Introduction
Intracranial pressure (ICP) is an event of great clinical repercussion that attacks patients with brain tumors, severe brain injury, and extensive ischemic and hemorrhagic cerebral vascular accident. Increased ICP is a major cause of secondary cerebral lesion and is frequently associated with worsened neurological evolution 1-3.
Conceptualized as cerebrospinal fluid (CSF) pressure from blood and brain tissue pressure, normal values range from 5 to 15 mmHg. 4. In critically ill patients, ICP may vary due to changes in blood pressure, ventilation, patient positioning, as well as changes in carbon dioxide and oxygen pressures 5. Increased ICP, above 20 mmHg, has as an important physiological repercussion in the reduction of cerebral perfusion pressure and cerebral blood flow, in addition to compressing brain structures and contributing to hydrocephalus, besides causing brain herniation 6-9.
Intracranial pressure monitoring by implanting a polyethylene catheter into the ventricular cavity connected to a pressure transducer is critical to prevent secondary brain damage that contributes to increased morbidity and mortality 10-13. Despite being an invasive procedure that involves health and safety risks to those who use it, it is the only accepted method for the safe diagnosis of increased ICP, as well as for its treatment in some clinical situations 14-16.
Added to the control of clinical, hemodynamic, respiratory, and metabolic parameters, monitoring the ICP helps and guides the therapy of neurological patients, as it allows for its rapid recognition and permits assessing the therapeutic efficacy, as well as brain injury 17-18.
Although catheter insertion is an inherent procedure for the neurosurgery team, its care and ICP monitoring are the responsibilities of the intensive care unit (ICU) nursing staff 19.
In addition, it should be considered that the nurse is the bedside professional giving meaning to the ICP monitoring parameters, through theoretical knowledge, logical reasoning, and experience acquired in practice 20. Care consistent with knowledge and practices combined with educational and care actions in the professional practice to ensure the quality of care provided to neuro-critical patients 21.
In the ICU, Nursing professionals should avoid unnecessary harm during health care delivery to improve the care provided and prevent iatrogenesis 22-23. Iatrogenic events, within this context, may put patient at risk of life and bring complications that may compromise their clinical course and safety 24.
It should be noted that increased ICP often occurs as a result of routine nursing procedures, such as bed bath, patient positioning, and oral and bronchial hygiene, among others 25-26. In this sense, the nursing staff should be aware of signs and symptoms of worsening intracranial hypertension, which depend on the location of the brain injury. However, the most common symptom is worsening mental state 27-29.
In this sense, systematization of Nursing care (SNC) is an important tool, given that it permits the Nursing staff to organize and direct their practice to the specific needs of each patient and prevent unnecessary harm 30.
Considering that the quality of health care is linked to the incorporation of good nursing practices, this study sought to know the interventions directed to patients with ICP monitoring to contribute to care based on scientific principles and the best evidence.
The objective of this study was to identify, in national and international publications, the principal Nursing interventions aimed at patients with intracranial hypertension.
Materials and Methods
Integrative literature review, conducted in five stages: problem identification, literature search, data evaluation, data analysis, and presentation of integrative review or synthesis of knowledge 31-32. To conduct this study, the following question was used: “What nursing interventions are described in the scientific literature for patients with intracranial hypertension?”
To search for the articles, on-line access was used to the following databases: Latin American and Caribbean Literature in Health Sciences (LILACS, for the term in Spanish), PubMed, Scopus, Web of Science, Cinahal, and Google Scholar. The descriptors selected from the list of Health Sciences Descriptors (DeCS) were: “hemodynamic monitoring”, “intracranial pressure”, “Nursing care” and “Nursing assistance”, “Nursing interventions”, “neuro-intensive care”, with Boolean operators OR and AND.
The search was carried out in December 2018. To include the articles, the following criteria were considered: original articles that addressed the guiding question, published between 2013 and 2018, in Portuguese, English, and Spanish. Articles not available in full, experience reports, literature reviews, theses and dissertations were excluded.
In order to obtain more accurate results, the search was aided by two researchers involved in the study. For the data collection of the studies, an instrument was elaborated that included the following information: year of publication, authors, objective, country in which the study was carried out, database, research design, sample detailing, intervention, results and recommendation/conclusions. Such information contributed to the analysis and synthesis of the data obtained in the search.
Results
The study initially identified 630 articles; of these, 380 were excluded because they were duplicated in the databases. Thus, 250 articles were selected to read the title and abstract, which resulted in a sample of 50 articles for full-text reading. Of these, 43 were excluded for not answering the guiding question, which lead to a total of seven articles (Figure 1). Four studies were conducted in the United States, two in Europe, and one in Brazil.
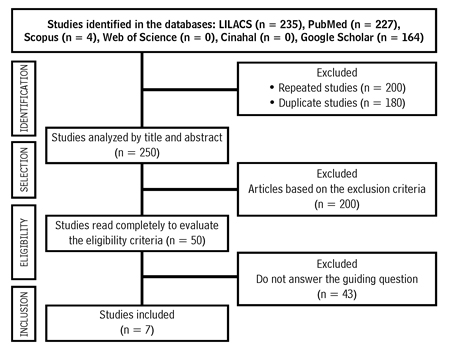
Source: Own elaboration.
Figure 1 Selection process of articles in the integrative review (Botucatu, Brazil, 2019)
Table 1 presents the characteristics of the articles selected for this review, according to author, year of publication, database, research design, and results associated to Nursing interventions.
Table 1 Articles included in the study according to title, author, place, year of publication, databases and countries of origin, research design and main results and interventions (Botucatu, Brazil, 2019)
| Author/year/research location/database | Article title | Research design | Results associated with Nursing interventions |
| Article 1 Rosa NM, Lima JF, Inoue KC, 2013 (33), Brazil, LILACS | Knowledge of Nursing staff on neuro-intensivism and the influence of continuing education | Descriptive, exploratory, and quantitative study, which sought to characterize the knowledge of the Nursing staff on neuro-intensivism. | • Normality parameters of CPP, MBP, CVP, SvJO2, ETCO2, ICP. • Parameters to note for patient assessment. • Nursing care after patient manipulation. • Aspiration of endotracheal tube. • Mathematical representation of parameters to calculate CPP. • Factors and/or procedures that contribute to elevation of ICP. |
| Article 2 Uğraş GA, Yüksel S, Temiz Z et al., 2018 (34), The United States of America, PubMed | Effects of different head-of-bed elevations and body positions on intracranial pressure and cerebral perfusion pressure in neurosurgical patients | Quasi experimental study. | The study showed that different patient and headboard positions led to insignificant changes in ICP and CPP. |
| Article 3 Sacco TL, Delibert, SA, 2018 (35), The United States of America, PubMed | Management of intracranial pressure: Part I | Descriptive study. | Nursing care for these patients includes collaboration with an inter-professional staff and is oriented at patient and family comfort. The use of a guideline based on evidence to manage ICP is strongly encouraged to improve the results of patients. |
| Article 4 Nyholm L, Steffansson E, Frojd C et al., 2014 (36), Sweden, PubMed | Secondary injuries related to nursing interventions in neuro-intensive care: a descriptive pilot study | Prospective, observational study that aimed to investigate events secondary to oral hygiene, bed mobilization, endotracheal aspiration, hygiene measures, and simultaneous neuro-intensive care interventions. | The most common type of event after Nursing care was increased ICP, followed by low cerebral perfusion pressure and mean blood pressure. |
| Article 5 Robinson JD, 2015 (37), The United States of America, PubMed | Management of refractory intracranial pressure | Descriptive article that addresses the approaches to treat brain injury and emphasizes the role of nursing in controlling ICP. | • Safe airway. • Maintain eucapnia. • Avoid hypotension. • MBP > 90mmHg. • Maintain glycemia levels between 80 and 180 mg/dl. • Maintain temperature at 37 °C. • Adequate sedation. • Maintenance of bed elevation at 30 degrees. • Maintain head neutral (aligned with the body). • When using a cervical collar, two fingers should fit inside the collar. • Medications used to control ICP: mannitol 20 % and hypertonic saline solution. • For decreased brain metabolism, barbiturates or hypothermia. The authors emphasize the role of nursing in hypotension control after pentobarbital bolus. Hypothermia (32 to 34 °C) reduces ICP for 24 to 72 h. • Recognition of signs of brain herniation: asymmetrical, non-reactive pupils, decortication or decerebration posture, bradycardia hypertension and respiratory arrest. |
| Article 6 Szabo CM, Grap, MJ, Starkweather A et al., 2014 (38), The United States of America, PubMed | The Effect of oral care on intracranial pressure in critically Ill adults | Observational, non-experimental study, which sought to investigate the effects of care of oral hygiene on ICP. | The repeated-measures mixed-effect variance analysis model indicated a statistically significant increase in ICP in response to oral hygiene (p = 0.0031). However, there was no clinically significant effect on ICP. This study provides evidence that oral hygiene is safe for patient performance in the absence of pre-existing elevated ICP. |
| Article 7 Nyholm L, Howells T, Enblad P, 2017 (25), Sweden, PubMed | Predictive factors that may contribute to secondary injury with nursing interventions in adults with traumatic brain injury | Prospective, quantitative study seeking to investigate the risk of inducing high intracranial pressure related to nursing interventions.. | Increase of secondary ICP related to nursing interventions occurring in six patients (21 %) and eight occasions (12 %). Patients with baseline ICP of 15 mmHg or more present risk 4.7 times higher of developing an injury. The initial ICP of 15 mm Hg or more was the most important factor to determine the risk of injury secondary to ICP. |
CPP - Cerebral Perfusion Pressure; MBP - Mean Blood Pressure; CVP - Central Venous Pressure; SvJO2 - Jugular Bulb Oximetry; ETCO2 - CO2 at the end of expiration.
Source: Own elaboration.
Figure 2 shows the structural synthesis of nursing interventions identified in the literature (Botucatu, Brazil, 2019).
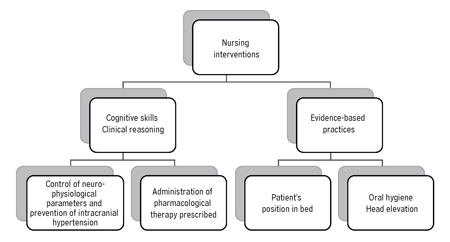
Source: Own elaboration.
Figure 2 Structural synthesis of the Nursing interventions (Botucatu, Brazil 2019)
The reading and analysis of the articles permitted observing that the Nursing interventions are linked to cognitive skills and clinical reasoning, but they should also be supported by practices based on the best scientific evidence.
The nurse’s cognitive skills and clinical reasoning are fundamental to interpret the neuro-physiological and hemodynamic parameters, prevent the increase of ICP during Nursing procedures, and administer the pharmacological therapy prescribed. However, it is in evidence-based practice (EBP) that care has the scientific support needed to improve care practice.
Discussion
Caring for patients with neurological alterations is a big challenge for the whole Nursing staff. Patients with ICP require specific and continuous care in ICU and demand maximum attention from the health staff and minimum manipulation, in order to avoid possible deleterious injuries or aggravate those existing 20,39-41.
As prerequisite to monitor ICP, the nurse needs to be aware of the principles of monitoring, neuro-anatomy, and neurophysiology, as well as the pathophysiology of intracranial hypertension (ICH) 42. It is known that increased ICP may be associated with the patient’s clinical condition or may occur in response to routine Nursing care. Therefore, the focus of medical and nursing interventions should be the prevention or minimization of secondary brain injury 37,43-44.
A study conducted with 18 patients with neurosurgical diagnoses revealed that the most common types of secondary events after Nursing care were increased intracranial pressure, followed by a fall in cerebral perfusion pressure and mean blood pressure. The authors concluded that patients with increased risk of secondary events must be recognized and their care and treatment must be rigorously planned 36.
In this sense, the literature emphasizes the importance of Nursing empowerment in the multidisciplinary staff and the use of care protocols that include interventions to control and manage ICP to intervene briefly and effectively in treatments aimed at mitigating this event, as well as adjusting nursing procedures that, by association, may increase intracranial hypertension and decrease cerebral perfusion pressure 25-27.
In the survey conducted in this research, it was identified that nursing interventions are linked to cognitive skills and clinical reasoning, essential to interpret the monitoring parameters and implement care to control ICP.
The interventions described in the literature found during the search period are neuro-physiological and encompass monitoring of hemodynamic parameters, like oxygen saturation, mean blood pressure, temperature, ICP, and cerebral perfusion pressure.
This search identified two works that describe procedures that, indirectly, can contribute to increase ICP and whose scientific evidence supports the best care. One of the procedures is the elevation of the bed headboard and the body position. Although the only study that addressed the subject did not find a statistically significant change in ICP values with the bed headboard at 15, 30, and 45 degrees, as well as in the supine, right, and left lateral positions, the sample size of 30 patients was considered a research limitation 34. However, other investigations show that patients with increased ICP benefit from head elevation by 10, 15, 30, and 45 degrees compared to zero degrees 45-46.
The other procedure described in the literature that contributed to increasing ICP is oral hygiene. A study that analyzed the influence of this procedure in 23 patients with ICP monitoring showed statistically significant increase of this parameter during oral hygiene (p = 0.0031), but without clinical repercussion 38.
Although this review did not include the inclusion of articles on endotracheal aspiration, it is essential to contextualize this procedure, which may also lead to increased ICP. A clinical study aimed at determining the best aspiration technique (open versus closed system) with 32 neurosurgical patients, showed that patients aspirated with open system had significantly lower mean carbon dioxide partial pressure than those aspirated with closed system, but without significant difference 47-50.
A recent study concluded that while most articles show an increase in ICP above 20 mmHg, when using the open aspiration system, it is still unclear which is the best technique to maintain adequate cerebral perfusion pressure. For the authors, more studies are necessary to determine the best endotracheal aspiration technique for the Nursing practice 51-52.
Implementing EBP-based care is critical to achieving effectiveness, reliability, and safety in health practices 53-54. In this context, nurses play an important role in planning the care for neuro-critical patients, given that they require daily systematized evaluation 35,54.
Nurses should be very cautious, given that routine procedures can aggravate the neurological condition due to the increase in ICP and decrease in cerebral perfusion pressure. Therefore, professionals must be trained to provide safe and qualified care to critically ill patients, given the need for constant attention in the application of interventions for their recovery 20,33,55-59.
Thus, the neurological assessment is essential to identify Nursing diagnoses, a crucial stage to elaborate a care plan based on a theoretical framework, which guides and improves the practice, as well as directs nursing interventions and expected results 60-61. In addition, the underlying clinical decision to care is paramount to the quality and excellence of the nursing practice in neuroscience 62.
A limitation of this research was that of obtaining studies with small sample sizes; therefore, it is necessary to develop more robust studies on the theme.
Conclusions
Intracranial hypertension is an event of great clinical impact. Complications arising from this event can be minimized and controlled through specific nursing interventions that include controlling neuro-physiological and hemodynamic parameters, as well as preventing the increase of ICP, often linked to the performance of nursing procedures.
The results of this study also evidence the importance of the best evidence-based care practice to support the multifaceted care that neurological patients require in ICU and whose success depends on a cohesive inter-professional staff, which also recognizes the family as an integral part of health care.
Despite the number of publications on the pathophysiology, it was found that few studies address Nursing care to the family and the patient affected by this secondary lesion, which may evolve to death.















