be used to monitor the effects of the implementation of the recommendations on disadvantaged populations •
REFERENCES
1. Shepperd S, Straus S. GRADE: complex decisions. J Clin Epidemiol. [Editorial Introductory]. 2011 Dec;64(12):1270-1. [ Links ]
2. Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health. [Review]. 2003 Apr;57(4):254-8. [ Links ]
3. Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429-45. [ Links ]
4. Oxman AD, Schunemann HJ, Fretheim A. Improving the use of research evidence in guideline development: 12. Incorporating considerations of equity. Health Res Policy Syst. 2006;4:24. [ Links ]
5. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. [Research Support, Non-U.S. Gov't]. 2004 Jun 19;328(7454):1490. [ Links ]
6. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011 Apr;64(4):383-94. [ Links ]
7. Tugwell P, Robinson V, Grimshaw J, Santesso N. Systematic reviews and knowledge translation. Bull World Health Organ. [Research Support, Non-U.S. Gov't]. 2006 Aug;84(8):643-51. [ Links ]
8. Aldrich R, Kemp L, Williams JS, Harris E, Simpson S, Wilson A, et al. Using socioeconomic evidence in clinical practice guidelines. BMJ. [Review]. 2003 Nov 29;327(7426):1283-5. [ Links ]
9. Dans AM, Dans L, Oxman AD, Robinson VZz, Acuin J, Tugwell P, et al. Assessing equity in clinical practice guidelines. J Clin Epidemiol. 2007 Jun;60(6):540-6. [ Links ]
10. Tugwell P, Pottie K, Welch V, Ueffing E, Chambers A, Feightner J. Evaluation of evidence-based literature and formulation of recommendations for the clinical preventive guidelines for immigrants and refugees in Canada. CMAJ. 2011 Sept 6;183(12):E933-E8. [ Links ]
11. Culyer AJ, Bombard Y. Equity in Health Technology Appraisal. In Press. 2012. [ Links ]
12. Kunst AE, MacKenbach JP. Measuring socioeconomic inequalities in health. Copenhagen: WHO Regional Office for Europe; 1994. [ Links ]
13. Welch V, Tugwell P, Petticrew M, de Montigny J, Ueffing E, Kristjansson B, et al. How effects on health equity are assessed in systematic reviews of interventions. Cochrane Database of Systematic Reviews [internet]. 2010; (12): Available from: http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/MR000028/frame.html. Consultado enero 2015. [ Links ]
14. Ueffing E, Tugwell P, Welch V, Petticrew M, Kristjansson E for the Campbelland Cochrane Equity Methods Group. [internet]. Equity Checklist for Systematic Review Authors 2011: Available from: http://equity.cochrane.org/sites/equity.cochrane.org/files/uploads/equitychecklist2011.pdf. Consultado enero 2015. [ Links ]