Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista de Salud Pública
versão impressa ISSN 0124-0064
Rev. salud pública vol.18 no.3 Bogotá maio/jun. 2016
https://doi.org/10.15446/rsap.v18n3.44487
Doi: http://dx.doi.org/10.15446/rsap.v18n3.44487
Artículos Investigación
Knowledge, attitudes and practices of prevention for cervical cancer and breast cancer among medical students
Encuesta CAP a estudiantes de medicina para prevención del cáncer de mama y cuello uterino
Pablo Rodríguez-Feria, Luis J. Hernández-Flórez y Daniela Rodríguez-Feria
Deparment of Public Health. Universidad de los Andes, Bogotá, Colombia. pa.rodriguez48@uniandes.edu.co; luishern@uniandes.edu.co; d.rodriguez892@uniandes.edu.co
Recibido 18 Julio 2014/Enviado para Modificación 6 Diciembre 2014/Aceptado 13 Septiembre 2015
ABSTRACT
Objective To assess the knowledge, attitudes and practices of medical students for health promotion, primary prevention and early detection of breast neoplasm and uterine cervical neoplasm, as well as to make recommendations for improving the Public Health curriculum at the Universidad de los Andes.
Methodology This study utilized a survey of medical knowledge, attitudes and practices applied to fifth year Colombian medical students attending the Universidad de los Andes in the first semester of 2013.
Results 64/76 students answered the surveys (response rate 84.2 % ): 62.5 % (40/64) and 37.5 % (24/64) response rates from students in their ninth and tenth semesters, respectively; and 64.1 % (41/64) and 35.9 % (23/64) response rates from female and male students, respectively. Knowledge: clinical breast exam (CBE), breast self-examination (BSE) and mammography were recommended by 95.3 % (61/64) of students, 96.9 % (62/64) of medical students and 90.7 % (58/64) of students, respectively. Attitude: the most effective tests to reduce mortality in women aged ≥ 50 years were the Papanicolaou test according to 90.6 % (58/64) of students and mammography according to 82.8 % (53/64) of students. Practice: 55.0 % (35/64) of students had received training in the guidelines and protocols for breast neoplasm and uterine cervical neoplasm screening.
Discussion To promote early detection of cervical and breast cancer, knowledge, attitudes and practices must be improved to enhance clinical practices (e.g. Papanicolaou test) and medical student training guidelines or protocols for these two cancers. Overall, with induced demand and support from research communities and institutions seeking to make these improvements, we collaborate to decrease missed opportunities in medical research and Public Health.
Key Words: Breast neoplasms, uterine cervical neoplasms, public health, education, medical, curriculum, students, medical (source: MeSH. NLM).
RESUMEN
Objetivo Evaluar el conocimiento, actitudes y prácticas (CAP) de los estudiantes de medicina para prevención de neoplasia de la mama y neoplasia del cuello uterino, así mismo el estudio proveerá recomendaciones para mejorar el currículo de las clases de salud pública.
Metodología El estudio empleo una encuesta CAP aplicada a estudiantes de quinto año de medicina de la Universidad de los Andes en el primer semestre del año 2013.
Resultados Del total de 76 estudiantes 64 contestaron la encuesta. Estudiantes de noveno semestre 62.5 % (40/64) y de decimo semestre 37.5 % (24/64). Género: Femenino 64,1 % (41/64) y masculino 35,9 % (23/64). Conocimiento: El examen clínico de seno fue recomendado por los estudiantes un 95,3 % (61/64), el auto examen de seno 96.9 % (62/64) y la mamografía 90.7 % (58/64). Actitudes: Los exámenes más efectivos para reducir la mortalidad en mujeres ≥ 50 años fueron la prueba de Papanicolaou 90,6 % (58/64) y la mamografía 82,8 % (53/64). Practica: 55,0 % (35/64) de los estudiantes han recibido entrenamiento en guías de manejo o protocolos para el tamizaje de neoplasia de seno y neoplasia de cuello uterino.
Discusión Con el fin de realizar detección temprana en cáncer se deben mejorar las destrezas, el conocimiento y el entrenamiento ¿en cuanto a demanda inducida, búsqueda activa tanto comunitaria como institucional y disminución de oportunidades perdidas relacionadas con Salud Publica. Adicionalmente, es importante mejorar la práctica clínica relacionada con el examen de Papanicolaou y entrenamiento sobre guías clínicas y protocolos para estos tipos de cáncer.
Palabras Clave: Neoplasia del cuello uterino, neoplasia de la mama, salud pública, educación médica, estudiantes de medicina, curriculum (fuente: DeCS. BIREME).
The knowledge, attitudes and practices (KAP) survey is a tool used to appraise the competence of a population of students or health workers for a particular theme. The tool focuses on the subjects' knowledge, attitudes and level of practical experience (1). First, it serves to implement and evaluate the mobilization of knowledge of the practices of medical students for a topic. Additionally, KAP survey identifies gaps in knowledge, which facilitates educational processes (2,3). Even though there is currently a paucity of studies in the literature which assess health care workers' KAP for the prevention and early diagnosis of cancer, existing studies have yielded important results.
In the United States (US), an assessment was conducted in 2012 on the curriculum of a medical school for prevention and detection of cancer. Using a KAP survey, specific interventions were developed to improve the knowledge and attitudes of students. Prior to the curriculum change in 1996, of 114 students surveyed in their fourth year, 70.2 % had observed a Pap smear, 81.6 % had been trained to do it and 88.6 % had performed it. Four years after the curriculum change, of 94 students surveyed in their fourth year, 71.4 % had observed a Pap test, 69.0 % had been trained to perform one and 78.6 % had actually performed the test (4).
A study conducted in Uganda also used the KAP in 2006 to assess the competence of 63 medical students on the topic of screening for uterine cervical neoplasm. The study showed that, despite knowledge of the importance of prevention of cervical cancer, the students' practical experience was limited, with only 13.0 % having performed a Pap test (5).
A KAP survey was also used to appraise fourth and fifth year Pakistani medical students (n=50) regarding screening techniques for breast cancer in 2008; it was found that 80.0 % and 70.0 %, respectively, were aware that mammography and BSE were important screening tests for this disease (6).
In 2009, a study was conducted in Colombia which examined the knowledge and attitudes of general practitioners regarding the Human Papilloma Virus (HPV) vaccine. The results showed that physicians had doubts about the age of vaccination, protection against virus types and the characteristics of the vaccine. It was concluded that extensive training and education was needed regarding HPV and its vaccine (7).
In 2009, a KAP survey was focused on breast cancer screening in 393 health care workers (including 102 doctors) in Nigeria. It was found that 80.7 % of all subjects knew that mammography was useful in the diagnosis of this cancer, however only 23.7 % were aware that this technique is vital in screening for this condition. It was also shown that 45.7 % considered CBE and BSE to be important in screening for breast malignancy (8).
A 2010 study conducted in Mexico looked at the knowledge of cancer screening procedures of 285 medical students and 156 residents. The question "Should a Pap smear be recommended in a woman with a total hysterectomy for a nonmalignant cause?" was correctly answered by 39.5 % of the students. Ultimately it was found that 69.2 % of the students were aware of the correct screening procedure for breast cancer and 70.4 % for cervical cancer (9).
In a survey conducted on 140 Malaysian medical students in 2012, it was shown that 62.9 % had a high level of knowledge about HPV infection, cervical cancer and HPV vaccination (10).
In 2006, another study was conducted to determine the success of a new curriculum for the knowledge of cancer prevention and detection in three US medical schools. The authors' goal was to evaluate if students had observed a doctor performing a Pap test. Pre-test results from the three medical schools showed 112 students (4.5 % ), 75 students (14.7 % ) and 108 students (38.0 % ) had observed the performance of the test. Post-test outcomes for the same situation were 144 students (100 % ), 123 students (92.0 % ) and 182 students (98.3 % ) with a p of value 0.401. In the same way, the authors evaluated how many students were trained to perform a Pap test. The pre-test results were 0.9 %, 6.7 % and 9.2 % in the same pre-test groups while the post-test outcomes were 100 %, 100 % and 98.9 % in the same post-test population (11). The same survey from this study was used again in the US (12) for family medicine/general practitioners, internal medicine specialists and obstetrician/gynecologists. Family medicine/general practitioners (n=502) answered the questionnaire, showing that 94.6 % of doctors recommended mammography in women ages 40 to 49, of which 69.5 % recommended the test on an annual basis, and 99.5 % of physicians suggested the same test in patients aged ≥ 50 every year. Furthermore, 96.5 % of doctors proposed CBE in the first age group once a year (94.7 % ) and 98.1 % recommended it in the second age group every month (96.0 % ). BSE was suggested by 91.6 %, every day of the year (98.6 % ) and 92.5 % in the second group once in a year (93.2 % ).
The incidence of cancer in Colombia over the years 2000-2006 was 70 887 per year, 38 571 of which occurred in women; the most common locations were the breast and cervix (13). Additionally, the average number of deaths due to cancer in Colombia was 32 000 per year in the period between 1984 -2008; the common sites were breast (12.3 % ) and cervix (12.1 % ) (14).
The global record of World Health Organization cancer (GLOBOCAN 2008) showed that, in Colombia, the prevalence of cancer in women over the last 5 years was 79 973 cases (15). Breast cancer was the most prevalent, accounting for around 30.0 % of these, or 24 012 cases. This was followed by cervical cancer with 15 347 cases corresponding to 19.2 % of the total. Breast and cervical cancer were also shown to be the cancers with the highest incidence, with age standardized ratios (ASR) of 31.2/100 000 and 21.5/100 000, respectively.
The Pan American Health Organization considers that many of these lives could be saved by carrying out screening strategies to ensure early diagnosis of breast and cervical cancers (16).
As previously mentioned, this article aims to assess the KAP of medical students in the fields of health promotion, primary prevention and early diagnosis for the two most prevalent cancers with the highest incidence and mortality in Colombian women. The study will also make recommendations to enhance the curriculum by filling gaps and reducing weak points.
MATERIALS AND METHODS
The current study utilized a KAP survey conducted on fifth year medical students on the topic of screening for breast and uterine cervical neoplasms.
To begin, researchers modified the national survey of primary care physicians' cancer screening recommendations and practices for breast and cervical cancer sponsored by the US National Cancer Institute in collaboration with the Agency for Healthcare Research and Quality and Center for Disease Control and Prevention (17).
All questions were translated into Spanish, 10 of these were subsequently chosen and 8 more were added. Afterward, a pilot study was done of the 18 questions on a sample of 20 students in their ninth and tenth semester. Following this pilot study, 2 questions were removed as they were poorly understood or did not fit the knowledge base of general practitioners. This allowed validation of the terminology and definitions used in the study.
The population studied included fifth year medical students attending the Universidad de los Andes, who were undertaking Public Health or Gynecology classes or had undertaken these classes in the past. In 2013, between January and June, there were 36 students from their ninth semester and 40 from their tenth semester.
The questionnaire was completed in April 2013 after verbal consent was obtained and the reasons for the study were explained to the participants. Information processing was done in Excel. Questions [1-3] were regarding demographics, [7, 8, 11, 12, 14-16] assessed knowledge, [4 and 9] concerned attitudes and [5, 6, 9, 10 and 13] focused on practical experience.
RESULTS
The survey was answered by 64 students (84.2 % ), 40 of whom were in their ninth semester of medical school (62.5 % ) and the remaining 24 were in their tenth semester (37.5 % ). The gender distribution was 41 female (64.1 % ) and 23 male (35.9 % ).
Knowledge
a. Student recommendations for breast cancer screening in asymptomatic women aged 40 to 49.
57 participants recommended CBE on an annual basis (54.4 % ), 62 students urged BSE every month (54.4 % ), 49 respondents proposed annual mammography (69.4 % ).
b. Tests that students recommended for screening in asymptomatic patients for breast cancer women aged ≥50.
61 medical students proposed CBE every 12 months (45.9 % ), 62 students recommended BSE once a month (41.9 % ), and 58 students suggested mammography on an annual basis (72.4 % ).
c. When did students not recommend screening for breast neoplasm?
18 students did not recommend CBE in patients aged ≥60 (33.3 % ). 17 participants did not propose BSE in women aged ≥ 60 (23.5 % ) and patients aged ≥70 (17.1 % ), while 23 participants did not recommend (35.9 % ) mammography in women aged ≥ 70 (30.4 % ).
d. Tests that students will recommend based on clinical history for screen breast neoplasm.
55/64 (85.9 % ) participants suggested mammography and CBE in healthy women at age 50. 49/64 (76.6 % ) students recommended the same tests in healthy women at age 65. 39/64 (60.9 % ) participants proposed the two exams in healthy women at age 80. 56/64 (87.5 % ) students recommended mammography and CBE in 50 year old women with unresectable non-small cell lung cancer, while 52/64 (81.3 % ) students suggested both tests in 65 year old women with unresectable non-small cell lung cancer.
e. Procedures for inducing demand or active search for breast neoplasm and cervical uterine neoplasm.
For breast cancer, 27 students (42.2 % ) answered that they knew procedures to accomplish this target, 33 students (51.6 % ) responded they did not know any procedures to achieve this goal, and 4 students (6.3 % ) were not sure if their answers would induce demand or active search. In the same way, for cervical cancer, 25 students (39.1 % ) knew how to induce demand or active search for this disease; in contrast, 35 participants (54.7 % ) did not know how to meet this task and 4 students (6.3 % ) were not sure about their answers.
f. Strategies which students used to reduce lost screening opportunities.
33 students (51.6 % ) did not know any actions to accomplish this goal, 13 students (20.3 % ) performed health brigades, 8 participants (12.5 % ) did university campaigns, 5 students (7.8 % ) made brochures and web pages, 3 students (4.7 % ) did surveys and 2 doctors in training (3.1 % ) sent emails.
g. When would students recommend a Pap smear test based on a clinical history?
For an 18-year-old who has never had sexual intercourse and presented for her first gynecologic visit, 19 students (29.7 % ) recommended the exam. Second, for an 18-year-old who had sexual intercourse for the first time 1 month ago and was going for her first gynecologic visit, 49 physicians in training (76.6 % ) recommended it. Third, for an 18-year-old who first had sexual intercourse 3 years ago and was going for her first gynecologic visit, 63 students (98.4 % ) would perform a Pap smear test. Fourth, for a 35-year-old with no new sexual partners within the last 5 years and 3 consecutive negative Pap smear tests performed by the same doctor, 62 participants (96.9 % ) recommended it. Fifth, for a 35-year-old whose cervix was removed last year during a hysterectomy for symptomatic fibroids, who also had no history of cervical, vaginal, or vulvar dysplasia, and 3 consecutive negative Pap smear tests performed by the same physician, 44 students (68.8 % ) suggested it. Finally, for a healthy 66-year-old who has had no new sexual partners in the last 5 years and 3 consecutive negative Pap smear tests performed by the same physician, 44 students (68.8 % ) recommended it.
h. Correlation of HPV vaccine with their respective serotypes.
46 students (71.9 % ) correlated Gardasil® with HPV serotypes 6, 10, 16 and 18, and the same students matched Cervarix® with HPV types 16 and 18.
i. Student recommendations for the HPV vaccine depending on age or intercourse.
23 students (35.9 % ) recommended the HPV vaccine for ≥9 year old patients, and 11 physicians in training (17.2 % ) would recommend it before patients started having sexual intercourse.
Attitudes
j. What are students' beliefs regarding the efficacy of screening procedures for reducing cancer mortality in average-risk women?
First, 39 students (60.9 % ) thought that CBE performed by practitioners was very effective. Second, 31 physicians in training (48.4 % ) considered that BSE was very effective. Third, 48 students (75.0 % ) believed that screen-film mammography for women 40-49 years was very effective. Fourth, 53 physicians in training (82.8 % ) believed that screen-film mammography for women aged ≥50 was very effective. Fifth, 30 students (46.9 % ) had the idea that digital mammography was very effective. Sixth, 48 students (75.0 % ) thought that the Pap smear test (conventional cytology) was very effective. Finally, 58 students (90.6 % ) affirmed that the Pap test (liquid based cytology) was very effective.
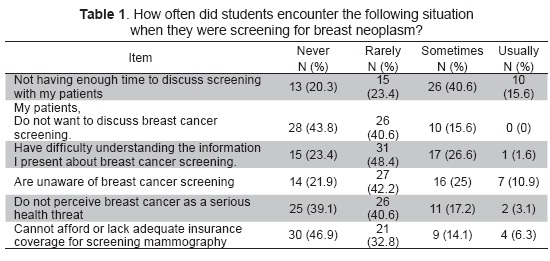
k. How often did students encounter the following situation when they were screening for breast neoplasms with patients?
First, 26 students (40.6 % ) answered that sometimes they did not have enough time to discuss screening with their patients. Second, 28 physicians in training (43.8 % ) remarked that their patients never want to discuss breast cancer screening. Third, 31 participants (48.4 % ) responded that rarely their patients had difficulties understanding the information that they presented about breast cancer screening. Fourth, 27 students (42.2 % ) answered that rarely their patients were unaware of breast cancer screening. Fifth, 26 students (40.6 % ) responded that rarely their patients did not perceive breast cancer as a serious health threat. Finally, 30 students (46.9 % ) answered that their patients could not afford or lacked adequate insurance coverage for screening mammography (Table 1).
Practice
l. Availability of clinical screening guidelines or protocols
Clinical guidelines and protocols for the screening of cervical cancer were more available than those of breast cancer screening, with totals indicating that 57 students (89.1 % ) and 38 doctors in training (59.4 % ), respectively, had available guidelines and protocols.
m. Clinical practice of the Pap smear
10 students (15.6 % ) indicated that they had ordered a Pap smear, 28 students (43.8 % ) had performed this test, while 40 students (62.5 % ) had worked with a person who ordered or performed this test. Only 3 students (4.7 % ) had not ordered it.
n. Training in handling guidelines and protocols for breast cancer or cervical cancer. 35 students (54.7 % ) answered that they received training guidelines and protocols for breast cancer or cervical cancer in clinical practice.
More tables are available at the following link: https://docs.google.com/document/d/1CkB5yHyWlNF5WWpxbtuboSmMauh4RlmeCaI1cbKuDGg/pub, so that readers can explore more information about this research.
DISCUSSION
Studies using KAP surveys for breast neoplasm and cervical uterine neoplasm in health care workers and medical students are sparse in the international literature. Some of the studies available internationally included those conducted by Kumar et al. and Akhigbe AO. Studies conducted in the US include Meissner HI et al. and the Latin-American study written by Villarreal-Garza et al. In addition, a study was conducted by Piñeros et al. in Colombia.
Compared to the study by Kumar et al., the current study found a better understanding of the usefulness of screening for BSE, with a result of 96.9 % compared to 70.0 % in the study by Kumar et al. (6).
Analyzing the results of the Akhigbe AO et al. study (Nigeria, 2009) on health care workers (including 102 physicians (26.0 % ), results indicating the recommendation of BSE and CBE as a screening method were higher in the our study for BSE (96. 9 % vs. 45.8 % ) and CBE (89.1 % vs. 45.8 % )(8).
Examining the outcomes of the current study for breast cancer screening in asymptomatic patients, it shows similar results to the study conducted by Meissner in the US (12). In the current study, 89.1 % of students recommended CBE in women ages 40-49 and 95.3 % recommended this test for women aged ≥50. In the study by Meissner, CBE was suggested in a similar percentage for general practitioners/ family medicine with 96.5 % and 98.1 % of participants recommending the test in women aged 40-49 and ≥50, respectively. In the current study, BSE was recommended in 91.6 % and 92.5 % of women in these two age groups compared with 96.9 % and 96.9 % in the Meissner study (12). The similarities seen between these results may be explained by the fact that the Colombian university where the study was conducted adopts an American curriculum and the majority of students read American Journals.
Comparing the results for mammography as a screening test in the present study, the Kumar et al. (6) study, which did not differentiate the recommendation for this test depending on age, had an outcome of 80 % of medical students suggesting it, while in our study, the percentage of recommendation was higher in women ≥50 years than women ages 40 to 49 (76.6 % vs. 90.6 % ). It should be noted that the Kumar et al. study did not mention the semester of medical students. This could affect the comparability of the studies if less advanced students are being compared with more advanced ones.
Evaluating the current study with research done by Akhigbe et al. (8), 86.7 % of the participants recommended mammography, whereas in the present research, the recommendation changed based on the age of the patient, with 76.6 % indicating the recommendation for women aged 40-49 and 90.6 % recommending mammography for women aged ≥50.
It is important to analyze that in the three last studies (6, 8 and our study), mammography was a pillar for screening this pathology around the world, with a grade of recommendation greater than or equal to 80 % .
Contrasting the data obtained in the current investigation with that conducted by Meissner HI (12); there was a difference in the percentage of participants who recommended mammography in women aged 40-49 in students and general practitioners/family medicine (76.6 % vs. 89.1 % ). On the other hand, the results in students and general practitioners/family medicine physicians were similar when considering women aged ≥50, with 90.6 % and 95.3 % respectively, recommending mammography for women in this age group (12). Interestingly, in the two previous studies, recommendations of the CBE, BSE and mammography were higher in women ≥50 than women ages 40 to 49.
The results of the present study showed that students had little practice in observing and performing Pap smear tests. This same issue was noted in the studies by Mutyaba et al., and Lee (5,11).
Comparing the results of the current study with that of Geller et al., there was little difference in the percentage of students who had observed the performance of the Pap test; outcomes were 62.5 % in the present study vs 61.6 % in the US research. In contrast, the percentage of students who had actually performed a Pap was considerably lower in the current study (43.8 % vs. 77.7 % ) (4).
Both the present study and the study by Villarreal-Garza C et al. (9) questioned whether a Pap smear test would be recommended in a woman with a total hysterectomy fora non malignant cause (18,19). In both studies, the knowledge of participants in this topic was poor, with only 31.3 % and 39.5 % of participants answering correctly in the present study and the Mexican study, respectively (9).
At a national level, comparing the present study with Piñeros et al. (7), both highlight the need to improve training and education for medical students and general practitioners in the field of HPV vaccination.
Considering the above findings, the following recommendations can be made in the medical curriculum: For early detection of cancer, one should improve knowledge, attitudes and practices of medical students and physicians in order to induce: 1. Demand, and; 2. Active community and institutional seeking of preventive screening methods to decrease missed opportunities for screening. Additionally, it is necessary to address questions about the utility of screening methods in clinical practice and how these activities should be carried out. For example, it is paramount to improve clinical practice related to the Pap test and related medical training guidelines and protocols for breast and cervical cancers. The indications for administering the HPV vaccine should also be strengthened. Overall, it is also vital to include interventions of health promotion, primary prevention, and early diagnosis and treatment for both breast and cervical cancers in medical school curriculums 
Contributor ship: Pablo Rodríguez-Feria (PRF) and Daniela Rodríguez-Feria (DRF) led the data gathering, drafted the manuscript, and setup the Excel tool, under the supervision of Luis J. Hernández-Flórez (LJHF) who edited the manuscript.
Acknowledgments: We want to acknowledge Bridget Lee, B.Sc. MPH for her support and participation in this study.
REFERENCES
1. Vandamme E. Concepts and challenges in the use of knowledge-attitude-practice surveys: Literature review. Department of Animal Health. Institute of Tropical Medicine. 2009; 1: 1-7. [ Links ]
2. Organization WH [editorial]. Advocacy, communication and social mobilization for TB control: a guide to developing knowledge, attitude and practice surveys. 2008; 46:1-68. [ Links ]
3. Launiala A. How much can a KAP survey tell us about people's knowledge, attitudes and practices? Some observations from medical anthropology research on malaria inpregnancy in Malawi. Anthropology Matters Journal. 2009; 11:1-13. [ Links ]
4. Geller AC, Prout MN, Miller DR, Siegel B, Sun T, Ockene J, et al. Evaluation of a cancer prevention and detection curriculum for medical students. Prev Med. 2002;35(1):78-86. [ Links ]
5. Mutyaba T, Mmiro FA, Weiderpass E. Knowledge, attitudes and practices on cervical cancer screening among the medical workers of Mulago Hospital, Uganda, BMC Med Educ. 2006; 6:13. [ Links ]
6. Kumar S, Imam AM, Manzoor NF, Masood N. Knowledge, attitude and preventive practices for breast cancer among health care professionals at Aga Khan Hospital Karachi. J Pak Med Assoc. 2009;59(7):474-8. [ Links ]
7. Piñeros MCC, Trujillo L, Wiesner C. Conocimientos, aceptabilidad y actitudes sobre la vacuna contra el VPH en médicos generales, ginecólogos y pediatras en Colombia. Revista Colombia de Cancerologia. 2009; 13(2):88-98. [ Links ]
8. Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9:203. [ Links ]
9. Villarreal-Garza C, García-Aceituno L, Villa AR, Perfecto-Arroyo M, Rojas-Flores M, León-Rodríguez E. Knowledge about cancer screening among medical students and internal medicine residents in Mexico City. J Cancer Educ. 2010;25(4):624-31. [ Links ]
10. Rashwan HH, Saat NZ, Abd Manan DN. Knowledge, attitude and practice of malaysian medical and pharmacy students towards human papillomavirus vaccination. Asian Pac J Cancer Prev. 2012;13(5):2279-83. [ Links ]
11. Lee M, Wilkereson L, Harrity S, Hodgson CS. Differences in cancer prevention knowledge and experience among medical students at three institutions over time. J Cancer Educ. 2006;21(4):223-9. [ Links ]
12. Meissner HI, Klabunde CN, Han PK, Benard VB, Breen N. Breast cancer screening beliefs, recommendations and practices: primary care physicians in the United States. Cancer. 2011;117(14):3101-11. [ Links ]
13. Plan Decenal para el Control del Cáncer en Colombia, 2012-2021 [Internet]. Available in: https://www.minsalud.gov.co/Documentos%20y%20Publicaciones/Plan%20Decenal%20para%20el%20Control%20del%20C % C3 % A1ncer.pdf. Accessed January 2016. [ Links ]
14. Piñeros M, Gamboa O, Hernández-Suárez G, Pardo C, Bray F. Patterns and trends in cancer mortality in Colombia 1984-2008. Cancer Epidemiol. 2013;37(3):233-9. [ Links ]
15. Ferlay J SH, Bray F, Forman D, Mathers C and Parkin DM. Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10 In. Lyon, France: International Agency for Research on Cancer; 2010. [ Links ]
16. Iniciativa del cáncer en la mujer: Un compromiso de todos para salvar vidas [Internet]. Available in: http://www.paho.org/panamericanforum/wp-content/uploads/2013/02/Nota-conceptual-PAFNCD-cancerenlamujer.pdf. Accessed january 2016. [ Links ]
17. National survey of primary care physicians´ cancer screening recommendations and practices. Breast and cervical cancer screening questionnaire [Internet]. Available in: http://healthcaredelivery.cancer.gov/screening_rp/screening_rp_breast_cervical_inst.pdf. Accessed January 2016. [ Links ]
18. The American Congress of Obstetricians and Gynecologists [editorial]. Practice Bulletin Number 131: Screening for cervical cancer. Obstet Gynecol. 2012;120(5):1222-38. [ Links ]
19. Karjane N, Chelmow D. New cervical cancer screening guidelines, again. Obstet Gynecol Clin North Am. 2013;40(2):211-23. [ Links ]