Falls among community-dwelling older adults are a leading cause of unintentional injury and death worldwide and are a growing public health concern 1,2. Approximately 20% of the older adults who fall seek medical attention to rule out injuries 3-5. Of the people who fall and then visit the emergency room, more than 40% result in hospital admissions; this is increasingly true in those with injuries 2,6,7. Older adults having falls requiring medical attention are also at risk of greater mortality, excessive costs for treatment, functional decline and to be discharged to a nursing home 8,9.
Currently understood risk factors for falls that cause injury include age, female gender, use of sedatives, gait impairment, extremity weakness, sleep disorders, functional impairment, sensory impairment, cognitive impairment, history of fractures, and comorbidities such as arthritis, diabetes, depression, urinary incontinence, Parkinson's disease, and history of stroke 1,10-14.
While falls requiring medical attention or causing injuries have been researched extensively 1,6-14, this is the first analysis to consider risk factors for falls requiring medical treatment across Latin American cities 15. The objective of this study is to estimate the prevalence of falls requiring medical treatment, referred as 'medical falls' 8, as well as the risk factors associated with those falls in older adults. To carry out this analysis, we examined data of the SABE surveys from Latin American (LA) cities and Bogota city.
METHODS
Data and design
To carry out this study, we used secondary analyses of SABE datasets 16,17. The SABE-LA study is a cross sectional study that was conducted in seven different Latin American and Caribbean cities (Bridgetown, Buenos Aires, La Havana, Mexico, Montevideo, Santiago, and Sao Paulo). It consists of surveys completed by men and women ages 60 and older from 1999-2000 18. Each of the 7 cities' sample consists of 1500-2000 individuals as well as their surviving spouse (total 10,587) 18. The SABE-Bogota study is a cross-sectional study of non-institutionalized men and women aged 60 or older residing in Bogota, Colombia. It includes 2,000 subjects who were interviewed in 2012 17. In total, 12,487 subjects were analyzed in the pooled sample of 8 cities for this article. Oral and written consent forms were obtained from all subjects and approved by the Human Subjects Committee and the corresponding Medical Research Institution or University in each city, in the original studies 17,18. Personal identifiers were deleted to make the datasets public available for secondary analyses.
Measures
Outcome variable
Prevalence of falls in the SABE-LA and SABE-Bogota studies were obtained by asking each subject: "Have you fallen down in the last 12 months?" A positive response was followed by "How many times have you fallen?", and subsequently, "Did you suffer an injury that required medical treatment or go to the hospital?" Fall status was categorized as 19: 1- No falls; 2- 1 fall with no medical treatment; 3- ≥2 falls with no medical treatment; and 4-≥1 fall requiring medical treatment - or medical falls 8.
Independent variables
The following variables were included: age, gender, level of education and medical conditions (history of arthritis, diabetes mellitus, hypertension, urinary incontinence, cancer, stroke or myocardial infarction). Any response other than 'excellent' or 'very good' vision ('good', 'fair' or 'poor') to questions related to distant or near vision was coded as visual impairment. Similarly, respondents were marked as having 'impaired' hearing if their response was anything other than 'excellent' or 'very good' ('good', 'fair', or 'poor'). Activities of daily living (ADLs) was dichotomized into either 'no help needed' versus 'needs help with or being unable to perform one or more of the seven activities' (walking across a small room, bathing, grooming, dressing, eating, transferring from a bed to a chair, and using the toilet) 20. Self-rated health was considered 'poor' if they responded 'fair', or 'poor' (vs. 'excellent', 'very good', or 'good'). Depressive symptomatology was measured using the Geriatric Depression Scale (GDS) which contains 15 items, where high depressive symptoms are considered a score of ≥6 21. Last, the abbreviated Mini Mental State Examination (AMMSE) consists of nine items, and scores can range from 0 to 19, where a score <13 is considered positive for cognitive impairment in the SABE surveys 22.
Data analysis
Weighted prevalence of both falls requiring medical treatment and falls not requiring medical treatment were calculated. Chi-square and ANOVA tests were utilized for bivariate comparisons in the pooled sample of the 8 cities of study variables according to fall category, based on Pohl et al. falls' categorization 19, each participant was placed into. To select the variables to be included into the multivariate models, the backward elimination selection method was used. The fit of the models was checked by the Hosmer-Lemeshow test. Then, weighted multivariate logistic regression analyses, with the SURVEYLOGISTIC procedure, were used to estimate the odds of suffering a medical fall compared to people without a history of falls.
Finally, the occurrence of medical falls according to the number of risk factors was also calculated. All analyses were performed using the SAS System for Windows, version 9.4 (SAS Institute, Inc., Cary, NC). Statistical level of significance was set at p<0.05.
RESULTS
Figure 1 illustrates the prevalence of falls not requiring medical treatment as well as the prevalence of medical falls across all 8 cities. The highest prevalence of medical falls was reported in Mexico City (11.3%), with the lowest prevalence in Bridgetown (6.0%). In the pooled sample, the overall prevalence of medical falls was 9.9% (12.4% for women and 6.2% for men).
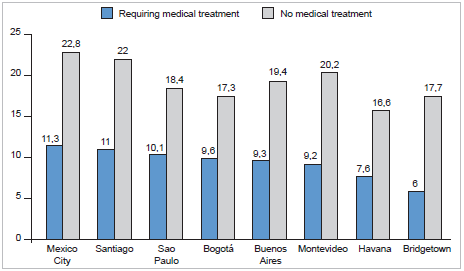
Figure 1 Weighted prevalence of falls requiring or not medical treatment in each Latin American city
Table 1 presents the characteristics of the pooled sample, as well as the characteristics of the groups stratified by fall status. Compared to subjects with no falls, subjects with ≥2 falls and no medical treatment and those with ≥1 falls requiring medical treatment [medical falls] tend to be female, and have greater age, more comorbidities, have sensory impairment, high depressive symptoms, cognitive impairment, poorer self-perception of health, and any ADL limitations.
Table 1 Characteristics of pooled sample of participants and status with respect to falls
| Characteristics | Total | No falls | 1 fall, no medical treatment | ≥2 falls, no medical treatment | ≥1 falls, requiring medical treatment (medical falls) |
|---|---|---|---|---|---|
| N=12,487 | n=8,874 | n=1,151 | n=1,258 | n=1,204 | |
| Mean ± SE or % | Mean ± SE or % | Mean ± SE or % | Mean ± SE or % | Mean ± SE or % | |
| Number of falls | 2.2 ± 0.1 | 0 | 1 | 3.2 ± 0.1 | 2.4 ± 0.1 |
| Age (years) | 70.3 ± 0.1 | 69.8 ± 0.1 | 71.0 ± 0.3 | 72.1 ± 0.3 | 71.6 ± 0.3 |
| Female | 60.0 | 55.9 | 62.6 | 71.3 | 75.0 |
| Education (years) | 5.9 ± 0.1 | 6.1 ± 0.1 | 5.6 ± 0.2 | 4.7 ± 0.2 | 5.5 ± 0.2 |
| Arthritis | 38.7 | 36.4 | 37.0 | 48.0 | 47.1 |
| Diabetes | 16.2 | 14.7 | 20.4 | 21.1 | 17.6 |
| Heart attack | 17.9 | 16.8 | 16.9 | 21.2 | 22.8 |
| Hypertension | 49.1 | 47.5 | 47.3 | 54.1 | 57.1 |
| Stroke | 5.7 | 4.7 | 6.6 | 9.5 | 7.6 |
| Cancer | 4.3 | 4.0 | 4.5 | 5.5 | 4.9 |
| Urinary incontinence | 14.8 | 11.3 | 16.1 | 28.2 | 24.3 |
| Vision problem | 78.0 | 77.2 | 76.8 | 81.5 | 81.6 |
| Hearing problem | 24.4 | 23.8 | 28.5 | 36.0 | 33.0 |
| Depression | 17.8 | 15.1 | 18.6 | 25.5 | 28.1 |
| Cognitive impairment | 7.0 | 5.8 | 7.1 | 12.5 | 9.7 |
| Poor self-rated health | 51.2 | 47.5 | 51.8 | 64.6 | 63.5 |
| Any ADL limitations | 17.1 | 13.4 | 20.9 | 29.4 | 27.6 |
Data are weighted. SE= standard error of the mean. All p-values across the four categories were significant with p<.001 (except for cancer, heart attack, and vision problem). ADL= activities of daily living.
Table 2 shows the results of the weighted multivariate logistic regression analyses. Significant independent risk factors for ≥1 medical falls are age ≥80, female gender, urinary incontinence, high depressive symptoms, poor self-rated health, and any ADL limitations.
Table 2 Weighted odds for falls, according to requiring or not medical treatment, pooled sample of 8 cities: 7 cities fromSABE from Latin America and the SABE Bogota
| Characteristics | Model 1 | Model 2 | Model 3 | p-value | ||
|---|---|---|---|---|---|---|
| 1 fall, no medical treatment | ≥2 falls, no medical treatment | ≥1 falls, requiring medical treatment (medical falls) | ||||
| n=1,151 OR (95% CI) | p-value | n=1,258 OR (95% CI) | p-value | n=1,204 OR (95% CI) | ||
| Age ≥80 | 1.04 (0.80-1.36) | 0.7682 | 1.33 (1.02-1.72) | 0.0326 | ||
| Female | 1.27 (1.04-1.56) | 0.0192 | 1.69 (1.38-2.09) | <.0001 | 2.07 (1.69-2.53) | <.0001 |
| Education ≤5 years | 1.11 (0.91-1.36) | 0.2792 | 1.43 (1.16-1.75) | 0.0007 | ||
| Arthritis | 1.27 (1.04-1.55) | 0.0175 | 1.16 (0.95-1.41) | 0.1447 | ||
| Diabetes | 1.39 (1.08-1.79) | 0.0134 | 1.29 (1.02-1.64) | 0.0312 | ||
| Heart attack | 1.08 (0.85-1.37) | 0.5154 | 1.12 (0.90-1.41) | 0.3075 | ||
| Stroke | 1.54 (1.09-2.17) | 0.0126 | 1.31 (0.89-1.93) | 0.1686 | ||
| Urinary incontinence | 1.20 (0.93-1.56) | 0.1648 | 1.81 (1.42-2.30) | <.0001 | 1.51 (1.18-1.92) | 0.0009 |
| Vision problem | 1.12 (0.88-1.43) | 0.3568 | 1.14 (0.90-1.45) | 0.2641 | ||
| Hearing problem | 1.36 (1.11-1.66) | 0.0034 | 1.22 (0.99-1.50) | 0.0561 | ||
| Depression | 1.14 (0.90-1.45) | 0.2687 | 1.35 (1.08-1.68) | 0.0075 | 1.53 (1.24-1.91) | 0.0001 |
| Cognitive impairment | 1.50 (1.12-2.01) | 0.0064 | 1.13 (0.82-1.55) | 0.4501 | ||
| Poor self-rated health | 1.24 (0.99-1.55) | 0.0515 | 1.35 (1.10-1.66) | 0.0038 | ||
| Any ADL limitations | 1.53 (1.16-2.01) | 0.0024 | 1.39 (1.09-1.77) | 0.0066 | 1.48 (1.16-1.87) | 0.0014 |
OR= odds ratios; CI= confidence intervals; ADL= activities of daily living. Models are compared to no falls (n=8,874). Adjusted for all variables in the table.
There was a significant increase in the occurrence of medical falling (Mantel-Haenszel Chi-squared (X2) 364.446; P<.0001) as the number of risk factors in-creased (Figure 2).
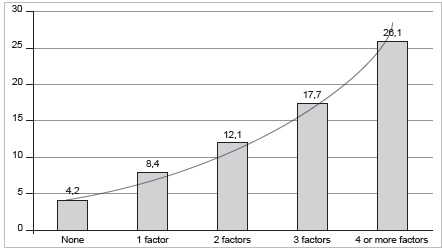
(N=12,487). The risk factors included age >80 years, female gender, urinary incontinence, high depressive symptoms (GDS>6), poor self-rated health, and any activities of daily living limitations. There was a significant increase in the occurrence of medical falling (P<.0001) as the number of risk factors increased.
Figure 2 Occurrence of medical falls according to the number of risk factors in older Latin Americans
DISCUSSION
This study demonstrates that the estimated prevalence of medical falls varies widely across Latin American cities. We also found that potentially modifiable risk factors correlate with a higher risk of suffering a medical fall. Further, a higher number of falls does not necessarily imply a higher likelihood of suffering a fall-related injury. This differs from a previous study, as it was previously thought that risk of injury is approximately proportional to the cumulative number of falls 23.
The prevalence of medical falls was approximately half of those that did not require medical attention. There is some variation between our results and other previous studies. For instance, our pooled prevalence of medical falls (9.9%) is higher than one study in Brazil (7.8%) 24.
Another previous study found that risk factors for fall-inducing injuries were like those for non-injurious falls 13. However, our study demonstrates that there are more identifiable risk factors among those persons with multiple falls (>2) that do not require medical attention. In contrast, the risk factors for falls requiring medical attention are more selective. Among these, some are potentially modifiable. These include incontinence, high depressive symptoms, ADLs limitations, and poor self-rated health 10-14.
On the other hand, self-rated general health is an important measure used in public health to assess the health of the older adults living in the communities. Like our findings, poor self-rated health has been associated with falling and frailty in Colombian older adults 25. A com-mon consequence of falling is fear of falling which has been also found associated with poor self-rated health in Colombian older adults living in the community 26.
Furthermore, we found that self- reported functional limitations are also linked with poor physical function and quality of life among older adults in other studies 17,27.
One potential limitation of this study is that the collected data for falls and comorbidities were self-reported. This allows for a potential recall bias. Another limitation is the reliance in cross-sectional data, which prevents us from establishing cause and effect between certain variables and falls. Finally, we were unable to control for environmental factors that are currently known to contribute to falls in the community.
In summary, our findings support the development of future public health efforts directed at early intervention and treatment of modifiable health conditions in order to prevent medical falls.
Additionally, preventive measures targeting these potentially modifiable risk factors may help to decrease the risk for medical falls in community-dwelling persons, age 60 and older, in Latin American cities.














