Diabetes mellitus has been a public health problem for decades due to its magnitude and transcendence 1,2. In Mexico, in 2002, there were 5 million diabetic patients and estimations are there will be 15 million by 2025. At least 90% of all diabetic patients suffer from type 2 diabetes 3, which is why it requires a comprehensive management that involves clinical, social and psychological aspects. To this end, the clinical competence of family physicians for the nutritional management of the condition is highly relevant as it will help guide patients to gaining knowledge on their illness and the way it should be taken care of.
Health services seldom estimate the abilities of family physicians to identify patient's nutritional habits and to direct the nutritional management of diabetes mellitus type 2; in this context, abilities are defined as "clinical aptitude" or "clinical competence" 4. Said clinical aptitude or competence consists in seeking the best nutritional care for the patient with diabetes mellitus, in order to generate formative processes directed to create knowledge based on their own experience.
According to some authors, family physicians should recognize the potential difficulties of type 2 diabetic patients regarding diet and therapeutic compliance, as well as facilitate the tasks of patients and their relatives throughout the entire treatment to establish a normal flow of their metabolic control 5-7.
Viniegra 8,9 studied physicians' competence and performance in primary health care. The goal was to evaluate the clinical practice of family physicians when addressing diabetes mellitus type 2. From an integrative perspective, identifying the nutritional management of diabetic patients by family physicians requires being able to recognize research indicators, which will be explained later, and being able to interpret and provide guidance on factors and conditions related with nutritional compliance 10-12.
The objective of this study was to evaluate the effect of a participative educational intervention on the clinical competence of Mexican family physicians for nutritional management of patients with diabetes mellitus type 2. This is the first attempt to counterbalance the shortage of nutrition professionals in primary health care units of social security institutions in Mexico.
MATERIALS AND METHODS
Design, setting and temporality
A "before and after with control group" quasi-experimental study was conducted in two medical units selected randomly at the Instituto Mexicano del Seguro Social, in the Guadalajara Metropolitan Area, Jalisco, Mexico, from January to October 2010. The units were located in different municipalities from the area to control the possible contamination of groups. These medical units were similar in number of physicians affiliated, attended population volume and availability of support services such as laboratory tests, X-rays, electrocardiography, among others.
Universe, sample and sampling
The universe was made up of 60 family physicians affiliated to the medical units, 30 in the medical unit "A" and 30 in the medical unit "B". The study was conducted in a sample for convenience that included all family physicians affiliated to the medical units selected and met the selection criteria defined for this research. Randomly, the medical unit "A" was assigned as control group, and the medical unit "B" as intervention group.
Selection criteria
The participants included were affiliated family physicians, of any age and sex, working for the medical units selected, with different levels of seniority and with or without postgraduate studies, who agreed to participate in the research, provided their informed consent, completely answered the instruments and assisted to at least 80% of the sessions of the course (intervention group).
Variables and instruments
The independent variable was the participative educational intervention, and the dependent variable was the clinical competence of family physicians for the nutritional management of patients with diabetes mellitus type 2. Clinical competence was measured using an instrument designed and validated ex professo, which consists of 100 true, false and don't know questions, based on real clinical cases that sought to evaluate the ability of the physicians for solving clinical problems in five dimensions: 1) identifying risk factors, 2) identifying clinical data, 3) integrating the diagnosis, 4) using diagnostic resources, and 5) using therapeutic resources. These 100 questions were balanced in 50 with correct answer "true" and 50 with correct answer "false"; each correct answer granted one point, each incorrect answer subtracted one point, and each don't know answer granted zero points for a maximum theoretical score of 100 points (maximum theoretical value). The scores were divided into six strata of clinical competence: ≤19 points = explained by random; 20-35 points = very low; 36-51 points = low; 52-67 points = intermediate; 68-83 points = high; and 83-100 points = very high.
The construction of the instrument was carried out based on the known method used in the real clinical cases discussed 13,14, and clinical competence strata was obtained by applying the Pérez & Viniegra formula with true, false and don't know answers 15.
The content of the instrument was validated by means of a consensus method, submitting it for review by five experts in the field: three endocrinologists and two internists. Internal and external consistency was evaluated by applying the instrument to two samples for convenience of 25 target and layman subjects with at least three weeks difference between the first and second application. Internal consistency was measured with Kuder-Richardson, obtaining a result of 0.94 (94%). External consistency was measured with Spearman's rank correlation coefficient and resulted in 0.93 (93%). The construct validity was evaluated comparing the results of target and layman subjects by means of Mann-Whitney U test to identify significant differences between both; results favored the target group (p≤0.05) in the overall score and the dimensions score. Finally, criteria validity was not measured as there was not a gold standard to compare the results of the instrument.
Intervention design
The scope of the educational strategy was based on the participative focus of students through communication, which uses dialog, exchange of ideas, and sharing of common actions in the diagnosis and treatment of diabetes mellitus type 2. This educational intervention lasted 6 months, and was developed for 5 hours a week divided into 2 sessions, each one of 2 hours in the classroom and 1.5 hours at the doctor's practice. The process included the following stages:
Classroom activities. After the previously selected topics had been read by family physicians, classroom sessions were followed by the specific activities detailed below:
Theoretical presentation of the topic by the expert (40 minutes), which included information on the nutritional management of type 2 diabetes mellitus.
Small group discussions (30 minutes), where the students discussed the topic presented on the previous session, including an analytical review of the literature. Each group analyzed the common points of agreement and disagreement, and the reasons that strengthen diagnosis and treatment of diabetes mellitus type 2.
Debate (30 minutes), after the small-group discussion exercise. Students made a short presentation for the entire group of their ideas, comments, disagreements and arguments.
Review of clinical cases (5 minutes), during which physicians presented a clinical case in an orderly fashion, allowing everyone to have the opportunity to participate.
Comments on the critical literature review (15 minutes), discussion and analysis of clinical cases, identification of risk factors, identification of clinical data, integration of clinical diagnosis and treatment proposals.
Activities at the doctor's practice. The whole purpose of this activity was to provide care to patients with diabetes mellitus type 2 to strengthen the use of diagnostic criteria, risk factor identification and treatment. Consultations were carried out by the group of instructors, ensuring participation of all family physicians included in the study, for which the necessary steps were taken.
Different scientific texts and articles were reviewed for the construction of theoretical contents and pedagogical materials. The strategy was developed by an internist with a master's degree in Public Health Sciences, a family physician with a master's degree in Medical Sciences, a nutritionist with a master's degree in Education, and two family physicians with a master's degree in Nutrition. All of them had plenty of experience in participatory teaching and research activities.
Data collection and analysis plan
The instrument was applied by staff external to the research before and after the intervention to both groups. Data were systematized in SPSS© version 15.0 for Windows©. Medians and intervals for overall scores and scores for each dimension were obtained, as well as frequencies distribution for clinical competence level for each group before and after intervention. Intra- and inter-group medians, before and after the intervention, were compared using the Wilcoxon test for intra-group medians and Mann-Whitney U test for inter-group medians, while changes in frequencies distribution of intra- and inter-groups, before and after intervention, were compared by means of Kolmogorov-Smirnov test, both with 95% of confidence (p≤0.05).
Ethical considerations
This research and the research protocol from which it derived were approved by the Local Committee on Health Ethics and Research No. 1301 of the Instituto Mexicano del Seguro Social, Jalisco, Mexico, who classified it as "research of minimum risk" according to the Mexican laws valid at the time of the study 16, and granted it the Register No. 2010-1301-0028. Data were collected anonymously after signing a written informed consent.
RESULTS
This study was conducted with 60 family physicians, 30 from the medical unit "A" and 30 from the medical unit "B". All of them met the inclusion criteria. No statistically significant differences were found among groups regarding age, sex, seniority and time elapsed since graduation (p>0.05).
Table 1 shows the comparison of clinical competence levels between both groups, before and after intervention, where no statistically significant differences before intervention (p>0.05) were found, although they were found after the intervention (p≤0.05). Table 2 depicts the comparison of clinical competence levels inside of groups before and after intervention. No statistically significant differences were found before the intervention (p>0.05), but they were found after the intervention (p≤0.05).
Table 1 Inter-group clinical competence level before-after the intervention
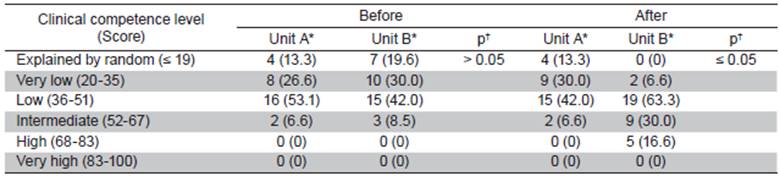
*Frequency (percentage [%]). † Obtained with Kolmogorov-Smirnov test
Table 2 Intra-group clinical competence level before-after the intervention
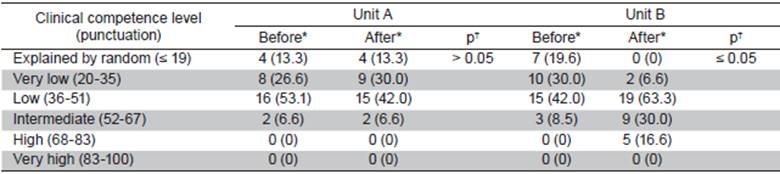
*Frequency (percentage [%]). † Obtained with Kolmogorov-Smirnov test
Table 3 shows the comparison of median overall scores and medians by dimension between both groups before and after intervention. Again, no statistically significant differences statistically were found before the intervention (p>0.05), but they were found after the intervention (p≤0.05). Finally, Table 4 shows the comparison of median overall scores and scores by dimension inside the groups, before and after intervention, finding no statistically significant differences before the intervention (p≤0.05), and statistically significant differences after the intervention (p≤0.05).
Table 3 Inter-group clinical competence median by dimension before-after the intervention
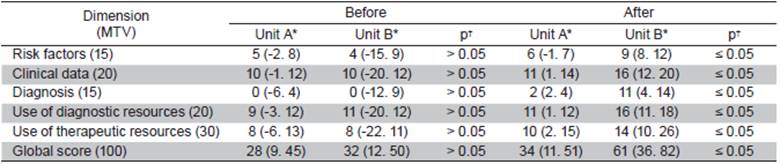
MTV = Maximum theoretical value. *Median (minimum, maximum). † Obtained using Mann-Whitney U test
DISCUSSION
Nutritional practices aimed at achieving metabolic control of patients with diabetes mellitus type 2 are a priority in family medicine promotion programs. Even with this being a priority, results in this study do not back up such policy because many physicians have a low level of clinical aptitude. This supposes an obstacle for diabetic patient's health and their families 17.
Regarding the educational process, it was observed that both groups had a homogenous distribution at the beginning of the intervention as far as clinical competence levels are concerned. After the intervention, a downward displacement in clinical ability was observed in the control group. No case was attributed to the random effect, whereas the control group showed no modifications concerning ability levels. This lack of improvement may be due to the traditional teaching-learning models utilized in the informative learning process.
There are few studies that estimate clinical aptitude of health care providers and its measure has very little institutional background; in fact, this has been studied in Mexico since 1992 4,18-21. Clinical aptitude for nutritional management of diabetic patients implies a series of complex abilities in family physicians and criteria to identify and solve in the best possible way the problematic situations in his/her daily practice.
The experimental group showed an upward displacement in competence levels of clinical ability regarding decision making in patient management. It is important to point out that only one physician was at a very low level and/or was explained by the random effect. Additionally, there was a 30% increase in medium clinical ability level and five physicians had a high level of competence 17,18.
The communicative-participative strategy, which was presented to the family physicians of the experimental group, was marked by reflection-action over the interpretation of risk factors, judgment of diagnostic and therapeutic measures, and the proposed management of the patient with diabetes mellitus type 2; these indicators of clinical ability show a relationship with the results of overall clinical ability. These observations are similar to those reported by other authors 19, which measured the effect of an educational intervention in critical readings of research reports. There was an outstanding improvement on all indicators except for those that identified signs and symptoms of diabetes mellitus type 2. Because of the persistent prevalence of these indicators in both groups, they were not modified despite the intervention.
This educational strategy, which is an alternative to the traditional model of education, allows for the improvement of family physicians at different levels, since educative methodology encourages physicians' participation in the construction of their own knowledge -created by confronting difficult, real clinical cases 20. In addition, medical and specialty programs provide little training in this regard.
Family medicine specialty education seeks to provide ideal theoretical and methodological tools 20,21 to offer comprehensive care to diabetic patients and their families. It consists of a three-year clinical rotation aiming to obtain specialized skills and knowledge on the top 30 pathologies that affect the Mexican population. The results of this study suggest a slight advantage of family medicine specialists related to their academic program and the clinical-psychosocial orientation of their practice 22. Reported results are similar to those referred by Sabido, who reports a low clinical aptitude in graduate physicians and low level in family physicians 8,9.
It is of utmost importance to acknowledge the existence of several factors influencing the results. One of the possible interpretations could be the hegemonic model of health care, which contributes to the physicians' way of thinking and the need to act in order to achieve goals and be efficient in their daily practice, given that physicians in this study have a daily practice described by an overload of consults, which hinder reflection and decision making. Also, they lack diagnostic and therapeutic resources, fact that limits their actions with serious consequences related to their lack of actual awareness and a holistic perspective of this disease.
From a pedagogical point of view, this generally low aptitude can be interpreted as a poor opportunity for family physicians in medicine school, as well as in their graduate studies, to deepen into the nutrition area. Besides this frequent use of passive-receptive traditional educational activities during their education and practice, it was found that active participation is barely promoted 22,23.
The use of instruments 12,23,24 to measure aptitude, competence and work performance is increasing in human resources formation processes and continuous work education. This type of instrument, even when it discriminates the clinical aptitude of family physicians for nutritional management, was insufficient to provide guidance about the qualitatively responsible variables related to this non-statistically significant advantage, given that both study groups were conformed and received continuous education activities that were more associated with information consumption than with the creation of knowledge from their own experience. That causes the investigation and interpretation indicators to be greater than the guidance indicator.
The instrument design considers the indicators involved in clinical aptitude (risk factors identification, clinical data identification, diagnostic integration, use of diagnostic resources and use of therapeutic resources). These indicators were chosen according to the abilities that were considered as the most important for nutritional management, since there was an attempt to approach theory (abilities that the physicians should have) and practice (abilities that they actually have). Actual case reports were used for the reviews because they were closer to the daily activities of physicians.
The instrument was designed to make physicians use their abilities to identify and discriminate between timely and pertinent decisions and actions, on the one hand, and useless (worsening), untimely or impertinent decisions and actions, on the other 8,12,19. These educational processes promote participation, so when these instruments -that allow reflection and debate from personal experience- are used, they facilitate the elaboration of own knowledge during the evaluation phase 12,19,25,26.
This educational model encouraged the involvement of family physicians through the recognition of their own knowledge, constructed in a mainstream fashion and which unchained and directed refined proposals in the clinical practice of diabetes mellitus type 2 measured by self-criticism 27,28.
In this study, the experimental group was made up of specialist in family medicine. This could explain the good effect of the educational strategy in improving the levels of clinical ability. Before the intervention, scores of clinical competences were homogeneous, which is a good indicator of base control for these variables. Thus, improvement in the experimental group was related to the effect of the educational intervention and not to a probable confounding variable 29.
The participation of a leader in the experimental group is explained by the learning commitment in the reflection-action mode. He was responsible for the development of strategies that ensured family physicians' participation. The aim of this participation was to build own knowledge from reflection-action patterns that were not present in the control group 27-29. The continuous educational model towards clinical aptitude in family physicians should foster participation, known as a way of becoming the leading actors in the elaboration of knowledge. The idea is that physicians themselves are the ones who promote and live the experience guided by self-criticism 29,30.
With the study, a reorientation of the health services offer from the institutions is expected, as well as the review of medical and residency programs and the consolidation of family medicine in the Universities that provide professional education 31-33. Finally, the use of this educational investigation as a learning tool (which allows feedback of the educative process) allows consolidation of the learning strategies, thus encouraging family physicians' participation within the scope of training schemes for their clinical practice. These methods support the development of competence concerning clinical ability at different levels and can be applied not only in patients with diabetes mellitus type 2, but in those with any other condition, which requires the physician's clinical ability to reach an accurate diagnosis and timely treatment ♦















