Ichthyozoonosis refers to diseases transmitted to humans via bacteria, viruses and parasites through fish consumption. They are associated with sociocultural factors that favor the onset of the disease, particularly the consumption of raw fish in dishes such as ceviche and sushi, or undercooked, smoked, marinated or salted fish 1-3.
In Latin America, helminth parasites are responsible for the highest number of ichthyozoonoses -causing diseases such as paragonimiasis, gnathostomiasis, anisakiasis and diphyllobothriasis-, as well as protozoans such as myxosporidia. All are considered to be emerging diseases 1,2,4-7, and the majority of clinical cases are associated with Japanese cuisine in the context of increased fish consumption 1,3,8. In the particular case of anisakis nematodes, Anisakis simplex is the species that has been most commonly linked to the occurrence of allergic reactions (type I hypersensitivity).
Public health interest in these diseases is increasing as the general population has also increased the consumption of raw or minimally processed fish products. In particular, Colombia is a country abundant in fish with coastlines along both the Pacific Ocean and the Caribbean Sea. However, it still has a low per-capita consumption of fish and shellfish compared to other countries in the world and the region. Thus, according to the Food and Agriculture Organization of the United Nations (FAO, 2014) and the Ministry of Agriculture for Rural Development in Colombia, the Colombian population consumes an average of 4.73 kg/year of fish and shellfish per person, whereas countries such as Spain and Japan consume 38 kg/year and 54 kg/year, respectively. For Latin America, the average per capita consumption of fish products is 18 kg/year 9.
Nevertheless, the increasingly globalized world has also witnessed an increase in the consumption of exotic dishes, the spread of the Mediterranean diet (rich in fish) for the prevention of cardiovascular diseases, and the permanent use of microwave ovens, which may result in undercooked foods. All these factors favor the survival of pathogens 10 and encourage the onset of ichthyozoonoses 3.
In Latin America, there is a higher number of zoonotic diseases as more people are consuming foods made of undercooked or raw fish, such as sushi 2. In Chile, cases of foodborne diseases caused by sushi skyrocketed by 100% in 2013 compared to previous years, and food poisoning cases were associated with the consumption of raw or semi-processed fish or shellfish containing nematodes, trematodes, cestodes or protozoa 11, a clinical picture related particularly to Diphyllobothrium spp., Pseudoterranova decipiens and Anisakis spp. 3,4,12,13. Furthermore, anisakidosis is considered an emerging disease in Peru 14; Diphyllobothrium and Ascocotyle characterize cases in Brazil; and fish-borne diseases are almost entirely related to Diphyllobothrium in Argentina, mainly in the region of Patagonia 15.
Chile, Peru, and Cuba have described cases of diphyllobothriasis 4, while paragonimiasis has been reported in Ecuador and Peru, where it is an endemic disease, and in other countries of the region such as Mexico, Costa Rica, Colombia and Venezuela, where it is found in a smaller number. Gnathostomiasis, on the other hand, is an emerging ichthyozoonotic disease in Latin America that affects an increasing number of people; although it was initially considered a disease exclusively found in Asia, Ecuador and Mexico have reported cases that demonstrate the existence of the disease in this region 4. Finally, Venezuela, Ecuador and Colombia have not reported cases associated with any ichthyozoonosis, but there are records of fish for consumption parasitized mainly by nematodes of the Anisakidae family 6,16,17.
Therefore, the present study aimed to determine dietary habits related to fish consumption in a population from Cali, Colombia, in order to identify the possible risk factors associated with the acquisition of an ichthyozoonotic disease.
MATERIALS AND METHODS
A descriptive, cross-sectional study was carried out on a sample of 150 healthy individuals selected by non-probabilistic sampling for convenience (accessibility and proximity of subjects). The individuals studied were students and professors of the Universidad del Valle, San Fernando Campus, in Cali, Colombia.
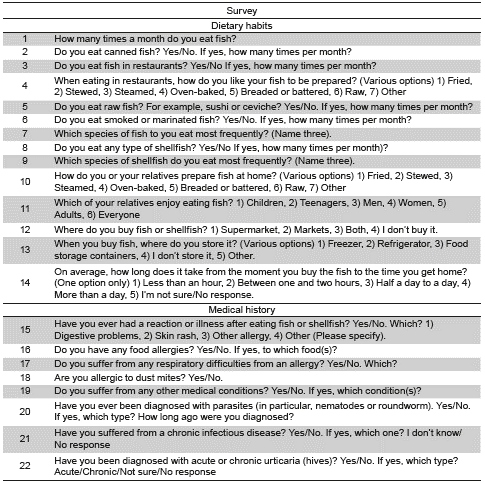
A questionnaire of 28 items on fish preparation and consumption habits was administered: 6 items were general information questions, 14 were multiple-choice questions about fish/seafood consumption, and 8 were open-ended questions about the clinical history of the participants.
The questions were designed to establish the frequency of fish and seafood consumption per month, the places of consumption (restaurants/home), preparation and/or consumption (canned, raw, salted), the species of fish consumed, and the individuals' clinical history. The survey was previously validated by means of a pilot administered to 44 participants from the same study population (Table 1).
Each participant was duly informed about the characteristics of the study and received training to complete the survey after signing an informed consent.
The SPSS version 15.0 was used for the statistical analysis, and a descriptive analysis was performed to establish the frequency and averages of variables with normal distribution such as age. Other numerical variables studied were frequency of fish intake; consumption of canned, raw, and salted fish; consumption of seafood; and consumption of fish in restaurants. It was observed that these numerical variables did not follow a normal distribution after applying the Kolmogorov-Smirnov test, so the median and interquartile ranges were estimated and the comparisons were performed using the Mann-Whitney test. Variables with p value <0.05 were considered significant.
Ethical considerations: This study was carried out in full compliance with the guidelines and the current revision of the Helsinki Declaration 18, which provides greater protection to study participants. It also complies with Resolution 008430 of 1993 from the Colombian Ministry of Health 19. The Institutional Committee for the Review of Human Ethics of the Faculty of Health, Universidad del Valle, Cali, Colombia, approved this study (code: 015-015).
RESULTS
Of the 150 participants, 84 were women (56%) and 66 men (44%), aged between 18 and 67 years, and 18 and 61 years, respectively. The dietary habits associated with fish consumption are presented in Table 2.
Table 2 Dietary habits associated with the consumption of fish and shellfish in a population surveyed in the city of Cali, Colombia
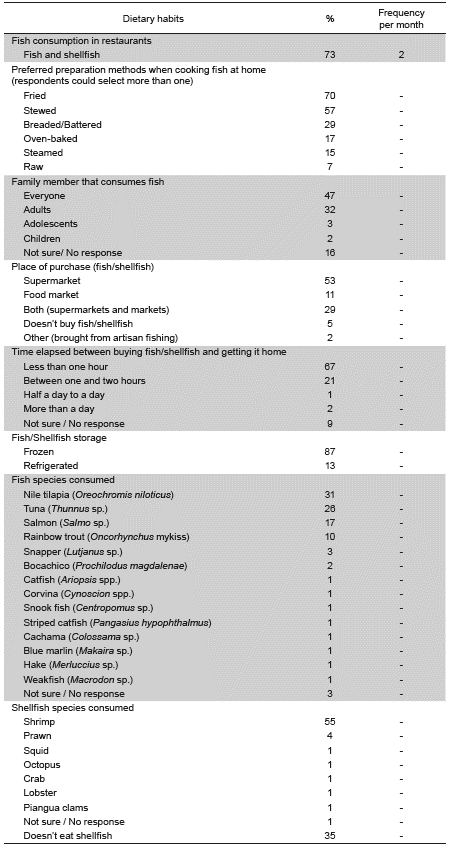
Fish consumption
The median of consumption was three times per month (interquartile range - IQR: 2-5). The median consumption of canned fish (tuna and sardines) was twice per month (IQR: 1-3). The median seafood consumption was once per month (IQR: 0-1.25). The median of eating fish or seafood in restaurants was once per month (IQR: 0 - 1.25).
Consumption of raw fish
The median consumption of raw or salted/marinated fish was once per month (IQR: 0-1.25). 19% of the respondents preferred to eat raw fish in restaurants, while the preferred form of preparation at home was fried fish (70%).
Most commonly consumed species
The 5 fish species most commonly named for consumption were tilapia (Oreochromis sp.) (31%), tuna (Thunnus sp.) (26%), salmon (Salmo sp.) (17%), trout (Oncorhynchus mykiss) (10%), and snapper (Lutjanus sp.) (3%).
Regarding seafood, participants preferred to consume shrimp (55%) and prawn (4%).
Place of purchase
53% of the respondents bought their fish in retail supermarkets and 11% in food markets.
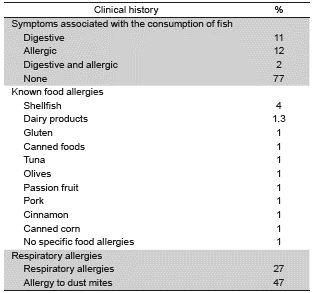
Medical history
Of the 150 respondents, 11% reported experiencing digestive symptoms associated with the consumption of fish or shellfish, and 12% some type of allergic reaction. 3 respondents (2%) reported having had both allergic and digestive symptoms.
With regard to food-related allergies, 11% reported being allergic to some type of food. 4% of all respondents reported being allergic to shellfish. 1 respondent reported being allergic to shellfish and canned fish, and another reported being allergic to seafood, passion fruit and pork. 27% of respondents reported having a respiratory allergy, while another 47% reported being allergic to dust mites. Table 3 summarizes the clinical history of the respondents.
When asked about other diseases, 2% said they had been diagnosed with a chronic infectious disease (Epstein-Barr virus and tuberculosis). The respondent with Epstein-Barr virus reported having had digestive symptoms associated with fish consumption, while the individual with a history of tuberculosis reported being allergic to dust mites. 4% of respondents stated that they had been diagnosed with urticaria and that they were allergic to dust mites; 1 had allergic symptoms caused by fish consumption, 1 reported being allergic to tuna, and 1 was allergic to dairy products.
The comparative study of the variables showed that participants consuming salted fish were more likely to suffer from urticaria (p <0.03), be allergic to mites (p <0.02) and to some foods (p <0.04). On the other hand, seafood consumption had a positive association with the probability of presenting urticaria (p <0.04). In addition, regarding the frequency of fish consumption per month, the analysis determined that the higher the intake of fish, the greater the probability of developing urticaria (p<0.001); it also identified a tendency towards significance with respect to having an allergy to dust mites (p=0.063).
DISCUSSION
This research was carried out in the city of Cali, located 122 km from Buenaventura, the main fishing port of Colombia in the Pacific Ocean and the point from where seafood is distributed to the interior of the country 20-22. Between 1998 and 2013, 1 099 568 tons of fish were caught in the Colombian Pacific region, by both industrial and artisanal fisheries 23. However, it is well known that the management of fishery products is inadequate during the extraction, processing and commercialization stages, and that it has a minimal level of processing in closed and controlled conditions. One of the main challenges for the development of the sector is the lack of dock services, in terms of processing and chilling, and this is evident in the inadequate handling of both fresh and frozen fish 22.
In the present study, the reported levels of fish consumption were generally low, although 87% of the subjects stated that they had no difficulty consuming raw or half cooked fish (sushi, marinated or salted fish), thus increasing the risk of acquiring an ichthyozoonotic disease. Moreover, the percentage of fish consumption is higher than the 74.2% reported by university students in the city of Bucaramanga 24, possibly due to the fact that only 13% of the participants in that study were from the Caribbean or Pacific coasts where fish consumption is more common based on cultural traditions.
Some of the agents that cause ichthyozoonoses are bacteria, viruses and parasites 3. In Latin America, helminth parasites cause the greatest number of these fish borne zoonoses. These parasites require aquatic organisms to complete their life cycle, and humans can act as accidental hosts by consuming infected fish carrying trematode, cestode and nematode parasites. In humans, they can cause diseases such as paragonimiasis, gnathostomiasis, diphyllobothriasis and anisakidosis, all emerging diseases in the region 3,14,25,26.
In Colombia, reports have only described some cases of paragonimiasis 25-28 and a single case of gnathostomiasis 26 of a patient diagnosed in Argentina who had been in Colombia for a few days in 2013 29. In addition, cases of fish for consumption parasitized with Anisakis nematodes have been described in different areas along the Caribbean coast (17,29X28-31); even though there are no reports of cases in humans in Colombia, these parasites have a global distribution and are found in several ecologically important species. Therefore, they are an emerging and permanent concern for food safety entities as they not only produce digestive or extraintestinal symptoms associated with raw fish consumption, but also cause allergic conditions 32. Consequently, several disciplines have become interested in this parasite, not only in the field of fisheries, parasitology and food safety, but also in several medical specialties, particularly allergy and immunology 32.
This study found that respondents between 26 and 45 years of age reported eating raw fish more frequently in dishes such as sushi -up to 5 times per month-, making evident the increasing popularity of Japanese food and a more Mediterranean-style diet among the younger population. These dietary trends increase the potential risk of developing ichthyozoonotic diseases in Colombia, requiring further research to have a clearer picture of the situation. Another area for further study is the development and availability of specific diagnostic tests for diseases that can be of importance for public health and medicine.
Control and prevention measures for these diseases are relatively simple. In Europe, where they are fully identified, legislation states that any fish to be consumed raw or undercooked should be frozen at -20°C for at least 24 hours, and that the finished product should be frozen in its entirety (Regulation EC No.854/2004 of the European Parliament and of the Council of April 29 2004) 33. In Colombia, these pathogens are not identified and, therefore, are not diagnosed, so there is no clear legislation in this regard. However, the Ministry of Health established - through Decree No.561 of March 8, 1984 34, article 21, regarding the capture, processing, transport and sale of fishery products, that the evisceration can be carried out as soon as the catch arrives onboard; however, if the process is not carried out immediately, the product must be washed once it reaches the deck using drinking water or clean sea water. Not performing the evisceration immediately facilitates the movement of parasites, such as Anisakis, from the viscera to the musculature of the fish, thus increasing the risks for the end consumer. Nevertheless, the microbiological requirements for fishery products set out in Resolution 776 of 2008 from the Ministry of Social Protection 35 only establish the analysis for the identification of E. coli, Staphylococcus spp., Salmonella spp. and Vibrio cholerae.
Further risk comes from the increase of imported seafood. In 2017, to meet growing domestic demand, the Colombian Aquaculture and Fisheries Unit imported 180 million tons of fish from Asia, where, as mentioned above, parasitic diseases are endemic and constitute a public health issue. Increasing fish imports to Colombia may elevate cases of emerging fish borne zoonotic diseases. It is worth noting that 53% of the participants of this study purchased fish in supermarkets and only 11% purchased it from local food markets. Supermarket purchases favor the consumption of imported fish, mainly of Asian origin, as they are often cheaper than local fish species.
The most commonly consumed fish species reported by the survey respondents were tilapia (Oreochromis niloticus), tuna (Thunnus sp.), salmon (Salmo sp.), trout (On-corhynchus mykiss) and snapper (Lutjanus sp.). Regarding shellfish, respondents preferred to consume shrimp and prawn. These results coincide with the research conducted in 2015 by Restrepo-Betancourt et al.36, who found that the preferred species of university students in the city of Medellín were tuna, tilapia, trout and shrimp; in turn, Gamboa-Delgado et al. administered another survey to university students in Bucaramanga, and also found that they preferred trout, snapper and tuna 24. In 2005, Hererra-Arias et al.37 found a high prevalence of Salmonella spp. in commercialized fresh trout in Pamplona, (department of Norte de Santander, Colombia), with similar prevalence levels of the pathogen in fish products sold in formal establishments and those sold more informally, demonstrating the presence of pathogens in the species preferred for consumption.
In the literature review, there were no reports of an association between fish for human consumption and ichthyozoonotic diseases in Colombia, possibly because they are emerging diseases that are largely unrecognized by the local health staff, making underreporting likely. However, there are reports of fish consumption with presence of anisakis geographically related to the Caribbean Sea, both in the sea and in continental waters, where several authors have found Contracaecum sp. 31. Moreover, anisakis parasites have been identified in species in other Latin American countries: in Chilean jack mackerel (Trachurus murphyi) and Argentine hake (Merluccius hubbsi) in Argentina; in Peruvian hake (Merluccius gayi) and Lorna drum (Sciaena deliciosa) in Chile and Peru; in anchovy (Pomatomus saltatrix), largehead hairtail (Trichiurus lepturus) and red porgy (Pagrus pagrus) in Brazil; and in species of the Mugilidae and Gerreidae families in Venezuela 16,38,39.
In the final section of the survey, respondents were asked about their medical history: 11% reported having digestive symptoms associated with fish consumption, 12% reported allergic symptoms for the same cause, and 2% reported both digestive and allergic symptoms. These percentages are higher than those reported by Gamboa-Delgado et al. in 2010, who found that 9.6% of the student population surveyed at the Universidad de Bucaramanga were allergic to fish 24 and 4% were allergic to shellfish. These data, along with the high frequency of dust mite allergy, are not unexpected in a population living in a humid climate. The association between sensitivity to dust mites and suffering from allergies to shellfish, especially from the group of crustaceans and frequently caused by cross-reactivity of allergens 40, has been well documented. The percentage of respondents who were allergic to dust mites far exceeds the percentage of patients who claim to have a respiratory allergy. Since it is a questionnaire, it was not possible to rule out an understanding bias on the part of the patient. However, it is possible that the allergy study performed on patients allergic to mites was performed for other reasons, e.g. episodes of urticaria, food allergies, etc., given the frequent sensitivity to dust mites in tropical zones.
A relationship between fish consumption and allergies was confirmed. Further research is necessary to establish the possible pathogens associated with hypersensitivity, such as parasites of the Anisakidae family ♦