Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Latinoamericana de Bioética
Print version ISSN 1657-4702
rev.latinoam.bioet. vol.15 no.1 Bogotá Jan./June 2015
ARTÍCULO ORIGINAL
DELIRIUM IN AWAKE PATIENTS WITH MECHANICAL VENTILATION IN INTENSIVE CARE UNIT
DELIRIUM EN PACIENTES DESPIERTOS CON VENTILACIÓN MECÁNICA EN LA UNIDAD DE CUIDADO INTENSIVO
DELIRIUM EN DOENTES ACORDADOS COM VENTILAÇÃO MECÂNICA EM UNIDADE DE TERAPIA INTENSIVA
Ángela María Henao Castañoa, María Consuelo Del Pilar Amaya-Reyb
a Doctorate in Nursing, Universidad Nacional de Colombia, Bogotá, Colombia. Self-funded Project, Universidad Nacional de Colombia, 2011. Email address: angmhenaocas@unal.edu.co. Bogotá, Colombia.
b PhD. Full –Emeritus professor, Universidad Nacional de Colombia, Bogotá, Colombia. Doctoral Program. Email address: p_amaya_rey@yahoo.com; mcamayad@unal.edu.co. Bogotá, Colombia.
Fecha de recepción: junio 24 de 2014
Fecha de evaluación: agosto 15 de 2014
Fecha de aceptación: octubre 14 de 2014
RESUMEN
Objetivos: identificar la incidencia de delirium en pacientes despiertos que reciben profilaxis primaria durante la ventilación mecánica en la unidad de cuidados intensivos en la Clínica Palermo, Bogotá-Colombia. Metodología: estudio descriptivo transversal. Se exploró la relación del delirium con la enfermedad médica, la profilaxis primaria, la historia personal y asociación con delirium. El tamaño de la muestra (n = 102) se calculó teniendo en cuenta la frecuencia de pacientes despiertos en ventilación mecánica con una estancia media hospitalaria de 7 días. Análisis estadísticos univariado, bivariado y multivariado. Resultados: el delirium se presentó en 8 de cada 102 pacientes (22 %) se observaron diferencias significativas entre los que deliraron y los que no deliran por edad y Marshall. Relaciones significativas entre el delirium y el Apache II, Tiss 28, y Marshall no se han demostrado a través de la regresión logística. Conclusiones: la edad (más de 60 años) es un factor predisponente para la presencia de delirium, así como los antecedentes de tabaquismo. La administración de medicamentos para la profilaxis primaria no mostró ninguna asociación con la ausencia de delirium en pacientes despiertos en ventilación mecánica en la UCI.
Palabras clave
Delirium, cuidado intensivo, enfermería, respiración artificial.
SUMMARY
Objectives: Identify the incidence of delirium in awake patients who receive primary prophylaxis during mechanical ventilation in the intensive care unit in the Palermo Clinic, Bogota- Colombia. Methodology: Prospective cohort study. This study explored the relationship of delirium with primary prophylaxis, medical illness and personal history The sample size (n = 102) was calculated by taking into account the traced frequency of awake patients on mechanical ventilation with an average hospital stay of 7 days univariate, bivariate, and multivariate statistical analyses. Results: Delirium was presented in 8 out of 102 patients (22 %) significant differences were noted between those who raved and those who did not rave for age and Marshall. Significant relationships among delirium Apache, Tiss 28, and Marshall were not proven via logistic regression. Conclusions: Advance age (over 60 years old) is a predisposing factor for the presence of delirium as well as smoking history. The medication administration in the primary prophylaxis did not show any association with the absence of delirium in awake patients on mechanical ventilation in the ICU.
Keywords
Delirium; Intensive care; Nursing; Artificial respiration.
RESUMO
Objetivos: Identificar a incidência de delirium em pacientes acordados que recebem profilaxia primária durante a ventilação mecânica na unidade de terapia intensiva na Clinica Palermo, Bogotá-Colômbia. Metodologia: Estudo descritivo transversal. Explorou-se a relação do delirium com a doença médica, a profilaxia primária, a história pessoal e associação com delirium. O tamanho da amostra (n = 102) foi calculado tendo em conta a frequência de pacientes acordados em ventilação mecânica com um tempo médio de internação de 7 dias. Análises estatísticas univariadas, bivariadas e multivariadas. Resultados: O delirium se apresentou em 8 de cada 102 pacientes (22%) Se observaram diferenças significativas entre aqueles que deliraram e os que não deliraram pela idade e Marshall. Relações significativas entre delirium e o Apache II, Tiss 28 e Marshall não foram demonstrados por meio de regressão logística. Conclusões: a idade (mais de 60 anos) é um fator predisponente para a presença de delirium e assim como os antecedentes de tabagismo. A administração de medicamentos para profilaxia primária não mostrou associação nenhuma com a ausência de delirium em pacientes acordados em ventilação mecânica na UTI.
Palavras-Chave:
Delirium, cuidados intensivos, enfermaria, respiração artificial.
INTRODUCTION
Delirium is defined as an acute variation of the state of mind with a fluctuating course, characterized by lack of attention and disorganized thought (Bourne, 2008). In patients admitted to the intensive care unit (ICU), delirium is an independent predictor of mortality in patients under mechanical ventilation HR 3.23. 95 % CI 1.4-7.7. p. 0.008 (Wesley et al., 2004) (McCusker, Cole, Abrahamowicz, Primeau, & Belzile, 2002). Delirium has a great importance in the patient care in an intesive care unit. However, permanent, preventive and predictable attention is not always guaranteed. Patients with delirium presented higher mortality in the intensive care unit compared to a rate of non-delirium patients (63,6 % vs. 32,5 %, respectively), with RR of 2.57 (95 % CI 1.56-8.15) (Shu-Min et al., 2004).
The motor subtypes of delirium are classified as: Hyperactive delirium characterized by increased psychomotor function with agitated behavior, or in some cases with aggressiveness, combative and overly alert (Meagher & Hanlon, 2000). Hypoactive delirium presents reduced psychomotor behavior or subjects may appear tranquil and slow, with reduced surveillance, apathetic and often misdiagnosed as depressive or with dementia (Irwin & Rippe, 2002). Mixed delirium ranges between hyperactivity and a manifestation of hypoactivity throughout the day or during course of several days. Both manifestations have been proven common in ICUs.
Two categories of risk factors exist for the presence of delirium (Inouye, Viscol, Horwitz, Hurst & Tinetti, 1993): the first, predisposing factors are those factors with which patients are admitted to the hospital and indicate vulnerability. Among these, there are age over 70 years, antecedents of depression, dementia, epilepsy, prior cerebrovascular disease, treatment with psychoactive substances, alcoholism, and hypo or hypernatremia. Among the medical history antecedents setting the relationship, there are hypertension, alcoholism, history of cigarette smoking, and abnormal levels of bilirubin (Alexander, 2009) (Dubois, Bergeron, Dumont, Dial & Skrobik, 2001). Precipitating factors, that is, those occurring during the stay in the intensive care unit, are secondary to the patient's disease, including the severity of the disease, metabolic disturbances (sodium, calcium, and blood urea nitrogen (BUN) levels), along with infection (Capuzzo et al., 2004), hypoxemia, anemia (Granberg, Malmros, Bergbom & Lundberg, 2002), acidosis, hypotension, and environmental factors in the intensive care unit. Use of epidural anesthesia and morphine are significantly associated to the presence of delirium. Delirium is also manifested with self-extubation, elimination of catheters, prolonged hospital stay, and ventilator dependence in sedated patients (Dubois, Bergeron, Dumont, Dial & Skrobik, 2001)
The importance of cognitive monitoring, besides the physiological constant, is the priority in ICU. Integrity and cognitive recovery of ICU patients is probably as important as the physical recovery if not the most important for patients and families. It is possible to live and adapt to some type of physical disability only with a sane mind or at least at the pre-morbid level of mental function. Every effort must be undertaken to help patients and their families to overcome the negative psychological effects of ICU, particularly within the three principal environments of patients' recollection: procedures, comfort, and the healthcare team (Roberts & Wendy, 2004).
The diagnosis of delirium in awake patients under mechanical ventilation is useful to identify modifiable factors to obtain higher survival rate opportunity (Thomason et al., 2005). Adequate and timely assessment of delirium in patients facilitates empowerment of the nurse in individualized care, which reduces the consequences related to mortality, increased hospitalization days and complications (Bourne, 2008).
From its practice, nursing highlights the importance of psychological recovery in patients in ICU and it is as important as physical recovery. This study puts to the test our hypothesis that the awake patients on mechanical ventilation with primary prophylaxis was associated with a lower presence of delirium during ICU stay that is on average of 7 days.
MATERIALS AND METHODS
The study's sample calculation was 102 patients through non-probabilistic sampling, using the finite population calculation. The following parameters were considered: expected frequency of the parameter is 0.17 as prevalence of delirium reported in ventilated patients in Colombia (Ramos, Perez, Takao & Almanza, 2007), with a 0,05 expected error in a population of 192 awake patients with mechanical ventilation who fulfilled the inclusion criteria during one year, in selected ICUs, with the calculation of N=102 for the sample.
Inclusion criteria: a) informed consent signed by a family member of the patient, b) male or female over 18 years of age, c) hospitalized in the intensive care unit, d) awake patient with mechanical ventilation since the moment of admission until the day of extubation. Exclusion criteria included: a) patients with mechanical ventilation under the effects of deep sedation or coma, b) patients in clinical condition of schizophrenia, encephalopathy, cerebrovascular disease, and clinical history of some type of dementia (Colombo, Corona & Praga, 2012), c) patients in neurosurgery postoperative, severe cranioencephalic (this term does not appear in medical dictionary) trauma, or increased intracranial pressure, Glasgow < 13, and d) pregnant patients.
Another characteristic of the participants in this investigation was the physician-pharmacological management of patients with mechanical ventilation who mostly received antipsychotics such as clozapine, haloperidol and morphine in intermittent dosage. None of the members from the sample received intravenous sedatives or muscle relaxants, which permitted maintaining consciousness; thus, facilitating the implementation of the CAM-ICU to diagnose delirium and the relevance of this study.
The Confusion Assessment Method for ICU (CAM-ICU) was the instrument selected for the study among the tools available for delirium assessment of delirium (Wesley et al., 2001) in the ICU. The CAM-ICU is an instrument validated and recommended by international guides and it permitted detection of delirium with RASS (Richmon Agitation-Sedation Scale) (Wesley & Truman, 2003). Within the psychometric quality of the CAM-ICU criterion validity reports are presented confirmed by the sensitivity and specificity of the test in its cultural adaptation and Spanish version. The translation and cultural adaptation process was carried out according to international recommendations currently in effect; 65 evaluations were conducted in 29 patients. The instrument's internal agreement was adequate, reaching Cronbach's alpha of 0,84 (unilateral 95 % CI: 0,77). Sensitivity of the Spanish version CAM-ICU for observer A (physician) was 80%, with 96% specificity. While for observer B (nurse) sensitivity was 83 %, with 96 % specificity. (Tobar, Romero & Galleguillos, 2010) (Toro, Escobar & Franco, 2010).
The diagnosis of delirium was carried out via the CAM-ICU test, which evaluates the motor response of awake patients with invasive mechanical ventilation, founded on four key criteria of delirium: (a) acutely changed mood, (b) lack of attention, (c) disorganized thought, and (d) altered levels of consciousness. Clinically, delirium is considered present if criteria (a - b and c, d) are manifested (Tobar, Romero & Galleguillos, 2010); the CAM-ICU shows good specificity and validity when applied by nurses and physicians in ICU (McNicoll, Pisani, Wesley, Gifford & Inouye, 2005).
DATA COLLECTION PROCEDURE
Monitoring of delirium was conducted in two phases: 1). A first follow-up (noun), which was comprised from the moment the patient was admitted to ICU fulfilling the study's inclusion criteria capturing antecedents of the record in the clinical history of predisposing factors of hypertension, smoking history and alcohol, motive of admission to ICU; laboratory results (electrolyte-BUN), the variables that were measured during ICU hospitalization included the severity of the disease given by the APACHE (Multiple Organ Dysfunction Score) (Knaus, Draper, Wagner & Zimmerman, 1985) and TISS 28 scales (Simplified Therapeutic Intervention Scoring System) (Miranda, Rijk & Schaufell, 1996), MARSHALL (Multiple Organ Dysfunction Score) (Marshall & Cook, 1995) followed by a second monitoring phase, which diagnoses delirium via CAM - ICU. The presence or absence of delirium was monitored through daily registries during different schedules, three times a day (morning, afternoon, and evening shifts) by the nursing personnel working in ICU and the principal investigator trained to evaluate delirium in patients and their level of consciousness during hospitalization. A format created for said purpose was used during a maximum of seven days of hospitalization. The seven days are an average hospital stay for awake patients with mechanical ventilation in the ICU. The primary prophylaxis for delirium with antipsychotics was also recorded daily for each of the patients and the use of drugs such as clozapine, haloperidol and morphine regardless of the dose. Data was gathered from September 2011 to March 2012 in a private catholic institution offering high-complexity services. The unit has 12 individual beds, each with individualized nursing care. This study was approved by the ethics committee at the Faculty of Nursing in Universidad Nacional de Colombia and at the Palermo Clinic. This study was defined with minimal risk, reflects the principles that reflect the concern of the researcher to do right, good and just and thus lay the ethical principles of non-maleficence, beneficence and justice during the course of the study, are the guidelines on professional ethics, which behave like moral norms, using the informed consent which was signed by the patient family (Ministerio de Salud, República de Colombia, 1993).
DATA ANALYSIS
Analysis of the clinical records of delirium diagnosis was performed for each of the patients studied; thus, managing to identify the behavior of each of the variables. This was accomplished through daily registries during different schedules (morning, afternoon, and evening shifts) for seven days. Data analysis was conducted with the SPSS statistical package version 19, calculating the incidence of delirium for this population. Descriptive analysis was used to determine the presence of delirium in the population; quantitative variables (age, Apache II, TISS 28. Marshall,) were expressed as mean and typical deviation. Qualitative variables were expressed as absolute and relative (%) frequencies (No).
RESULTS
During the study period, 130 patients were admitted to the intensive care unit of which only 102 complied with the inclusion criteria. Sample distribution by gender was 55 % female and 45 % male, mean age was 58 years.
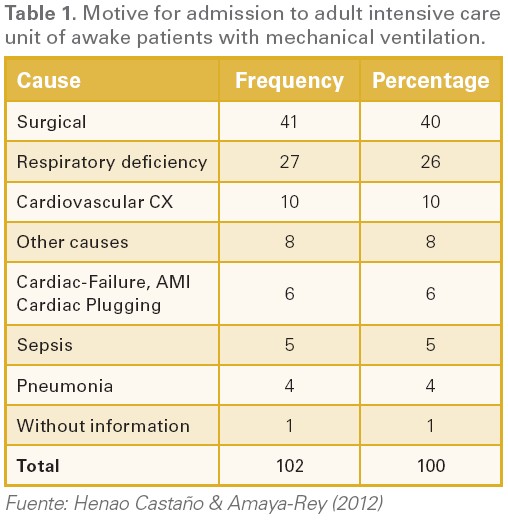
Table 1 presents the description of the motives for admission to ICU of patients prioritizing surgical post-operative admission with 40% (41 cases), followed by respiratory deficiency 26 % (27 cases), sepsis 5 % (5 cases) and pneumonia with 4 % (4 cases). To detect delirium as inclusion criterion, the sample had a level of consciousness evaluated institutionally via a Glasgow scale of 15/15 in 91 % of the patients (93 cases) and a Glasgow scale of 14/15 in 9 % of the patients (9 cases). A fact that permitted the patients to have an adequate motor response (shaking hands with the researcher according to instructions) at the moment of assessing delirium with the CAM-ICU instrument.
The incidence of delirium occurred in 22 patients, that is, in 22 % of the sample of 102 patients, hypoactive delirium 10 %, hyperactive 12 % delirium. Among the personal antecedents of the sample monitored for the presence of delirium while under mechanical ventilation, personal antecedents were found of hypertension with 3408201%, followed by alcoholism at 908201%, and smoking at 708201%. After ascertaining the validation of assumptions of normality according to Konmogorov Smirnof, Table 2 presents Student's t test to evaluate the presence of possible significant differences in the average values among patients with and without delirium events in each of the scales. For the APACHE II (p = 0,060) and TISS 28 (p = 0,618) averages, no significant difference was noted among the averages of patients who presented or did not present delirium. The Marshall scale (p = 0,029) presents a significant difference among averages of patients who presented delirium and those who did not.
Table 3 presents the mean difference significance by age, gender and motive for admission to ICU in patients who had and those who did not have delirium, finding that only age was significant. Likewise, the mean differences were calculated among patients who raved and did not rave by antecedents of hypertension, alcoholism, smoking, administration of morphine and other medications, only finding significance among patients who raved and who did not rave in the smoking factor.
Based on Table 3 and 4: It can be noted that significant values do not exist to infer a possible degree of statistical association among the independent variables, which is why it is concluded that no collinear problems exist among the variables associated to the presence or not of delirium events. Table 4 presents the multiple logistic regression models, which includes the three variables that showed statistical significance.
Upon adjusting a multiple logistic regression model to evaluate the joint effect observed from the MARSHAL score, age and the presence of smoking antecedent on the likelihood of delirium occurrence; it was found -as shown in Table 5- that only age presented a positive effect on the probability of delirium occurrence; specifically, the older the patient, the higher the probability of delirium occurrence (see positive parameter in the table).
Likewise, it is worth noting that smoking and the MARSHAL score were not significantly associated from a multivariate perspective. A probable explanation for this phenomenon is the low number of patients who stated they were smokers (7 of 102), which led to the OR estimated (4451) with 95 % CI (0,708-27.980) not being significant in spite of its high value. Similarly, the slight magnitude of the bivariate association found between the Marshal score and the presence or not of delirium (p = 0,02) could be the cause of no association found from a multivariate perspective. Due to the aforementioned, new studies are suggested that permit increasing the simple size to evaluate the joint effect of the variables studied herein.
CONCLUSIONS
The 22% incidence in the current study of this finding is lower compared with the international data from 60 to 80 % of the presence of delirium (Girard, Pandharipande & Wesley, 2008). The study in Colombia's Central Military Hospital reported delirium incidence at 29 % in critically ill patients with mechanical ventilation who were sedated during mechanical ventilation and with pharmacological treatment with opioids and benzodiazepines (Ramos, Perez, Takao & Almanza, 2007). Also, at the Reina Sofía Clinic in Bogotá, Colombia, found 21 % incidence of patients with delirium, but the difference is that all the patients from these two studies were sedated patients (benzodiazepines and opioids) with mechanical ventilation (Florez & Velasquez, 2009) . It is remarkable that for Colombia the incidence of delirium behaved with a similar intensity in the three studies, while -in contrast- in the United States the incidence of delirium in sedated patients, critically ill patients and in ICUs ranges between 60 and 80 % (Serpa, Nassar & Cardoso, 2012). In two studies, reports that patients studied with this incidence of delirium were sedated with Midazolam, opioids, and propofol (Bourne, 2008), and in another study the patients were sedated with benzodiazepines and meperidine (Girard, Pandharipande & Wesley, 2008). The marked difference among the studies carried out in Colombia with authors mentioned may lead us to think that while in Colombia there may be underreporting due to diagnostic deficiencies, in the United States the formation of an interdisciplinary group to diagnose delirium facilitates early detection and typification of delirium impacting on the incidence reported in that country. Additionally, the state of minimum sedation as a physician management protocol of patients under mechanical ventilation maintains patients awake in contrast with prolonged deep sedation management.
All the awake patients under mechanical ventilation are susceptible to being evaluated for early detection of delirium. The intensive care unit in which this study was conducted, presented advantages to evaluate the presence of delirium in patients under mechanical ventilation, given that they were already awake, permitting application of the test without difficulties in comprehension and rapid administration. In contrast with the studies analyzed, as antecedent and for the present discussion, it is known that the diagnostic tests of delirium occur during the sedation weaning process and detection of delirium is hindered, given that states of deep sedation, stupor, or coma do not permit performing the CAM-ICU test in elderly adults (McNicoll, Pisani, Wesley, Gifford & Inouye, 2005). This diagnostic medium of delirium diagnosis is delayed and only until the moment of ventilatory support weaning and the patient's recovery of consciousness can present motor response to enable application of the CAM-ICU test to diagnose delirium.
The moments to assess delirium in this study were three times per day and upon presenting some type of change in the patient's behavior (hypo or hyperactivity). This decision to monitor delirium was consistent with that recommended by (Zaal & Slooter, 2012). In the literature, most research conducted in ICUs has measured delirium at a given moment during a 24-hour period in the morning, evening and at night and when changes in patient's behavior were suspected for the presence of delirium. Two publications evaluated delirium more than once per day (Pun et al., 2005) (Peterson et al., 2006). However, for this study, several measurements were made, one per shift, because delirium is of acute and fluctuating nature, and the measurements besides being easy and rapid (from one to three minutes) are highly sensitive for detection, given that delirium tends to be underestimated by healthcare teams (Balas et al., 2012).
In this study, data related to sample size (n = 102), incidence of delirium (22 %), and the manner of assessment to detect delirium through the CAM-ICU test, as well as the range of time between day one and day five to detect the presence of delirium is similar to the study in Taiwan (Lin, Liu & Whang, 2004). Both studies report that the sample was with patients in critical state and with mechanical ventilation. The difference between the studies lies in that in the present study all the patients were awake and medicated with clozapine and/or haloperidol and morphine according to pain. In contrast, the patients from the study in a hospital in Taiwan were medicated with high dosages of morphine (50 mg/day) or midazolam (0,09 mg/kg/h). Although the article does not state the number of days the medication was maintained, most likely the patients sedated with these doses cannot be evaluated with the CAM-ICU test. Hence, it is not precisely known what moment is considered day one of the evaluation and the continuity of assessments to detect delirium, to interpret the findings related to the 22 % incidence and the report of delirium between the first day and the fifth day; given the circumstance that the measurement makes us think that it is possibly ventilatory support post-weaning.
Broader research is required with greater coverage of factors to verify predisposing and precipitating factors inside and outside the ICUs with and without sedation during mechanical ventilation and without mechanical ventilation with adults.
Review the literature circumscribed to awake patients under mechanical ventilation or consider the possibility of multi-centered research at the national and international levels to contrast with different places under the same therapeutic management.
LIMITATIONS
The inclusion criteria considered for this study, among which patients had to be without sedation effects or with minimum effects during mechanical ventilation, makes the sample size require greater time to gather data and increase sample size.
The exclusion criteria used for this study may keep some patients from being diagnosed as hypoactive delirium, causing the sample to be underestimated or restricted to Glasgow scores above 13.
Use of prognosis tools like the TISS 28 and Marshall do not easily permit contrasting because literature and the ICU scenarios do not always use them.
Medical clinical management of adult patients predominates in mechanical ventilation with sedation, thereby, not many broad samples are available with critically ill awake patients or patients with minimum sedation under mechanical ventilation.
ACKNOWLEDGMENTS
We thank Alonso Gomez, MD and the Palermo Clinic of Bogota-Colombia for their insights and helpful contributions that guided us in our approach to this manuscript.
We thank the Universidad Nacional de Colombia, Doctoral Program in Nursing for the academic discussions and we are deeply appreciative of the patients and nursing staff who made this study possible.
No conflict of interest Arises. Study self-funded
REFERENCIAS
1. Alexander, E. (2009). Delirium in the intensive care unit: medications as risk factors. Critical Care Nurse, 29(1), 85-87. [ Links ]
2. Balas, M., EE, V., Burke, W., Boehm, L., Pun, B., Olsen, K. & Wesley, E. (2012). Critical care nurses' role in implementing the "ABCDE bundle" into practice. Critical Care Nurse, 32(2), 8-35. [ Links ]
3. Bourne. (2008). Delirium and use of sedation agents in intensive care. Nursing in critical care, 13, 195-202. [ Links ]
4. Capuzzo, M. V., Cingolani, E., De Luca, S., Gianstefani, G., Grassi, L. & Alvisi, R. (2004). Application of the Italian version of the Intensive Care Unit Memory tool in the clinical setting. Critical Care Medicine, 8(1), 48-55. [ Links ]
5. Colombo, R., Corona, F. & Praga, C. (2012). A reorientation strategy for reducing delirium in the critically ill. Results of an interventional study. Minerva Medica, 78(9), 1026-1033. [ Links ]
6. Dubois, M., Bergeron, N., Dumont, M., Dial, S. & Skrobik, Y. (2001). Delirium in an intensive care unit: a study of risk factors. Intensive Care Medicine, 27(8), 1297-304. [ Links ]
7. Florez, P. & Velasquez, J. (2009). Frequency and risk factors for delirium in geriatric population in the intensive care unit of the clinic Queen Sofia of Bogota - Cololmbia. Revista Médica, 12(3), 66-73. [ Links ]
8. Girard, T., Pandharipande, P. & Wesley, E. (2008). Delirium in the intensive care unit. Critical Care Medicine, 12(Suppl 3), 1-9. [ Links ]
9. Granberg, A., Malmros, C., Bergbom, I. & Lundberg, D. (2002). Intensive care unit syndrome/delirium is associated with anemia, drug therapy and duration of ventilation treatment. Acta Anaesthesiol Scand, 46(6), 726-31. [ Links ]
10. Inouye, S., Viscol, i. C., Horwitz, R., Hurst, L. & Tinetti, M. (1993). A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Annals of Internal Medicine., 119(6), 474-81. [ Links ]
11. Henao Castaño, A. M. & Amaya-Rey, M. C. P. (2012). Delirium in mechanically ventilated patients in the ICU: associated factors and nursing care (thesis). [ Links ]
12. Irwin, R. & Rippe, J. (2002). Diagnóstico y tratamiento de la agitación y el delirio en el paciente crítico. En manual de cuidados intensivos (pp. 869-871). Madrid: Marban Libros. [ Links ]
13. Knaus, W., Draper, E., Wagner, D. & Zimmerman, J. (1985). Apache II: A severity of disease classification system. Critical Care Medicine., 13(10), 818-829. [ Links ]
14. Lin, S., Liu, C. & Whang, C. (2004). The impact of delirium on the survival of mechanically ventilated patients. Critical Care Medicine., 32(11), 2254-2259. [ Links ]
15. Marshall, J., & Cook, D. (1995). Multiple Organ Dysfunction Score: A reliable descriptor of a complex clinical outcome. Critical Care Medicine, 23(10), 1638-1652. [ Links ]
16. Ministerio de Salud, República de Colombia. (1993). Resolución 008430 de 1993. Recuperado de http//www.unal.edu/viceinvestigacion/normatividad/etica_res_8430_1993.pdf. [ Links ]
17. McCusker, J., Cole, M., Abrahamowicz, M., Primeau, F. & Belzile, E. (2002). Delirium predicts 12 month mortality. Internal Medicine, 162(4), 457-463. [ Links ]
18. McNicoll, L., Pisani, M., Wesley, E., Gifford, D. & Inouye, S. (2005). Detection of delirium in the intensive care unit: comparison of confusion assessment method for the intensive care unit with confusion assessment method ratings. Journal of the American Geriatrics Society, 53(3), 495-5. [ Links ]
19. Meagher, D. & Hanlon, D. (2000). Relationship between symptoms and motoric subtype of delirium. Journal Neuropsychiatry Clin Neurosci, 12(1), 51-56. [ Links ]
20. Miranda, D., Rijk, A. & Schaufell, W. (1996). Simplified therapeutic intervention scoring system: The TISS_28 items- Results from a multicenter study. Critical Care Medicine, 24(1), 64. [ Links ]
21. Peterson, J., Pun, B., Dittus, R., Thomason, J., Jackson, J., Shintani, A. & Wesley, E. (2006). Delirium and its motoric subtypes: a study of 614 critically ill patients. Journal of the American Geriatrics Society, 54(3), 479-84. [ Links ]
22. Pun, B., Gordon, S., Peterson, J., Shintani, A., Jackson, J., Foss, J. & Wesley, E. (2005). Large-scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centers. Critical Care Medicine, 33(6), 1199-205. [ Links ]
23. Ramos, I., Perez, D., Takao, F. & Almanza, J. (2007). Incidencia de delirio en las unidades intensivo y cuidado coronario del hospital militar central. Revista Neurología, Neurocirugía y Psiquiatría, 40(2), 41-19. [ Links ]
24. Roberts, B., & Wendy, C. (2004). Patients' dreams and unreal experiences following intensive care unit admission. Nursing in Critical Care, 9(4), 173-179. [ Links ]
25. Serpa, A., Nassar, A., & Cardoso, S. (2012). Delirium screening in critically ill patients: A systematic review and meta-analysis. Crirtical Care Medicine, 40(6), 1946-1951. [ Links ]
26. Shu-Min, L., Chien-Ying, L., Chun-Hua, W., Horng-Chyuan, L., Chien-Da, H., Pei-Yao, H. & Han-Pin, K. (2004). The impact of delirium on the survival of mechanically ventilated patients. Critical Care Medicine, 32(11), 2254-2259. [ Links ]
27. Thomason, J., Shintani, A., Peterson, J., Pun, B., Jackson, J. & Wesley, E. (2005). Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Critical Care Medicine, 9(4), 375-81. [ Links ]
28. Tobar, E., Romero, C., & Galleguillos, T. (2010). Método de Evaluación de la confusión en el diagnóstico de delirio en los pacientes de la UCI (CAM-ICU): adaptación cultural y validación de la versión española. Medicina Intensiva, 34(1), 4-13. [ Links ]
29. Toro, A., Escobar, L., & Franco, J. (2010). Spanish version of the CAM-ICU (Confusion Assessment Method for the Intensive Care Unit). Pilot study of validation. Medicina Intensiva, 34(1), 14-21. [ Links ]
30. Wesley, E., & Truman, B. (2003). Monitoring sedation status over time in ICU patients. Realibility and validity of the Richmon Agitation-Sedation Scale (RASS). JAMA, Internal Medicine, 289(22), 2983-2991. [ Links ]
31. Wesley, E., Margolin, R., Francis, J., May, L., Truman, B., Dittus, R. & Inouye, S. (2001). Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Critical Care Medicine, 29(7), 9-1370. [ Links ]
32. Wesley, E., Shintani, A., Truman, B., Sperof, T., Gordon, S., Harrel, F. & Dittus, R. (2004). Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA, Internal Medicine, 291, 1753-1762. [ Links ]
33. Zaal, I. & Slooter, A. (2012). Delirium in critically ill patients. Epidemiologya, pathophysiologya, diagnosis and management. Drugs, 72(11), 1457-1471. [ Links ]













