Introduction
The most commonly used cardiovascular risk stratifications are the Framingham Risk Score (FRS), the Systematic Coronary Risk Evaluation (Score) and the Prospective Cardiovascular Munster (Procam). However, few studies have measured them in comparison. In addition, it should be noted that the choice of method may involve different interventions according to guidelines established for each classification result. 1
Score, as well as other cardiovascular risk prediction scores, is used in specific groups such as patients with rheumatoid arthritis, recommended by organizations such as the European League Against Rheumatism (Eular). This score, by means of age, gender, total cholesterol levels, systolic blood pressure (SBP) and tobacco use 2, estimates mortality from cardiovascular disease (CVD) and atherosclerotic events.
Procam, like the others, estimates the risk of developing cardiovascular disease in ten years and has the variables LDL-cholesterol, triglycerides, diabetes and a family history of CVD. Some authors suggest that Procam, Framingham and other scores do not represent, in their entirety, cardiovascular risk by not including biomarkers of inflammatory activity, for example, in their calculation. 3
In Brazil, there are studies performed with Score, Procam and Framingham even though it is known that the current recommendation by the Brazilian Society of Cardiology (SBC) is the Framingham score, in order to work on the study of limitations in the real identification of patients of high cardiovascular risk. 4
The 7th Brazilian Guideline of Hypertension, in its Chapter 4, which deals with the stratification of cardiovascular risk, stresses that, in a more accurate evaluation in the Brazilian population, with a high prevalence of hypertension, the use of a single risk score should be avoided to base the therapeutic decisions. Therefore, it recommends multifactorial models in order to obtain a more precise individual risk classification 5.
The study of endothelial function by noninvasive techniques is of good predictive value to estimate cardiovascular events and be used as a tool to determine cardiovascular risk in asymptomatic patients. However, more studies need to be developed to strengthen the subject in order to create protocols to establish, in a consensual way, which screening parameters in a given population at risk are needed 6.
Therefore, the objective of this study was to investigate the agreement between modified FRS through the ankle-brachial index (ABI) and the high-sensitivity C-reactive protein (rsCRP) with the other scores.
Materials and method
Cross-sectional, population, observational, descriptive and analytical study, nested to a cohort, conducted from January 2018 to March 2018. Elderly access was achieved thanks to a facilitated access by a primary cohort study and by the support of the Municipal Health Secretariat of Aiquara, Bahia (Brazil).
It was included in the study people aged 60 years or older, living in the urban area of the municipality of Aiquara, Bahia, who slept more than three nights at the house where they were located, and that there was in the database information that would allow stratification by the three risk scores simultaneously. The individuals who presented incapacitating cognitive and physical conditions to respond to the form and to measure cardiovascular markers and risk factors and/or blood collection were not included in the study.
The data were obtained in three stages, performed by trained researchers and equipped with material needed for each data collection. In the first one, the research form was applied through home visits. In the second, the arterial pressures of the arm and the ankle were measured. In the last one, blood was collected in the morning with the elderly, after nocturnal fasting of 8 to 12 hours. The blood samples were collected, adapted and processed by the Central Laboratory of Vitória da Conquista (Lacem).
In the laboratory, serum levels of total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides and glucose were processed by colorimetric enzymatic reactions and dosed on the Beckman Coulter AU 680 Automated Analyzer by the spectrophotometry method. For those individuals with triglyceride values > 400 mg/dL, LDL cholesterol was calculated by the Friedwald equation. The rsCRP dosage was done in the same analyzer by the immunoturbidimetry method.
The conformation of the instruments of data collection was composed of modules arranged on the basis of groups of variables: 1) sociodemographic characteristics, family history of cardiovascular disease and referred morbidity; 2) clinical and biochemical variables (ABI, systemic blood pressure, glucose, HDL cholesterol, LDL cholesterol, total cholesterol, triglycerides and rsCRP).
Systolic blood pressure (SBP) was measured in triplicate by automatic digital blood pressure Omron, Hem-7320 model, in the same upper limb, and was considered elevated when ≥ 140mmHg and/or diastolic blood pressure (DBP) ≥ 90mmHg according to the 7th Brazilian Arterial Hypertension Guideline 7. High fasting glycemia was given as values > 100 mg/dL according to the Brazilian Society of Diabetes Guideline parameter 8. Total cholesterol was determined as altered with values ≥ 200 mg/dL; the HDL-c fraction < 40 mg/dL in men and < 50 mg/dL in women; the high LDL-c will be ≥ 160 mg/dL and triglycerides (TG) ≥ 150 mg/dL, according to the 5th Brazilian Directive on Dyslipidemias 9.
The reclassification of the FRS score was performed based on the ABI and rsCRP. The ABI was determined by the automatic oscillometric method, and adjusted the cutoff point from 0.9 to 1.0 second according to the meta-analysis. 10 The rsCRP was dichotomized from the cutoff point of > 2mg/L, indicative of cardiovascular risk and individuals with more than 10mg/L were excluded because they corresponded to a high inflammatory state 9.
The FMR considered classification at high risk, without stratifying, individuals with presence of DM and episode of acute myocardial infarction 11.
The PROCAM and FRS score 11 had its RCV in 10 years < 10 % classified as low risk, between 10 and 20 % intermediate risk and ≥ 20 % as high risk. The Score was classified as low risk (< 1 %), intermediate (1-4 %) and high risk (≥ 5 %) 2.
The degree of normality was verified for all variables using the Kolmogorov-Smirnov test. The qualitative variables were presented by means of absolute and relative frequencies and the continuous variables by mean and standard deviation or median and minimum and maximum values, according to normality.
For the analysis of the concordance of the modified FRS stratification with the other scores, the Kappa statistic was used with the categorization of very good (0.81 to 1.00), good (0.61 to 0.80), moderate (0.41 to 0.60), weak (0.21 to 0.40) and poor (< 0.20) 12. When the value of p was < 0.05, statistical significance was considered.
Double data entry was performed to minimize possible typing errors and correction through a spreadsheet built in Excel. The analysis of the data was performed in the software IBM SPSS® (Statistical Package for the Social Sciences), 21.0 version.
The research was approved by the Committee of Ethics in Research in Human Beings, from the Universidade Estadual do Sudoeste da Bahia, under project number 1,575,825. All individuals were informed about the purpose and risks of the research and signed a Free and Informed Consent Form as recommended.
Results
Individuals who met all the eligibility criteria to participate in the study totaled 158. There were 17 denials and 23 losses for cognition, 100 losses for not having enough data for the three stratifications simultaneously, and 16 were not found.
The characteristics of the population with data for the three risk scores are presented according to their sociodemographic and biochemical variables of cardiovascular risk in Table 1. Of the elderly evaluated, 59.5 % were female, 67.7 % were hypertensive, 47.6 % had altered rsCRP levels and 18.6 % were ABI. The high-risk stratifications for reclassified FRS, the FRS, Procam and Score were respectively 52.5 %, 39.9 %, 12 % and 43 %.
Table 1 Characteristics of the study population. Aiquara, Bahia, Brazil (2018) Values are presented as absolute number and frequency, mean ± standard deviation or median (minimum-maximum).
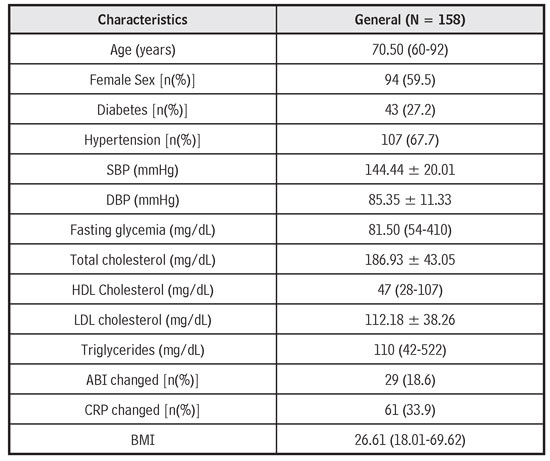
Source: Own elaboration.
The Kappa statistic showed a weak agreement between the modified FRS and Procam, and a moderate agreement with the reclassified FRS and the FRS, as well as the Score. Significant differences (p < 0.001) were identified between the reclassified FRS and the FRS, as well as between the reclassified FRS and the Score (Table 2).
Table 2 Kappa concordance analysis between reclassified FRS with other cardiovascular risk scores. Aiquara, Bahia, Brazil (2018)
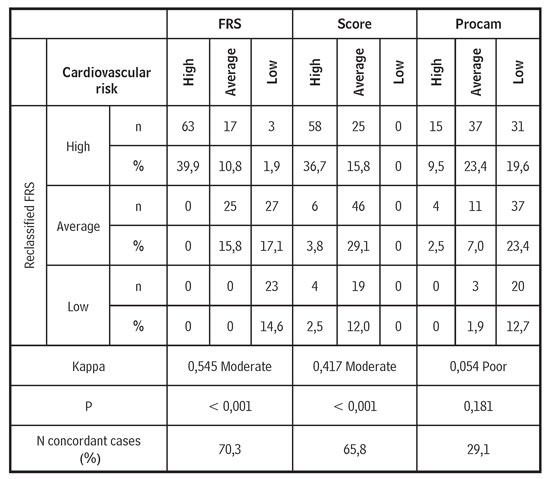
Source: Own elaboration.
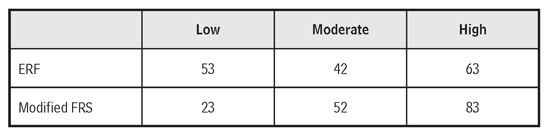
The reclassification with the rsCRP had a larger quantity than the ABI. It was found that 8 people were reclassified from low to high risk and 6 from moderate to high risk in relation to ABI. It was also identified that 25 elderly people were reclassified from low to high risk and 11 from moderate to high risk compared to rsCRP (Table 3).
Discussion
Among the elderly in Aiquara, self-reported arterial hypertension was the most prevalent risk factor, affecting 67.7 % of them. The mean systolic pressure was 144.44 mmHg, thus above the value recommended by the 7th Brazilian Hypertension Guideline 8. Among the study population, 53.2 % had the frequency of systolic blood pressure levels changed.
The National Survey on Access, Use and Promotion of the Rational Use of Medications (PNAUM), a population-based study conducted in municipalities of Brazil between September 2013 and February 2014 identified a lower prevalence of self-reported hypertension in the 60-year-old population (59 %). 13 Another Brazilian national survey, for individuals older than 75 years, the prevalence was 55.1 %; 14 in Campina Grande, Paraíba (Brazil), was higher (75.6 %) 15 and in a survey of the Surveillance System for Risk Factors and Protection for Chronic Diseases by Telephone Inquiry (Vigitel), the prevalence in age group of 55-64 was 50.3 % and, at 65 years or more, was 60.4 % 16.
When comparing the self-reported prevalence of hypertension in the elderly of Aiquara (67.7 %) with those of the PNAUM (59 %), it was identified that the values obtained in Aiquara, a small municipality, although superior, are close. It is worth mentioning that the PNAUM evaluated the resident population in municipalities of different population sizes. Faced with the increasing tendency of hypertension 13, the differences related only to the population size no longer sustain. The prevalence of hypertension in the study is probably due to the presence of many risk factors, easy access to the diagnosis provided by the Family Health Strategy, greater recognition of the elderly patient’s hypertensive condition or a synergism of all these factors.
Another important cardiovascular risk factor in all stratification is the presence of diabetes, whose self-reported prevalence in Aiquara was 27.2 %; this value is greater than that reported in elderly Brazilians in the National Sample Survey (PNAD) (16.1 %) 17 and also in population of four communities in the United States of America (10 %) 18.
It is important to mention that the isolated presence of diabetes classifies the individual in the category of high cardiovascular risk without having to make stratification to the FRS and Score since 2007. It is considered, however, that the stratification given by Procam considers the diagnosis of diabetes or the high glycemic value in its calculation, while others do not consider it, considering that the presence of this complaint already classifies the individual in the category of high risk.
The prevalence of the high-risk category scores of the reclassified Framingham, Framingham, Procam and Score were respectively 52.5 %, 39.9 %, 12 % and 43 %. The value obtained by Procam distances more from the two FRS when compared to the Score that presented better agreement by Kappa analysis. Thus, there was a moderate agreement between reclassified FRS and Procam, as well as between reclassified FRS and FRS with statistical significance (p <0.001), but weak agreement between reclassified FRS and Procam. Probably because there is inclusion of the variables LDL, triglycerides and glycemic value in Procam that is absent in the others. In addition, the Score did not present the category of low risk, since in it the age of 60 marks the elderly in the highest stratum.
Considering that the results obtained by the different methods used to estimate cardiovascular risk employ variables that are not always equivalent, and that there are also differences between geographic regions, time of patient follow-up, quality of data filling, it is presented justifications for differences of agreement in the classification of cardiovascular risk 19 demonstrated in the present study.
However, there is no consensus that the available scores can predict the risk of cardiovascular disease in low- and middle-income countries. It is necessary, however, to have these cardiovascular risk assessment tools to support daily clinical practice 20, with the objective of directing resolutive health practices.
In Brazil, FRS is the most commonly used cardiovascular risk screening method and recommended by SBC. It also presents the possibility of reclassifying risk through so-called “emerging factors” such as ABI and rsCRP. 9
The reclassification of FRS significantly improves the validity of cardiovascular risk, 5 since no score used in the risk assessment accommodates all known factors, and it would not be possible at all places to continuously produce updated risk functions based on prospective cohort studies 21. Therefore, reclassification is considered the best viable alternative 21.
Thus, in this research, ABI and rsCRP were used as additional investigation to improve cardiovascular risk assessment. The reclassification of the FRS from the ABI caused 14 elderly people to change their classification, and 36 elderly people reclassified by rsCRP. Based on these results, rsCRP, due to its higher prevalence of altered values (47.6 %) compared to ABI, contributed to a greater magnitude with the reclassification of cardiovascular risk.
It is important to add that rsCRP, considered an inflammatory marker, is also useful in improving cardiovascular risk assessment in individuals with atherosclerosis, even if they present only one or none of the traditional risk factors 22.
The rsCRP, for being part of the general inflammatory state, can detect chronic infections of low grade in several places and, therefore, contribute to the reclassification of risk. Reclassification is especially important in prevention, since high-risk individuals have a concrete indication of pharmacological treatment, while the same measure has an uncertain efficacy in the category of intermediate risk 22.
However, it is worth mentioning that, even though it is recommended by SBC, there is still no consensus on the use of rsCRP in routine primary prevention, although it presents clinically higher predictive capacity. Despite these findings, there is an indication of the need for validation of rsCRP in large-scale studies in order to clarify whether it contributes to reduce cardiovascular morbidity and mortality, but there is no doubt about its value as a marker of risk 22. In this sense, more studies are needed for an evaluation of the benefits and damages of adding these indices to the traditional risk assessment for CVD in asymptomatic adults to prevent CVD events 23.
Like rsCRP, ABI also has the ability to improve classification, discrimination (ability to distinguish between people who will or will not experience an event) and reclassification (transfer risk strata) 24. A meta-analysis, performed in the Japanese population using the oscillometric method, concluded that the lower the ABI values, the greater the risk of CVD and all-cause mortality 24.
Studies suggest the use of ABI in the reclassification of cardiovascular risk. Results of The Artper cohort, conducted in Spain, with people over 49 years (The ARTPER), support the addition of ABI to the reclassification of cardiovascular risk 25. Another study (Longitudinal Study of Adult Health - ELSA/Brazil), in which three different ABI methods were calculated, was associated with a high load of cardiovascular risk factors and, therefore, the authors recommend its application in primary care 26.
Thus, based on the results found, it is possible to infer that the reclassification of risk in the modified ERF generated large changes of classification and, consequently, may have more strongly influenced the level of agreement weak Kappa between the modified FRS and Procam. The modified FRS and the FRS as well as the modified ERF with the Score, presenting a moderate agreement, bear similarities mainly in the high-risk category. Even so, the FRS presents greater prediction of cardiovascular risk in Aiquara.
Conclusion
From the Kappa concordance analysis, it was concluded that the reclassified FRS presented statistical significance with the FRS and the Score, with the highest number of cases consistent with the FRS. The rsCRP and the ABI modify the cardiovascular risk of individuals between the strata and allow a more reliable and therefore more effective targeting of the therapy.
Since stratification is part of the standardized clinical management for those with systemic arterial hypertension, a highly prevalent and basic disease for numerous cardiovascular conditions, it is necessary to handle them appropriately considering the addition of emerging variables to give robustness to the results.
The FRS better predicts risk, however, coupled with aggravating factors, adds even more accuracy to more specific individual clinical guidance. This study demonstrates that the information on rsCRP and ABI obtained mainly in individuals at intermediate risk by FRS, which resulted in their change of category, brings an incremental value analysis to the stratification of cardiovascular events. New markers, then, can improve stratification in groups at risk of multimorbidity, such as the elderly.
Therefore, it is necessary a clinical practice with the greatest possible contribution of measures to the adequacy of cardiovascular risk and, consequently, the individualized and effective therapeutic targeting that leads to lower risk of mortality and better quality of life for individuals.