Introduction
Clinical situations exist in which nursing professionals have a clear opinion of what is the morally correct course of an action, but the institutional or hierarchical structure often keeps them from deciding what should be their own moral actions; this experience is what Jameton denominates moral distress 1. Distress is something different from fear or uncertainty, given that it is related with the experience of freedom as possibility, that is, the faculty an individual has to act freely 2. Nursing professionals, as moral agents, have the possibility of choosing to do what is correct, but their election can be restricted by something external or internal, which generates in them a sense of powerlessness when not being able to act correctly 3. Hence, moral distress appears.
Literature describes moral distress as a current and important problem that affects patients in different health systems 4-7. This phenomenon has been explored in the area of critical care 8-10 and has been described as a threat to the integrity of the nurses, as well as to the quality of patient care 11. Studying it is an opportunity to transform moral distress into moral resilience and to help nurses, and other health providers, to mitigate its effects, improve the ethical environment of the practice and quality in care 12.
The concept of moral distress has been discussed by different authors 3,11,13,14, who are critical of the way this problem has been researched, given that errors have been detected in the objectives of the studies, as well as in the operationalization of the concept itself 14. Some suggest that research should focus on improving the quality of the moral decision, moral conduct, among others 11. However, recent studies propose rethinking the way it is being investigated and suggest that it is an opportunity to address its causes, its development, and its moral foundations 15.
Within the literature, the work by Barlem and Ramos 3 stands out, proposing a conceptual model (Figure 1) that explains the emergence and manifestations of moral distress. This model has as central point the moral deliberation process, which is an ethical approach where dialogue seeks to discuss rationally and reflect critically to reach an agreement 3. The deliberation process and the moral sensitivity permit seeing moral problems that could remain hidden and, therein, discuss the possible solutions or ways of coping with them within the health staff. In addition, the authors establish that multiple micro-spaces of power exist in which health professionals perform and develop their relational dynamics 3.
In the oncology area, this is a growing phenomenon with health staff caring for cancer patients 16-21. Among the motives for the emergence of moral distress in this area, ethical conflicts are highlighted associated with the use of advanced technology, both in relation with caring for patients, as with the treatments, entailing ethical challenges for nurses 18,22,23, which are derived from the complex clinical situations they experience next to their patients. Due to the aforementioned, this literature review describes the factors that influence upon the emergence of moral distress in oncology nurses.
Methodology
The review was developed from the six stages proposed by Ganong 24:
Guiding question: What are the factors that influence upon the emergence of moral distress in oncology nurses? The search used key words in English: Moral distress, oncology nursing and their similes in Spanish.
Inclusion criteria: Articles, editorials and reflections related with moral distress in the area of oncology nursing. No restriction was applied for years of publication, given that it is a new theme of which no literature review was found encompassing the objective of this work. The study included articles in Spanish, English, and Portuguese and excluded those that do not address the phenomenon of moral distress explicitly or which were not related with oncology nursing.
The data were obtained from the databases Web of Science, EBSCO (CINAHL), Proquest Central, Pubmed, and PsycInfo, between August and December 2017. From the key words established in the different databases, 177 registries were found; both researchers selected the articles according to the title and abstract, and discriminated them from the objective of the document, and in contrast with the initial question of the review. Those not related with moral distress in oncology were excluded, as well as those from the area of palliative care and whose theme was clinical research, for a total of 38 registries (139 eliminated); and the duplicated registries (20 eliminated), for a total of 18 selected (Figure 2).
Each of the 18 articles selected was subjected to a critical reading using a process of abstraction, synthesis, and data analysis from the guide questions (Chart 1) to synthesize the information collected on moral distress in the area of nursing oncology. In this process, the reviewers agreed on eliminating an article that did not deal specifically with moral distress; thus, leaving a total of 17 registries for this review. Both reviewers extracted from each of the articles the information corresponding to the factors that influence upon the emergence of moral distress and gathered this information into themes or subcategories that group the factors that influence -both favorably and unfavorably- the emergence of moral distress; in turn, this information was classified into three large categories (Figure 3). 5
To introduce the results, each of the categories was described according to the findings in the articles, and to discuss the results, the results obtained were contrasted and integrated with the model by Barlem and Ramos 3, when comparing the elements present in said model with the findings from this review, creating a new matrix to understand the phenomenon of moral distress in the area of oncology nursing (Figure 4).
Results
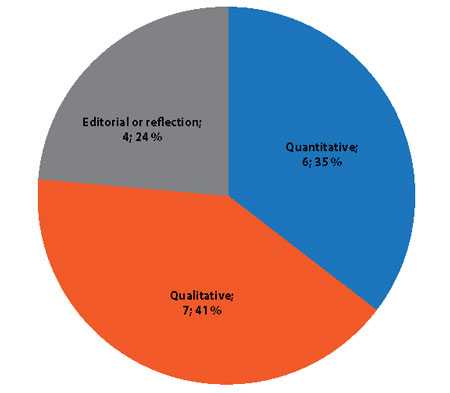
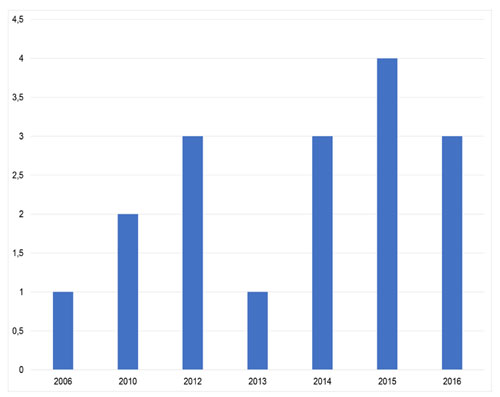
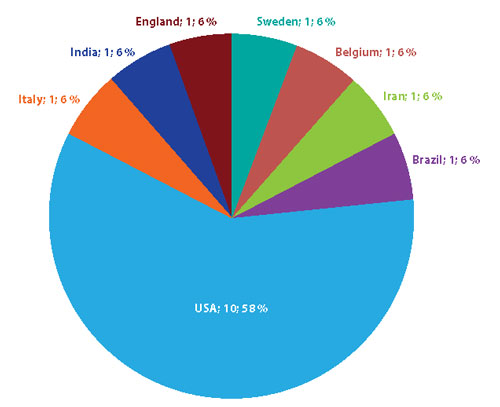
Of the 17 articles selected for this review, seven corresponded to qualitative studies 22,23,26-30; six to quantitative studies 16,31-35; two were reflections 36,37; and two were editorials 17,18 (Figure 3). Eighteen percent of the articles were published between 2006 and 2011, and 82% between 2012 and 2016 (Figure 4). The studies were conducted in different countries: most of them from the United States and the rest from Europe, South America, and Asia (Figure 5).
Quantitative studies used the instrument Moral Distress Scale (MDS) 34 or the version Moral Distress Scale - Revised (MDS-R) 31,35 to measure moral distress in nurses from the oncology area. Another study used the pediatric version of the MDS (MDS-PV): the items in this scale differ from the MDS only in reference to pediatric subjects instead of adults 33.
Table 1 Articles found in the literature on moral distress in oncology nursing
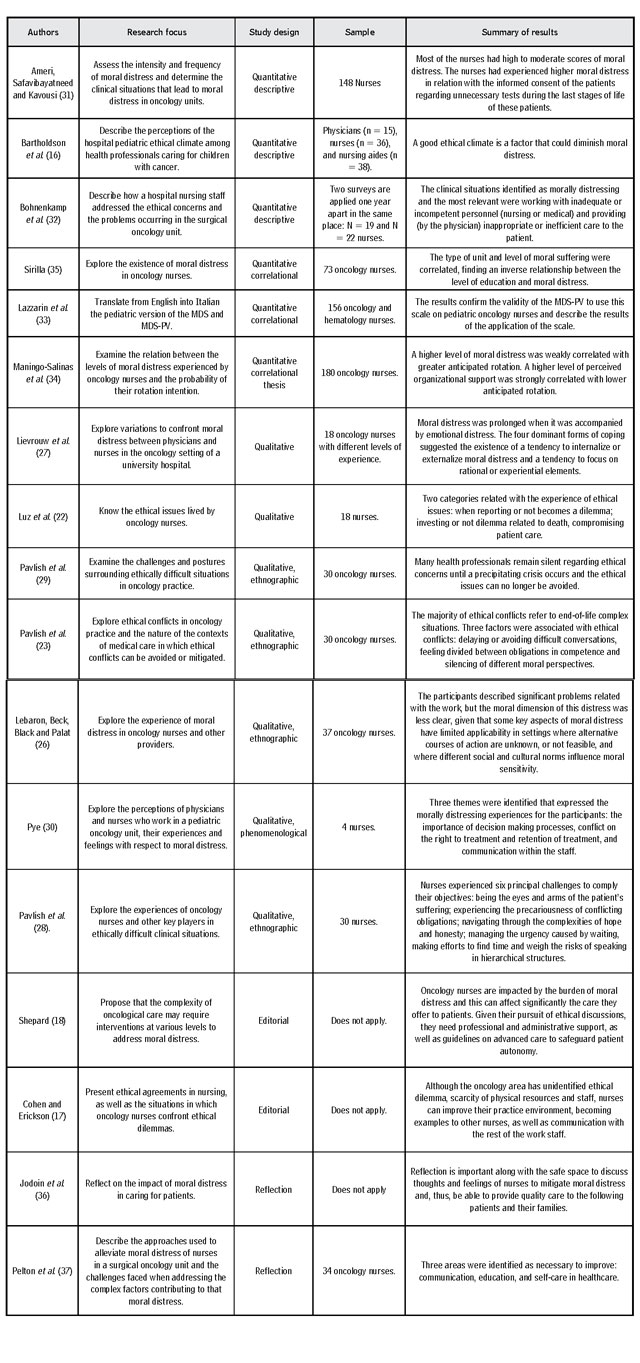
Source: Own elaboration.
From the critical analysis of the articles selected, it was possible to establish the factors that, according to the literature, favor the emergence of moral distress in oncology nurses (Table 2).
Table 2 Factors influencing upon the emergence of moral distress in oncology nurses found in the integrative review
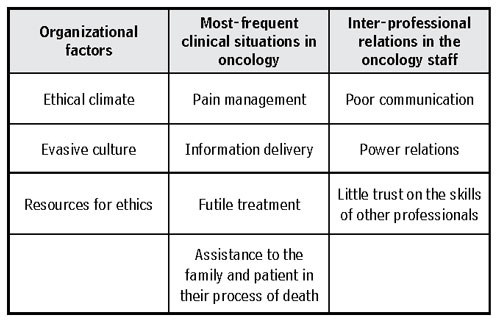
Source: Own elaboration.
Organizational factors
Ethical climate
Ethical climate refers to those factors in an organization that contribute to the skills of health professionals to identify and deal with ethical issues to provide adequate ethical care 16. A poor ethical climate is described as a trigger of moral distress in physicians and nurses in oncology units and affects inter-professional interaction 16. Likewise, Pavlish et al., point to the need to develop health systems in moral communities where all the members are urged to clear their ethical concerns and to deal with them in a way that promotes trust, shared understanding, and mutual respect 23. The study by Bartholdson et al., on ethical climate shows that a lower percentage of the participants reported having the necessary tools to solve ethical issues, as well as time for reflection and discussion when there were ethical conflicts related with the treatment and care.
According to Maningo-Salinas et al., health staff leaders could influence positively on the inquest of the phenomenon of moral distress in nursing professionals, upon recognizing the situations that produce moral distress 34 and when becoming aware of the impact this phenomenon can have on the team 27. Similarly, Jodoin et al., highlight the importance of creating an ethical climate; one of the useful strategies in their unit is the creation of ethical rounds 36.
Evasive culture to deal with difficult ethical issues
According to Pavlish et al., ethical conflicts in oncology are caused by delaying or avoiding difficult conversations about the poor prognosis of the patient or about the end-of-life care. In another study by the same author 29, nurses and other health providers state that ethical questions can damage relations with patients, relatives, and colleagues, which is why they avoid talking about such. The authors found that many health professionals remain silent about ethical concerns until a precipitating crisis occurs, where these matters can no longer be avoided 29.
Resources for ethics
Lack of resources for ethics, like participation in specialized programs, funding for follow-up, and time for discussion also influence on the emergence of moral distress 17,27,37. Cohen and Erickson propose that the lack of recognition of the ethical dilemma and their appropriate discussion in the team lead to having moral distress; upon this, Sirilla adds that it is necessary to analyze the ethical problem through theoretical approaches that guide nurses 35.
In the study by Pelton et al., nurses and physicians established key words that allowed them to communicate when they disagreed, for example, with respect to a physician’s care plan. When these words were mentioned, a discussion was begun in that respect; thus, the physician reported how decisions were made in light of different processes of the disease, and this permitted the nurses to understand the steps of the treatment to facilitate their care role. Additionally, in this study, the participants worked in inter-professional groups, developing solutions for stressing factors in the unit, and this allowed them an emotional bond to open communication opportunities 37.
Training in ethics and in coping with death can benefit nurses by increasing their self-trust in their knowledge about the end of life and on their awareness with respect to moral distress 35. Sirilla recommends starting education during the initial orientation of the practice to ensure that all nurses are aware of the signs and consequences of moral distress 35.
Lack of time is another resource revealed as a general concern in nurses when dealing with ethical issues. Not addressing the ethical issues related with the treatment and care can trigger moral distress 16. Communication, reflection, and discussion of ethical issues in specific clinical situations allow the opinions to be heard of all the members involved, and this could contribute to better ethical climate in oncology 16,27.
Furthermore, the existence of support groups for the nursing professionals, comprised by other colleagues, can facilitate discussion of difficult cases, provide support and, thus, reduce moral distress 18. The same study suggests that rotation of complex patients may be useful to diminish the individual burden of moral distress 18.
Complex clinical situations
In the area of oncology, complex clinical situations exist in which ethical aspects arise that have been widely discussed in the literature and which are a common place of current bioethics.
Pain management
It is a complex situation that causes ethical conflicts among health professionals 34. In diverse studies, participants report that, on occasion, discrepancies exist among the team members with respect to the doses of analgesics that should be administered to a patient 29,33,34. They also indicate that they must follow medical indications that are not aimed at controlling the patient’s pain; thereby, this need is postponed 32. Inadequate management of pain is consequential of patient suffering, which can be a source of moral distress for nurses 26, given that providing inadequate care to patients interferes with the good development of their role, which is related with a high intensity of moral distress in these professionals 31.
Pain management is also influenced by cultural aspects: the study conducted by Lebaron et al., in India shows that nurses endure moral distress because they cannot manage their patients’ pain due to scarce resources and administrative barriers, which keeps them from acting as they believe is best for patients.
Information delivery
Oncology patients are subjected to multiple diagnostic and therapeutic procedures for which it is necessary to obtain informed consent from the patients or their families. On some occasions, nursing professionals feel they must ignore situations in which patients have no adequate information that ensures a correct process of informed consent 22,33,38.
The study by Luz et al., shows that several of the ethical issues are related with the transmission of information and orientation to patients in relation to their disease 22. Reporting or not to patients and to their relatives is one of the principal ethical dilemmas experienced by nurses, and this can be potentiated by the family’s difficulty in perceiving the information 22,23. Oncology patients have doubts about the diagnosis and medical prognosis of the cancer, and that makes nurses act as links between them and other members of the health staff to make sure patients are informed and have clarity about their care 22.
Futile treatments at the end of life
Shepard and Pavlish et al., demonstrate that, for the majority of nurses, administering an aggressive treatment to oncology patients during the end of their lives is an ethically difficult situation 18,23. Similarly, witnessing the adverse effects of the treatment causes them moral distress, especially when the objective of care is focused on palliative care and not on curative care 28. The study by Lazzarin et al., shows that the situations in which the family wishes to continue with the treatment, although this is not the best for the child, is a circumstance that causes moral distress to the nurses caring for pediatric patients with cancer 33. The study by Pye mentions that for nurses moral conflicts emerge when limits do not exist with respect to the reanimation of patients at the end of their lives 30. Shepard, in turn, indicates that ethical conflicts appear when physicians and the families make decisions that harm the quality of life of the patients 18.
Assistance to patients and their families during the process of death
A qualitative study found that some of the important ethical conflicts in oncology refer to confronting situations appertaining to end of life, like administering aggressive treatments during this stage 29, responding to the request of suicide assistance by the patient when a bad prognosis is received 34, and delivering inadequate palliative care 30. This prolongs the process of death with unnecessary aggressive care and offers false hope 32.
Along with these situations, it has been added that many times health providers delay conversations about precarious prognoses or about the treatment at the end of life 29. Remaining silent upon these situations can act as a trigger of moral distress in nurses (23, 29, 33).
Interpersonal relations in the oncology staff
Poor communication
The health staff in oncology is comprised of members from various disciplines, and lack of communication among them lead to important problems being misinterpreted or misunderstood, which could provoke moral distress in its members 37. The qualitative research conducted by Pye indicates that poor communication and scarce dynamics within the team and within the decision-making process can influence the appearance of moral distress in nurses 30. In this regard, Jodoin et al., indicates that respect is fundamental for the opinions of the rest when the different professions do not coincide on what is best for the patient 36.
Inclusion of nurses as equal partners and informed in formal communication and in the deliberation processes is key to prevent moral distress 23,28,29,32. Staff meetings permit clarifying the procedure to follow in relation to the treatment and care plan 35. Discussing ideas, concerns, and feelings that emerge from the complex clinical situation permit diminishing moral distress (23, 32) and having better management to provide quality care to other patients 36.
Power relations
Differences in professional roles involve distinct power relations, and this can be reflected in the perception of a more or less positive ethical climate among the team members 16. Lack of participation in decision making leads to feelings of powerlessness and devaluation in nurses 30; these can believe that they are incapable of solving ethical conflicts, as well as fearing failure when solving them, or not having enough experience, and this will keep them from formulating ethical questions in the interaction with other professionals 17.
In the study by Pavlish et al., nurses report that working in ethically difficult situations requires time and space; however, the care system in oncology, often, sacrifices comprehensive care for care focused on efficiency due to the high demands of care 28. Additionally, some nurses expressed fear of speaking when their own professional or personal perspectives differed from the predominant voices of the medical care team 28.
Trust in the team’s competence
The study carried out by Ameri et al., in Iran 31 shows that working with colleagues or other health care providers who are quite competent to care for oncology patients propitiates the emergence of moral distress. Recognition of inadequate situations related with negligence, lack of preparation, and professional incompetence can lead these professionals to suffer this phenomenon 22,32,39. Added to this are prejudices among the different disciplines: for example, nurses indicate that physicians do not experience moral distress, given that they do not spend sufficient time with patients to have ethical conflicts 27.
Discussion
Figure 6 links the results from this review in light of the central concepts of the conceptual model of distress proposed by Barlem and Ramos. Said figure demonstrates that the scenario in which the emergence of moral distress is described in nursing professionals is the health institution, particularly the oncology unit, a micro-space of power that frames the health staff caring for cancer patients, as well as the relations developed among its members. This health staff is made up by different professionals, among which there are the nursing professionals. Nursing professionals who work with people with cancer are exposed constantly to complex clinical situations with associated ethical aspects. Besides, in this model, a key aspect is moral sensitivity, which implies having self-critical view to perceive the moral content of the actions, facts and thoughts related with their clinical practice 3 to, thus, become moral agents 40.
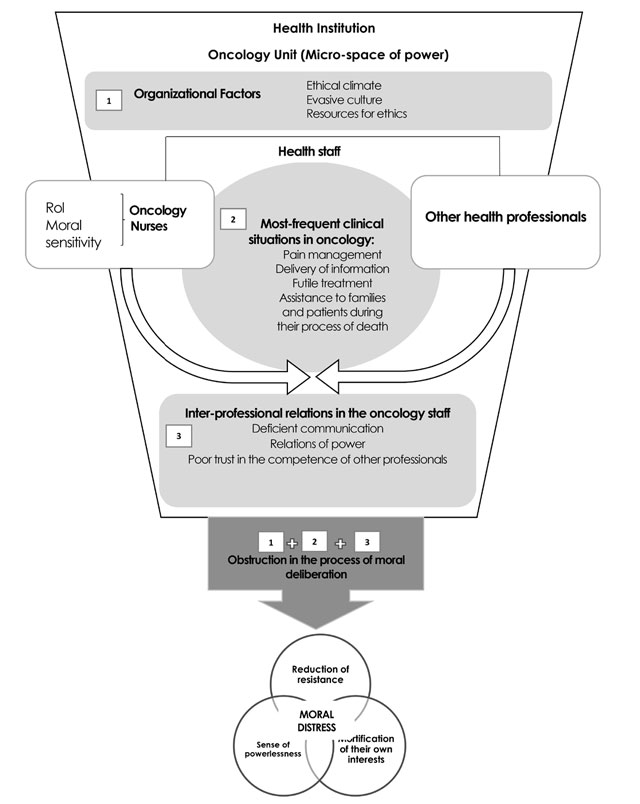
Source: authors’ elaboration from the model by Barlem and Ramos 3
Figure 6. Approximation of the review results of the factors that influence upon the emergence of moral distress in oncology nurses to the model by Barlem and Ramos
Figure 6 lists the triggering factors of moral distress in oncology nurses. First, there are the organizational factors that correspond to the ethical climate, evasive culture, and resources for ethics; these generate the organizational context in which the health staff performs. The institution plays a fundamental role in delivering the resources to develop ethical competences, and these permit nurses to negotiate and confront administrative and relational obstacles. The findings in this review agree with other authors 41,42 who indicate that it is necessary to provide a support environment in the hospitals and to consider strategies to diminish moral distress. In the oncology area, nurses report that the principal barriers for an ethical practice to take place are lack of time, absence of physical spaces for debate and support by the institutional leaders and policies that permit the development of an ethical climate, which coincides with the results found in nurses who work in the area of critical care 8,43.
The second factor in Figure 6 is the health staff confronting complex clinical situations, like pain management, information delivery, consideration of a treatment as futile, and assistance to patients and their families during the process of death. These situations can be favorable scenarios for the appearance of moral distress in oncology nurses 44, when these professionals do not participate in decision making in relation to therapeutic actions or when a clash of values occurs between the nurse’s perspective and that of other professionals in decision making. This finding is similar to that found in investigations in critical care 45,46, neonatal and pediatric areas 10,47, and is different from that found in emergency units, where other factors exist, like acute technical environment and high demand with insufficient resources 48. The third factor that triggers moral distress (Figure 6) is inter-professional relations in the oncology staff. In oncology, poor communication, differences in power relations, and poor trust in the competence of other professionals are described in this setting. Power relations, according to Barlem and Ramos, are not merely structures or prohibitions, but also consequences of constant and sustained confrontations over time that define the micro-spaces of power. In the case of oncology, the results show that a scarce dynamic exists within the teams, which marks these spaces with diminished participation by the nurses in decision making. Likewise, the relationship of power is manifested in the fear of nurses in dealing with difficult themes because they are afraid of damaging current or future work relations, which agrees with other studies 49.
In this review, power relations defined the space in which the moral deliberation process took place in oncology. In this key stage of the model, the professionals can discuss their own perspective, bearing in mind the visions of the rest of the team members, and this coincides with other authors who have highlighted the importance of the organization of the teams in the development of moral distress 50. When this process is obstructed, moral perspectives are silenced and the consequence is a feeling of powerlessness in the nurses that keeps them from undertaking the actions they perceive as correct. The obstruction triggers a chain of moral distress that includes the sense of impotence, mortification of their own interests and reduction of resistance to the phenomenon of moral distress. This triggers a process of normalization of the situation and of indifference toward the moral problems of the daily practice of oncology nursing.
Conclusions
The model of moral distress by Barlem and Ramos 3 permits giving flow to the elements presents in the emergence of moral distress and shows how the obstruction of the moral deliberation process and power relations are central elements in the chain of moral distress, by making it possible to link, coherently, the results of this review. Furthermore, it permitted arranging the results of the review in a cohesive diagram that exposes the dynamics of the teams shown by oncology nurses in the distinct articles reviewed. When ethical issues exist in the clinical situations experienced by oncology nurses, and they do not participate in the deliberation process, these can remain hidden and be presented as normal, which diminishes the moral sensitivity of the professionals and the possibility of acting as moral agents. In all, the three factors described are triggers of moral distress in oncology nurses.
The concept of moral distress applied in oncology involves problems related with the growing demand for care by patients and their families, scarcity of human and material resources, scarce organizational support, training in ethics, correct management of the information provided to the family on the patient’s treatments, times of reflection and dialogue regarding death, among others, which makes the study of this phenomenon in oncology even more complex.
Finally, in terms of the professional role, it is worth noting that studies are needed to explore physical, psychological, and behavioral manifestations in oncology nurses. Likewise, it would be important to investigate the implications of moral distress in caring for cancer patients. It is fitting to ask why some nursing professionals normalize the contexts in which moral problems develop and give up on moral resilience 51. The answer could be related with factors, like lack of personal skills, the wear caused by negotiating with other professionals, and clinical demands in oncology that take up an important part of the nurses’ time.