Introduction
Critically ill pediatric patients whose spontaneous ventilations are inadequate to maintain life will be put on mechanical ventilators. While a mechanical ventilator assists children's respiratory efforts, it renders them unable to express their needs and feelings verbally 1. Patients' difficulty in verbal communication causes the nursing staff and the caregivers, as well as the patients themselves, to become exhausted and discouraged 2; finally, the patients are left without communication, leading to stress. In general, mechanically ventilated patients require augmentative and alternative communication (AAC) tools and strategies to facilitate communication 3. AAC includes all forms of communication, except oral speech, that are used to express message; its types included unaided systems (e.g., gestures, facial expressions, and sign language) and aided systems (e.g., pen and paper, letter/picture boards) 4 are usually used as the regular communication methods with children on mechanical ventilators.
Even though these methods aid the communication between the patients and their communication partners, the limitations from being under mechanical ventilators, together with the illness severity, often decrease the efficiency of the communication. The loss of two-way communication can affect the patients' mental health greatly. Previous studies revealed that severe emotional reactions among mechanically ventilated patients - such as frustration, disconnection, helpless, stress, anxiety, and fear - could arise 5-7. These adverse emotional reactions also happened with caregivers and nursing staff due to their inability to comprehend the patient's needs and feelings, and a limited competence to find strategies to facilitate communication 7-9.
The communication difficulties with mechanically ventilated patients have been improved by the use of assistive communication devices that are available for both adult and pediatric patients. These devices include communication cards 10, a text-illustrated communication board 11, a communication board 12-13, an electronic communication device 14, an electronic voice-output communication aids 15, and a handheld computer device 16, for example. However, these devices still carry some limitations, including insufficient information about needs and requirements of the patient, poor device positioning, discomfort during the use of device, for example 17.
In the current Digital Age, communication technology is much more advanced. Tablets are one of the most popular and friendly-use communication devices with users across all age groups, even among nurses and other health professionals 18. There are many tablet applications, either paid or free, available to aid communication among pediatric patients, nursing staff, and care-givers 19; however, the free communication applications available have a limitation for use with Thai population because most of the applications were developed in English.
In Thailand, the assistive communication devices are for outdated operation technology, and there is no current tablet application for use to communicate with pediatric patients on mechanical ventilators. Thus, the researchers became interested in developing "My Voice Board," a tablet application running on the Android operating system, with the purpose of enhancing effective communication between pediatric patients on mechanical ventilators and nursing staff, as well as caregivers. This study was conducted with the purpose of examining the effect of using the "My Voice Board" tablet application on communication satisfaction of nursing staff and caregivers, as well as the satisfaction of pediatric patients with the use of the application. The hypotheses of this study were: 1) Nursing staff had greater communication satisfaction when using My Voice Board to communicate with pediatric patients, compared to the use of regular communication methods; 2) Caregivers who used My Voice Board to communicate with pediatric patients had greater communication satisfaction than those who used regular communication methods.
Conceptual Framework
The Osgood and Schramm Circular Model of communication 20 was used as a conceptual framework of the study. According to the model, communication is viewed as a circular, rather than linear, process that takes place between a sender (encoder) and a receiver (decoder). When the message is transmitted and reaches the receiver, his responsibility is to understand or decode what the sender wants to convey and provide feedback to the (previous) sender. This model was selected because communicating effectively with mechanically ventilated patients is essential for their care. Communication between nursing staff/caregivers and patients must be a two-way process, so the needs and feeings of both parties are not only conveyed, but also understood, and responded to. Effective communication is particularly challenging with pediatric patients. Therefore, in this study, the model was adapted by integrating a user-friendly tablet application (My Voice Board) to facilitate communication.
Methods
Design
The study was a quasi-experimental research. In this study, the one-group pretest-posttest design was implemented with nursing staff, and nonequivalent pretest-posttest control group design was used with caregiver-patient dyads.
Participants
Convenience sampling was used to recruit nursing staff and caregiver-pediatric patient dyads from two intensive care units (ICUs) of a hospital located in Bangkok, Thailand. Due to a limited number of eligible pediatric patients, caregiver-pediatric patient dyads from an ICU of a second hospital located in vicinity were also recruited. These pediatric ICUs encouraged caregivers to visit, but they could only visit four hours each day. During visit, simple assistive communication tools (such as paper and pencil) may be provided if requested. Eligible nursing staff in the study included professional nurses and practical nurses (assistant nurses with one year of training) who were able to use a smartphone/tablet. Eligible caregivers had to take care of their children retaining ventilators for at least two days, be literate, and be able to use a smartphone/tablet. Among the inclusion criteria for the pediatric patients were those who were literate and receiving either continuous noninvasive or invasive ventilators with Glasgow coma scores of 10T.
In this study, all of the nursing staff in the ICUs (N = 51) were invited to participate in the study, and 44 (86%) agreed. For the sample size of caregivers, a power analysis via G*Power program using the large effect size from a previous study 16 with alpha set at .05 and power of .80 was performed to determine the number of caregiver-pediatric patient dyads. Finally, 18 dyads of caregivers and pediatric patients were included in the study; that is, 9 pairs in the control group and the other 9 pairs in the intervention group.
Instruments
The My Voice Board tablet application was developed by the researchers on ASUS ZenPad C7.0 tablet operating on android system version 5.0 (Lollipop). The tablet came with a 7.00-inch display, a dimension of 189.00 x 109.00 x 8.40 (height x width x thickness in millimeters) and the weight of 265.00 grams. It was powered by a 3450 mAh battery. Its ROM and RAM were 16 GB and 1 GB, respectively.
Based on the literature reviews and associated documents, 53 messages were developed by the researchers to indicate the problems and needs of critically ill pediatric patients. The messages were classified into four main menus of needs, feelings, questions, and emergency requests, all of which were also composedof submenus as follows.
Needs, including six submenus: food and water, excretion, changing position, breathing, hygiene, and relaxation;
Feelings, including two submenus: physical and psychological;
Questions, including three submenus: questions about parents, physical well-being or symptoms, and time;
Emergency, consisting of three messages: severe pain, dyspnea, and nausea/vomiting.
The messages for the My Voice Board application were validated for appropriateness and congruency among pictures, sounds and words used by three content experts in the field of media and communication and nursing profession, plus six children (8-14 years of age), and their caregivers. This process was repeated until 100% consensus was obtained.
To use the My Voice Board application for communication, a user can use his/her fingers to control the touch screen. First, the user should select the patient's sex by tapping the gender button so that the pictures and voice will correspond to the child' gender. Next, the user taps on a selected menu, from which he/she can access the submenus. The user can slide a finger up and down the screen to go through the list of submenus. Tapping a selected submenu, the user will see different images accompanied with text messages showcasing the application. When a picture with text message that the patient wants to convey is tapped, the selected message will be transformed into voice to indicate the patient's needs. The user can press the home button at any time to go back to the primary home screen. The users could be nurses, caregivers, and even the pediatric patients. Figure 1 displays the My Voice Board tablet application.
Figure 1 showed a main menu of the My Feelings menu with, for example, four windows of pictures saying, "I feel thirsty," "I feel hungry," "I didn't sleep well," and "It's noisy" (from left to right and down). The bottom shows the other three main menus (i.e., My Needs, My Questions, Emergency), and a Home Menu symbol.
The data collecting instruments included:
The Personal Information Form, which consisted of 8 items asking nursing staff and caregivers about their gender, age, position, education, years of experience in the care of children with ventilators, regular communication methods, problems faced when communicating with the children, and experience in use of applications on a tablet.
The Communication Satisfaction Scaleconsisted of 10 items asking nursing staff and caregivers how satisfied they felt with the communication in terms of, for example, understanding the patients' problems, feelings, and needs; response to patients' needs; explicitness of message sent/received; and increase of participation in care for patients. The response scale ranged from 1 (least satisfied) to 5 (extremely satisfied) and yielded the total scores ranging from 10-50; the higher the total scores, the more satisfaction in the communication. Validated by the three content experts, the content validity index (CVI) of this questionnaire in the current study was .91, and Cronbach's alpha coefficients were .88 and .91 when tested with nursing staff and caregivers, respectively.
The Suitability for Use Scaleconsisted of 18 items asking nursing staff's and caregivers' opinions about the suitability of the My Voice Board application for use as a communication aid. The suitability was measured in terms of content (including categories of needs, clear statement and picture, sufficient number of statements representing basic needs and feelings, synchronization of statements, pictures, and voice), design (including simplicity for use, appropriateness of font, pictures, and voice in terms of size, color, and clarity), and device (including weight, size, and mobility). The response scale ranged from 1 (strongly disagree) to 5 (strongly agree) and yielded total scores ranging from 18 to 90. To ease the interpretation, the total scores divided by the number of items gave the average scores ranging from 1 to 5; the higher average scores, the more suitability for use of the application. Validated by the three content experts, the CVI of this questionnaire in the current study was 1.00.
The Pediatric Patient's Satisfaction Questionnairewas a single item measure asking if the child was satisfied with the use of the My Voice Board application for aiding their communication during mechanical ventilation. The answer was a rating scale ranging from 1 (least satisfactory) to 5 (extremely satisfactory); the higher scores, the more satisfied the child was.
Intervention and data collection
Intervention and data collection were performed between October 2016 and August 2017 with the following groups of participants.
Nursing staff
Prior to the implementation of the intervention among nursing staff, they were required to answer: 1) the Personal Information Form, and 2) the Communication Satisfaction Scale (pretest); in this step, the respondents' satisfaction was based on the regular methods they used to communicate with ventilated patients. Then, the researcher (CT) demonstrated how to use My Voice Board for communicating with the patients. All the nursing staff demonstrated the use of all messaging functions in the application under the researcher's supervision to ensure that they were able to use it correctly. They were allowed to use the application with patients for seven consecutive days because this timeframe would allow all nurses in the study units to be able to use the tablet with patients. Afterward, the nursing staff completed the Communication Satisfaction Scale again (post-test); in this step, their responses were based on their satisfaction after using the application. In addition, their opinions regarding the suitability of My Voice Board for use as a communication aid were also collected via the Suitability for Use Scale.
Caregivers
The implementation of the experiment among caregivers and their children started with the control group, specifically those who used regular communication with the patients. Upon their consent to be the study participants, the caregivers were required to answer 1) the Personal Information Form, and 2) the Communication Satisfaction Scale (pretest). Then, they were allowed to take care of and communicate with their children as usual for two consecutive days. Afterward, the caregivers completed the Communication Satisfaction Scale again (post-test). Upon completing the data collection in the control group, caregivers in the experimental group were required to complete the Personal Information Form and the Communication Satisfaction Scale. Then, the researcher demonstrated how to use the My Voice Board application for communicating with their children. All caregivers demonstrated the use of all messaging functions in the application under the researcher's supervision to ensure that they were able to use it correctly. Mostly, patients were weaned by 3-5 days; thus, the caregivers in this study were allowed to use the application with the patients for two consecutive days. During this period, the nursing staff could be of further assistance, if needed, to the caregivers regarding the use of application. Afterwards, they were asked to complete the Communication Satisfaction Scale again. Their opinions regarding the suitability of the application for use as a communication aid were also collected via the Suitability for Use Scale.
Pediatric patients
Personal information of the pediatric patients about age, sex, education, medical diagnosis, type of ventilator used, duration on ventilator, and intravenous sedation was collected from medical records. This study did not investigate the difference of communication satisfaction between ventilated pediatric patients who used the application and those who used the conventional methods of communication. Basically, patients in ICUs are critically ill and sedated, and therefore it might not be appropriate to ask them a set of questions during such time. Thus, after weaning from ventilators, only the patients in the experimental group were asked to rate their satisfaction towards the use of My Voice Board.
Statistical Analysis
The comparison of communication satisfaction scores in the nursing staff group between prior to and after the use of tablet intervention was assessed using paired t-test. Due to the small sample size of caregivers in both control and experimental groups, the Mann-Whitney U test was used to analyze and compare the communication satisfaction scores between before and after the intervention in both groups.
Ethics
The ethical consideration of this study was approved by the institutional review boards of the study hospitals (COA-Si 559/2016 and COA-RBHEC 009/2017).
Results
Nursing staff
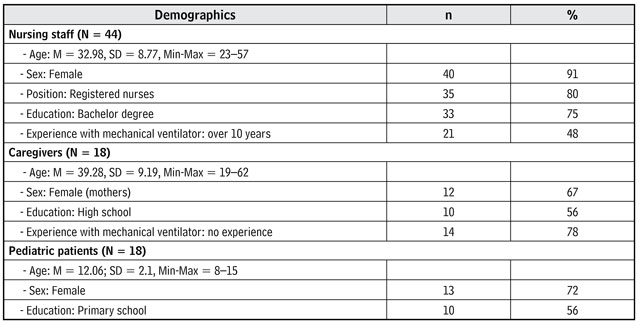
The sample group of this study consisted of 44 nursing staff. Table 1 contained their demographic data. The top three regular communication methods used were lip reading (91%), asking yes-no questions (75%), and gesturing (73%). The top three communication problems with pediatric patients being on mechanical ventilators were: being unable to understand the message through lip reading (93%), being unable to comprehend patient's gestures (86%), and time-consuming of communication (75%). About half of them (52%) never used tablets before.
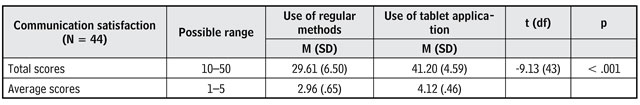
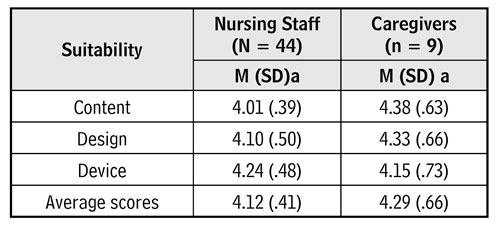
As shown in Table 2, the nursing staff reported more communication satisfaction with the use of the My Voice Board application, compared to the use of regular communication methods(p< .001). The results shown in Table 4 revealed that mean scores of their agreement on the suitability of the tablet application was 4.12 and varied between 4.01 and 4.24 for its content, design, and device. According to the findings, nursing staff mostly agreed that My Voice Board was suitable as a communication aid for use with pediatric patients on mechanical ventilators.
Caregivers
There were 18 caregivers in this study.Table 1 contained their demographic data. The caregivers in both control and intervention groups did not have a significant difference in these personal characteristics. The main regular methods used to communicate with their sick children being on ventilators were: talking directly to the child (89%), using yes-no questions (50%), observing the child's facial expressions (72%), and lip reading (67%). The top three communication problems when these methods were used to communicate with their child were: being unable to understand what the child tried to convey (78%), being unable to understand the child through lip reading (67%) and time-consuming communication (61%). Every caregiver knew how to use the applications on the tablets.
As shown in Table 3, caregivers in the intervention group who used My Voice Board to communicate with their children exhibited significantly higher communication satisfaction than those in the control group who used the regular communication methods(t=-9.13,df= 43,p< .001) (Table 3). Whereas, prior to the study, both groups had shown the same level of satisfaction from regular methods used for communication (p > 0.05).
Table 3 Comparison of communication satisfaction scores between the control and intervention groups
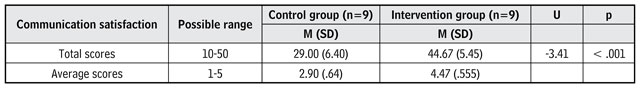
Source: Own elaboration.
As shown in Table 4, caregivers also evaluated the suitability of the tablet application. The mean scores of their agreement on the suitability of the tablet application was 4.29 and varied between 4.15 and 4.38 for its content, design, and device. The findings indicated that the My Voice Board application was suitable as a communication aid for use with pediatric patients on mechanical ventilators.
Pediatric patients
There were 18 pediatric patients in this study. Table 1 contained their demographic data. In addition, nearly 30% of them were diagnosed with autoimmune diseases, followed by 17% with respiratory diseases, and 17% with urological diseases. Seventy-two percent of them were ventilated with endotracheal tube and 28% with BiPap; 78% of the pediatric patients were on first-time ventilators. The duration of mechanical ventilators used among the study patients ranged from 4 to 9 days (M = 5, SD = 1.37), and 61% of them received intravenous sedation while they were on the ventilators. The pediatric patients in both the control and intervention groups did not significantly differ in the aforementioned characteristics (p > .05).
Eight out of nine pediatric patients using the My Voice Board application rated the highest scores, or 5, for their satisfaction with the use of the application, resulting in average satisfaction scores of 4.89 (SD = .33).
Discussion
The study results supported the first hypothesis-that is, nursing staff had greater communication satisfaction with the use of the My Voice Board application, compared to the use of regular methods of communication. The reason why the My Voice Board application obtained more satisfaction may be due to its user-friendly design as well as the sufficient coverage of needs and feelings illustrated for communication with this group of patients; the application was evidently supportive, as shown by the nursing staff's agreement of its suitability for use. Based on previous findings 12,13,16,21 when patients' needs were quicker and more explicitly expressed via an effective communication device, there was no doubt that their needs and feelings would be responded to, leading to compliance and participation towards the treatment and care received. According to the findings from a previous systematic review 17, the regular communication methods (i.e., lip reading, asking yes-no questions, and gesturing) mostly used by nursing staff were not only inadequate to understand the pediatric patients' needs but they were also time consuming and frustrating for both patients and nursing staff. Thus, it was not surprising why communication satisfaction of the nursing staff increased when they had a more effective and modern communication method. Similar to a previous study that emphasized the essential role of nurses to develop effective communication strategy used with pediatric patients to promote patient/parent engagement and satisfaction 22-23. The findings of this study were significant in demonstrating how nurse communication can be improved though a modern and simple device.
The results of the study also supported the second hypothesis that caregivers who used the My Voice Board application to communicate with their mechanically ventilated children had greater communication satisfaction than those who used regular methods of communication. The possible reason could be explained by the same logic as why the nursing staff was more satisfied-namely, that the application on a tablet, an effective communication aid, made it easier for them to communicate with their mechanically ventilated patients through its user-friendly design, as well as the sufficient coverage of needs and feelings shown in the statements and pictures. Based on these findings, the My Voice Board application could be one solution to many of the existing issues with conventional methods of communication. The application might help bringing the caregivers and the patients to a common understanding with ease because it facilitates two-way communication.
Even though the study results support the implementation of the My Voice Board application, as one AAC method, in communicating with this group of patients, the wise use of conventional methods is also important. It is noteworthy that talking directly to the patients was mostly used by the caregivers as a regular communication method, while a better method, yes-no questions, was used by only half of them. Talking to the patients directly was a form of one-way communication conveying only the caregivers' needs rather than receiving and perceiving the patients' needs and feelings. This finding from the current study did confirm that the caregivers were unprepared for the communication difficulties with their critically ill. Previous studies revealed that the presence of family members could lighten the patients' adverse experiences of being on mechanical ventilators 24 and communication of the patients with their family members influenced their psychological well-being 25 that would help to improve quality of care. The caregivers in the current study should be advised on how to communicate with their ventilated children.
The comparison of the pediatric patients' communication satisfaction between the usages of regular methods and the My Voice Board application was not analyzed because most critically ill patients were sedated and required rest, and thus it might not be appropriate to interview them during that time. After weaning, most patients might have little memory of their experience during mechanical ventilation 26, and therefore the communication satisfaction assessed from the pediatric patients' recall may not be reliable. In the current study, satisfaction with the use of My Voice Board rated on one single item was assessed among the pediatric patients in the intervention group only. All of them, except one patient, gave the highest score, 5, about their level of satisfaction with the use of the application. Findings did confirm the effectiveness of the application on tablet for improving the communication during mechanical ventilation, but it is not known what the children in the control group thought.
This was a preliminary study aimed to develop a tablet application, My Voice Board, and to examine the nursing staff's and caregivers' communication satisfaction with pediatric patients on ventilators when using the application. The interpretation of the study findings should be cautious due to its certain limitations. First, the study did not use random samples, and thus, the study sample was not a good representative of the population. Second, selection bias could arise because the subjects were not randomized to the study groups, this means, the caregiver subjects were divided into two groups: Application user VS. Application non-user. The researchers did not randomly assign them to the groups. They completed the first group and then started with the second.
Conclusions and Recommendations
An innovative My Voice Board application was developed and used in a clinical nursing context to facilitate communication between nursing staff/caregivers and pediatric patients on mechanical ventilators who could not verbally and explicitly communicate to others as usual. The study findings indicated that My Voice Board worked effectively, resulting in greater communication satisfaction among the users. Due to its user-friendly design on a modern device with a comprehensive message representing the needs of the patients, the nursing staff and caregivers strongly agreed that My Voice Board was suitable for use as a communication aid.
Thus, the My Voice Board application should be encouraged as one of the assistive communication devices for use with pediatric patients who have speaking difficulties due to their need for mechanical ventilation. This application could be used in ICUs and with home care of mechanically ventilated pediatric patients. However, pediatric nurses should firstly assess the patient and the caregiver communication potentials and, then, select an alternative communication method that fits their potential and conditions. A combination of various communication methods and useful assistive tools like My Voice Board is also advised due to the strengths of each method.
In addition, the My Voice Board application is a preliminary innovative communication device, and its functions need further development. For example, users should be able to add up new vocabulary and message statements representing the patients' specific needs to the message inventory of the application. Further and continuing development of this tablet application is essential so that its function will be up-to-date with the modern technology.