The reproductive process of living beings involves a series of physiological changes that occur within the specific patterns known, which is mediated by the particularities of each individual, sometimes the reproductive moment and pregnancy pass in coincidence with disease states of the mother that depends on the reproductive process itself, or that exist and known before or during the course of pregnancy 1.
The above, this leads to the magnitude of the negative impact of Chronic Non-Communicable Diseases (CNCD) in the process of pregnancy, which when pre-existing to pregnancy, exacerbate or complicate the mother and the newborn child's, which represent health and reproductive problems and cost for a health system.
Little is known, however, about the prevalence of CNCD in pregnant women or how many women with chronic illness have Access to care after delivery-either through a continuous source of insurance or a regular provider of health care. It is also not known how much CNCD adds to the health care costs in age pregnant women 2.
In studies carried out on pregnancy and the most prevalent CNCD, it has been found, in the case of Diabetes Mellitus (DM), pregnancy causes a deterioration of the metabolic control of DM1 and DM2 3,4. There were exposed the effects of this pathology on pregnancy, finding such serious effects as: embryopathy (anencephaly, microcephaly, congenital heart disease), preeclampsia 5, polyhydramnios, macrosomia 6, abortions, fetal losses, preterm birth, dystrophic births, higher caesarean section rate, perinatal mortality, neonatal hypoglycemia, neonatal hyperbilirubinemia, and increased risk of obesity and DM2 in the child.
The obesity is a precursor to CNCD 7, increased risk of maternal complications such as gestational diabetes, hypertension, preeclampsia, HELLP syndrome (hemolysis, increased liver enzymes and thrombocytopenia), obstructive sleep apnea, thromboembolism, increased fetal malformations (neural tube defects, heart disease, hydrocephalus, cleft lip, ano-rectal atresia) 8. And with regard to childbirth, the higher rate of caesarean sections, surgical complications, macrosomia, greater risk of maternal and fetal obstetric trauma, plus prematurity iatrogenesis derived from maternal medical causes 3.
As for Arterial Hypertension (HT), which is defined as chronic HT in pregnancy known before pregnancy, or detected before week 20, its effects on pregnancy could be condensed into: abruptio placentae, preterm birth, cesarean section, low weight, admission to neonatal unit and perinatal death. The preeclampsia appears in 17.0-25.0% of cases 9.
Taking into account the above, it can be stated that this situation is of such importance that it results in the generation of a high economic (health system) and social (family, community) cost, by a party directly associated with the cost of care derived from complications from pregnancy, childbirth and/or the puerperium that are contemplated from a longer than expected hospital stay, increased demand for high complexity services, prolonged treatments, and even permanent disability care that can occur in relation to the effects of pregnancy in women suffering from CNCD 10.
As a mechanism to aid in the economic control of health systems, contraceptive mechanisms have been implemented in women with high-risk pregnancy, for example, in Mexico the High Reproductive Risk Modules (MARR) project has been incorporated, the intervention consists of in implementing, in the hospital units where this type of women is attended, medical care centers, which have the function of providing vulnerable patients access to a set of contraception interventions, trying to prevent pregnancy from becoming a additional morbidity factor for the patient, and that could contribute to a fatal outcome 11.
The purpose of our study was carried out an analysis on the cost of pregnancy of women with high obstetric risk where there is a directly proportional relationship between high-cost disease burden and pregnancy complications. The research question is: What is the impact of pregnant women with a high disease burden, especially with CNCD in the costs of a health insurer?
MATERIALS AND METHODS
Study type
Retrospective costing study conducted at Famisanar EPS between 2016 and 2018. The insurer's perspective was taken into account for the analysis.
Data source
In Colombia, universal healthcare services are provided by health insurance (EPS) that is obligated to insurance every citizen who wishes to join them (obligatory public health system). This study was conducted in Famisanar EPS. It has one central data base are automatically updated with differents services f.e. hospitalization, laboratory test, medical treatment and others, who is issued a unique identification number (in this study the identification number was anonymized). Famisanar EPS delivers its service via third-party providers. All medical services have a rate that can be used for billing purposes. It used differents forms payment (fee for service, per period, episode, bundled payment and others). Famisanar EPS's databases allow for all costs to be calculated according to the medical service given for each identification number.
We calculated the pregnancy total costs for each patient for the years 2016, 2017 and 2018. Pregnancy total costs per patients was routinely calculated by the Famisanar EPS information department that included indirect and direct medical costs components without the administrative costs. We converted at a representative rate of the dollar price to the market of December 2018 (USD 1.00 = COP 3,250.00).
Famisanar EPS has several computerized patient registries. These registries were validated for physicians that use the registries to assess treatment and outcomes. Using advanced networking information technology theses registries currently make use inclusion criteria and marcation in the sistem for identification the differents diseases how hypertension, diabetes mellitus, diabetes mellitus/hypertension, oncology, rheumatology and collagen diseases and others (bariatric surgery, dyalisis, chronic obstructive pulmonary disease, multiple sclerosis, cystic fibrosis, hemophilia, pulmonary hypertension and transplant). We used International Codification Diseases version 10 (ICD-10) for diagnosis primary and secundarys and Unique Codes for the Provision of Colombian Health Services (CUPS) por the medical services 12.
Stastistical methods
The analysis had two components: descriptive and comparative. To examine the bivariate group differences in the presence of CNCD among pregnant women and among all 4 study groups, chi square test was used (P<0.05). Additionaly, logistic regression on the odds of belonging to 1 of 3 groups compared with the reference group (pregnant healthy's women) was performed to examine group differences for age. Parameter estimates from logistic regressions were converted to Adjusted Odds Ratio (AOR) were presented for ease interpretation. All analyses were condubted using standard statistical software en this case SPSS® version 25.0 2,13.
RESULTS
Prevalence use of contraceptives and chonic conditions
The study universe was made up of 458 249 women of childbearing age affiliated to Famisanar EPS between 15 and 49 years, of which 24 030 (5.2%) women have some relationship with the CNCD, of these, 2 454 (10.2%) went to childbirth and caesarean section. The average age for CNCD'S were 40.0 (S.E.±7.7) and for healthy's women 27.4 (S.E.±6.4). The average pregnancy age for CNCD'S were 32.6 (S.E.±6.4) and for pregnancy healthy's women 36.1 (S.E.±3.2). The annual pregnancy rate was 19.5 in healthy's women and 102.1 in CNCD'S women.
We had determined that the use of contraceptives in healthy's women were 31.0% (18 069) and were distributed as follows: sterilization 11.4% (5 363), barrier 4.9% (2 307), injectable month 6.4% (3 030), oral 4.3% (2 027), intrauterine device (IUD) (1 947) 4.1%, injectable quarterly 2.9% (1 361) and others 11.3% (2 034). Therefore, the contraceptive methods's failure to healthy's women were 11.0% (1 988).
As well, we had determined that use of contraceptives in CNCD'S women were 51.2% (12 311) and were distributed as follows: sterilization 25.1% (3 091), barrier 18.6% (2 290), injectable month 10.9% (1 341), oral 10.5% (1 293), intrauterine device (IUD) (1 194) 9.7%, injectable quarterly 8.2% (1 009) and others 4.5% (2 093). Therefore, contraceptive methods's failure in CNCD'S women were 15.4% (1 897).
The CNCD'S women were distributed as follows: hypertension 56.2% (P<0.05), diabetes mellitus 10.6% (P<0.05), rheumatology 8.9% (P<0.05), oncology 8.8% (P<0.05), diabetes mellitus/hypertension 6.6% (P<0.05) and others 8.9% (P<0.05). The pregnant CNCD'S women was made up of: hypertension 52.2% (P<0.05), diabetes mellitus 21.5% (P<0.05), oncology 7.2% (P<0.05), rheumatology 7.0% (P<0.05) and others 12.1% (P<0.05).
Health care expenditures
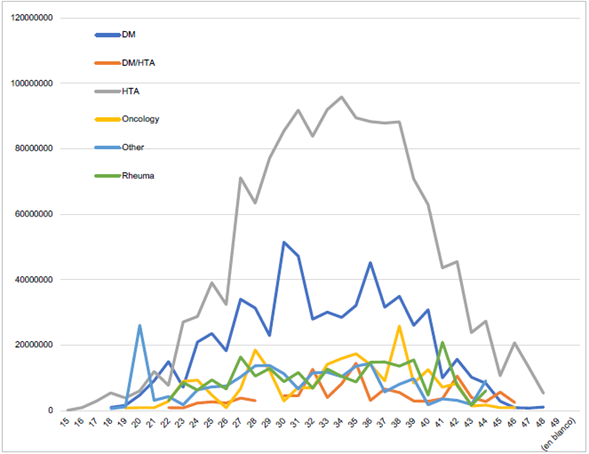
It shows that the highest costs of care in pregnancy CNCD'S women are hypertension (USD 1,477.61) and rheumatology (USD 1,316.94). The Table 1 and Figure 2 shows the distribution result by diseases and costs.
Table 1 Pregnancy CNCD's women for diseases
| Disease | Age | COP | USD |
|---|---|---|---|
| DM | 31.6 (S.E. +-6.3) | 1,635,216.32 | 503.14 |
| DM/HT | 33.4 (S.E. +-6.3) | 2,682,849.16 | 825.50 |
| HT | 33.0 (S.E. +-6.4) | 4,802,240.67 | 1,477.61 |
| Oncology | 32.1 (S.E. +-6.5) | 2.994.603,12 | 921.42 |
| Rheumatology | 31.8 (S.E. +-6.2) | 4.280.056,44 | 1,316.94 |
| Others | 31.3 (S.E. +-6.8) | 2,267,092.10 | 697.57 |
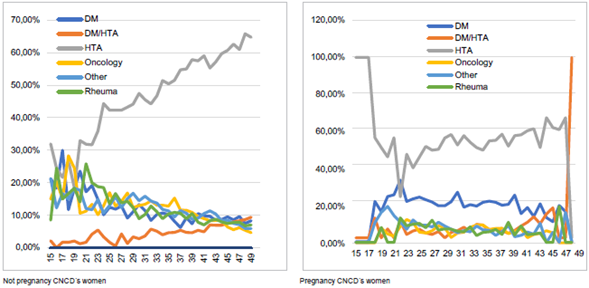
Figure 2 Age and pregnancy CNCD´s women - not pregnancy CNCD´s women specific prevalence of selected. Famisanar EPS 2016 - 2018
Similarly, it determined the costs of pregnancy healthy's women and pregnancy CNCD'S women in terms of the costs for the gestation care (included complications) and of newborn child's complications at birth. The costs of care for newborn child's and pregnant women are higher in CNCD'S women vs. healthy's women. The Table 3 and Figure 4 shows the results.
Table 3 Costs in pregnancy care complications and newborn child's complications for CNCD's women and healthy's women
| CNCD's women | Healthy's women | Percentage (%) | ||||
|---|---|---|---|---|---|---|
| COP | USD | COP | USD | |||
| Pregnancy care (included complications) | 1,689,823.17 | 519.95 | 651,321.69 | 200.41 | 97.5 | |
| Newborn child's complications | 7,130,101.96 | 2,193.88 | 4,368,242.62 | 1,344.07 | 63,2 | |
In the same way, it made the calculation of the costs in pregnancy CNCD'S women for diseases in childbirth and caesarean care finding that critical care represents 47.8% of costs, hospitalization 26.1%, event obstetric 15.2% and others 10.9%. In the event of the newborn child's complications the distribution is the critical care represents 51.5% of the costs, the medications 32.4% and others 16.1%.
Differences in demographics and access to care
Similarly, the Table 5 describes the characteristics of the study sample of 4 groups of women with and without pregnant and with and without CNCD. All variables were significant in the chi-square analysis, at the 5.0% level for age, zone and ingress.
Using multinomial regression, we compared the pregnancy with CNCD with the other groups of women. We did not observe any significant differences in ingress and zone. However, we observe signicant differences in the age, (Table 6).
Table 5 Profile of women in the age group 19 - 49 years by pregnancy and CNCD. Famisanar EPS 2016 - 2018
| Not pregnant healthy's women | Not pregnant CNCD's women | Pregnant healthy's women | Pregnant CNCD's women | |||||
|---|---|---|---|---|---|---|---|---|
| N | wt% | N | wt% | n | wt% | N | wt% | |
| All | 63,895 | 71,6 | 21,575 | 24,2 | 1,269 | 1,4 | 2,454 | 2,8 |
| Age | ||||||||
| 15-29 | 3,189 | 53,5 | 2,019 | 33,9 | 1 | 0,0 | 752 | 12,6 |
| 30-34 | 4,836 | 60,8 | 1,974 | 24,8 | 459 | 5,8 | 683 | 8,6 |
| 35-39 | 18,535 | 79,6 | 3,507 | 15,1 | 585 | 2,5 | 650 | 2,8 |
| 40-49 | 37,335 | 71,8 | 14,075 | 27,1 | 224 | 0,4 | 369 | 0,7 |
| Zone | ||||||||
| Atlantic Sea | 1,493 | 74,3 | 436 | 21,7 | 43 | 2,1 | 37 | 1,8 |
| Center Country | 5,161 | 39,1 | 6,593 | 50,0 | 720 | 5,5 | 720 | 5,5 |
| Bogotá D.C. | 55,663 | 77,2 | 14,307 | 19,8 | 452 | 0,6 | 1,677 | 2,3 |
| Eastern plains | 1,578 | 85,1 | 239 | 12,9 | 18 | 1,0 | 20 | 1,1 |
| Ingress | ||||||||
| < USD 250 | 9,896 | 84,3 | 1,458 | 12,4 | 124 | 1,1 | 267 | 2,3 |
| USD 251 - USD 500 | 41,075 | 88,1 | 4,446 | 9,5 | 434 | 0,9 | 664 | 1,4 |
| USD 501 - USD 750 | 6,099 | 76,9 | 1,479 | 18,6 | 133 | 1,7 | 223 | 2,8 |
| USD 751 < | 6,825 | 78,8 | 1,551 | 17,9 | 112 | 1,3 | 176 | 2,0 |
Table 6 Adjusted Odds Ratio (AOR) and 95% confidence interval from multinomial on pregnancy and CNDC categories. Famisanar EPS 2016 - 2018
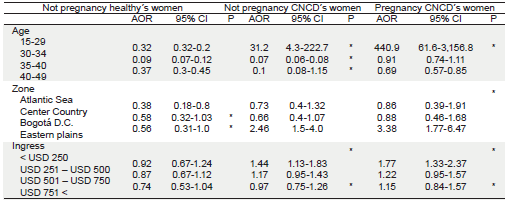
Note: Based on 63,895 women aged between 15 and 49 years. Asterisks denote significant (P<0.05) group differences compared to the reference group based on multinomial logistic regression on the precence of CDCD and pregnancy. The regression also includes an intercept term. The reference group for the depend variable is a pregnancy healthy's women.
DISCUSION
This is one study using a Colombia insurance database to describe the prevalence use of contraceptives, CNCD in pregnancy women and health care expenditures. We found that the prevalence of CNCD overall was lower in non pregnant women (25.2) than pregnant women (65.9) age 15-49 years.
Our study is very close to the results found in the Women's Health Study of the Center of Pennsylvania, Weisman et al. (2006) regarding arterial hypertension, however, we did not take into account mental illnesses 14.
According to our study results, despite the implementation of contraceptive mechanisms, these have failed between 11.0% and 15.4% of pregnancies in CNCD'S women; the results prove what Holton et al. (2018) on the consequences for health care providers and CNCD'S women and the importance of addressing possible assumptions about the inability of CNCD'S women to get pregnant. It is very important that women receive information on affected contraceptive methods and pre-pregnancy care 15.
Additionaly, the objetive of this study was to examine indirectal and indirectal costs of CNCD in pregnancy. Our results indicate that treatment of CNCD in pregnancy imposes a substancial economic borden on Famisanar EPS in Colombia, checking what was mentioned by Chodick et al. (2010) 13. Common pre-existing conditions in pregnant women may result in the use of additional resources and cost for mothers and newborn child's 16. Pregnancy in CNCD women costs 97.5% more in pregnancy and 63.2% again in the CNCD mother's newborn children. This is a new contribution from our study.
We check what is mentioned by Chodick et al. (2010) and Jovanovic et al. (2015) on the complications and costs of medical care were higher with diabetes mellitus, which highlights the need to optimize the treatment of diabetes mellitus during pregnancy 13,17. The results indicate that hypertension and diabetes mellitus impose a considerable economic burden 18. We agree with the statement of Barton et al. The use of outpatient treatment services for women with pregnancy-related hypertension reduces the need for hospital care and is cost effective 19. Likewise, the increase in the use of health services and health costs during pregnancy are associated with the increase of obesity 20.
We found that CNCD was relatively common in pregnancy and childbearing women and found few significant cost differences between pregnant healthy's women and pregnant CNCD'S women. This is very interesting for insurances.
There are limitations to our study. First, we did not include all CNCD in our analysis, we excluded chronic neurologics and mental diseases. Second, we use ICD-10 in Colombia for primary and secondary diagnosis, but the number of secondary diagnoses in information systems is very poor 21. Third, the study did not include the out of pocket of families. Finally, by limitations in the database we were not able to access the data model as important as marital status, education and employment.
In conclusion, our study presents the use of a population-based computerized database to comprehensively assess the cost CNCD diseases (hypertension, diabetes mellitus, rheumatology, oncology, diabetes mellitus/hypertension and others). Pre-existing CNCD in pregnant women can lead to the use of additional resources in the health system. CNCD in society represent a severe burden for a health system due to high costs and especially when talking about women who have an CNCD and are pregnant. The study also indicates that female infertility treatments are important for cost containment in health systems ♣