Introduction
Despite the technological advances and the emergence of new treatments, cancer and other chronic diseases have shown an increase worldwide, regardless of the countries’ income levels. For example, in the context of low- and middle- income countries, chronic diseases are the first cause of death1. Many of them progress and require palliative care due to late diagnosis, disease aggressiveness, or treatment failures2.
Added to the aforementioned, the experience of a person with an advanced disease in palliative care is characterized for being complex, with important physical and spiritual needs, and the family caregiver accompanies this situation3. On many occasions, these caregivers must take on their role without adequate training, without the continuous accompaniment by health professionals, and without appropriate support networks, which triggers in them feelings of uncertainty towards the patient’s disease4. Additionally, becoming a caregiver implies stressful factors, changes in the relationships, and expectations regarding the care tasks, which generate control imbalances5, emotional instability, and negative feelings towards this new reality6,7.
Family caregivers of patients in palliative care experiment sensations and feelings like those described, but with higher intensity, reason why they present greater episodes of anxiety and depression than caregivers of other types of patients8-9. According to a study supporting that assertion, 80 % and 82 % of the caregivers present anxiety and depression signs, respectively, whereas 69 % noticed overburdens in their duties. Added to this are the characteristics of the context, in which they are constantly close to the death of the person they are caring for, a factor which increases uncertainty towards the disease10.
Such uncertainty towards the disease is a cognitive state that inhibits the person to determine the meaning of the events related to the disease, which generates inability to assign definite values to objectives and events and to accurately predict consequences11.
Evidence shows that other aspects related to uncertainty towards the disease of the caregiver are lack of knowledge on the patients’ situation, their home care, and medication management, apart from the absence of follow-up and social support6-7. Thus, the importance having been described of approaching uncertainty towards the disease for the caregivers of people in palliative care, the aim of this article is to know the development of the scientific evidence on uncertainty towards the diseases of family caregivers of patients in palliative care.
Materials and methods
A descriptive review of the scoping review type12 which aims to answer the following questions: What is the current state of the scientific knowledge on the phenomenon of uncertainty towards the disease in caregivers of patients in palliative care? What kind of evidence is found on the theme and what are the gaps in research? The search was conducted in the Embase, ScienceDirect, Medline, Academic Search Complete, and Scopus databases, in the English, Spanish, and Portuguese languages, and was limited to the 2000-2019 period. The MeSH terms and the Boolean operators were used as follows: uncertainty AND palliative care OR end of life AND nursing AND caregiver.
The inclusion criteria considered for this review are original articles or those derived from research which included subjects such as caregivers of patients with cancer or with other chronic diseases in advances stages, at the end of their lives, or in palliative care. Books and theses were excluded due to their extension, as well as reflection and narrative review articles, for the impossibility of cataloging them within the levels of evidence given by the Joanna Briggs Institute (JBI)13. The classification of the evidence used was by levels of effectiveness and meaning, which apply to quantitative and qualitative studies, respectively. The highest level of evidence was classified with 1 and the lowest, with 5.
This type of classification was selected because it is one of the broadest in the inclusion of various methodological approaches. The strategy for conducting the search and selecting the articles is detailed in Figure 1. The bibliographic search lead to the selection of 145 original articles, 65 being excluded due to failures in their internal validity; after applying the CASP-e instrument, 50 original articles or research results were selected for analysis.
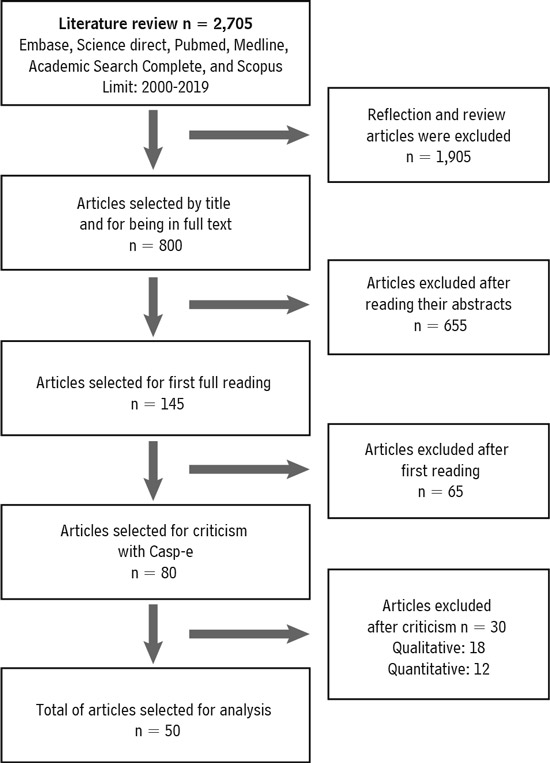
Source: Own elaboration.
Figure 1. Flowchart of the strategy for conducting the search and selecting the articles. Bogotá, 2020.
The steps proposed by the selected review methodology were developed12, which include: question, objective, inclusion criteria, participants, main concept, context, search and selection of articles, extraction and classification of results, and discussion12. To analyze the information, the articles were compiled in Microsoft Excel, where a matrix was created in which the following were defined as variables to be considered: research approach, study design, data collection means, analysis used, its main results, and conclusions. Subsequently, the quality of the article was criticized by means of the CASP-e instruments, a series of checklists to assess the contents of quantitative and qualitative studies. Those checklists contain questions to identify if, in the research article, there is a clear definition of the study objectives, coherence in the methodology employed, and adequate selection of participants, among other aspects14.
The information was organized by common characteristics and a name was assigned to each group of articles, taking into account the criteria of thematic or methodological affinity. This process generated a total of five groups: 1) Characterization of uncertainty in the caregiver, 2) Factors influencing uncertainty, 3) Resources to manage uncertainty, 4) Uncertainty assessment, and 5) Therapies and interventions to approach uncertainty.
Faced with the ethical considerations of the study, the researches took into account the principles of copyright when using and referencing all the material analyzed.
Results
The thematic distribution of the information lead to an integration of the most frequently approached concepts in the articles. It was found that the most frequently approached concept was that of factors influencing uncertainty, with 36 % of the total frequency of the themes. In the case of the methodological approach, the qualitative research was predominant, with 38 % of the total analyzed, as well as the development of interventions for caregivers, with 8 %. The information is presented in Table 1.
Table 1 Distribution of the reviewed articles according to methodology and theme. Medellin, Colombia, 2020
| Themes | Methodological approach | Total n (%) | ||||
|---|---|---|---|---|---|---|
| Qualitative n (%) | Quantitative | Systematic reviews n (%) | ||||
| Non-experimental n (%) | Experimental n (%) | |||||
| Characterization of uncertainty in the caregiver | 1 (2) | 5 (10) | - | 4 (8) | 10 (20) | |
| Factors influencing uncertainty | 10 (20) | 7 (14) | - | 1 (2) | 18 (36) | |
| Resources to manage uncertainty | 6 (12) | 3 (6) | 3 (6) | - | 12 (24) | |
| Uncertainty assessment | 2 (4) | 2 (4) | - | 2 (4) | 6 (12) | |
| Therapies and interventions to approach uncertainty | - | - | 4 (8) | - | 4 (8) | |
| Total | 19 (38) | 17 (34) | 7 (14) | 7 (14) | 50 (100) | |
Source: Review data, 2009-2019.
Apart from the contributions found in each of the reviewed articles, Table 2 presents the predominant level of evidence according to the JBI 13 and the voids in the research according to each thematic category.
Table 2 Levels of evidence and explicit voids found by theme. Medellin, Colombia, 2020
| Themes | Level of evidence according to the JBI* | Explicit voids |
| Characterization of uncertainty in the caregiver | Levels 1B, 2B, and 4B in effectiveness | Research must point to the development of studies which comparatively establish uncertainty levels in caregivers of individuals at the end of their lives, as a consequence of diseases other than cancer. It is necessary to characterize the uncertainty of the caregivers and its relation with mental health and the coping processes they go through. |
| Factors influencing uncertainty | Level 3 in meaning and Level 4B in effectiveness | Studies must be conducted which verify the influence of various factors on the levels of uncertainty towards the diseases of the caregivers. |
| Resources to manage uncertainty | Level 2 in meaning and Level 4B in effectiveness | Health professionals are one of the resources that can best help control uncertainty in the caregivers; however, what the literature describes shows the lack of training in palliative care and in communicative skills to approach those caregivers. It is then important to know the perception and experience of these professionals towards end of life, as well as to develop interventions that favor these competences for palliative care. |
| Uncertainty assessment | Levels 4B and 4B in effectiveness | Research must be targeted to the development of valid and reliable instruments with enough sensitivity to assess the uncertainty of the caregiver in different contexts of diseases in advanced stages and at the end of life. With this, the expectation would be being able to determine the schooling level of the caregivers, the social support they have, their perception of the health professionals, and the coping strategies leading to a positive or negative assessment of uncertainty towards the disease. |
| Therapies and interventions to approach uncertainty | Levels 1C and 2C in effectiveness | This theme is the one that presents the fewest studies. There are few existing interventions to approach uncertainty in caregivers of individuals in palliative care. Thus, the need emerged to develop different intervention strategies about uncertainty towards the disease and its influencing factors and, to this end, it is necessary to assess its acceptance by the caregivers, its impact, and its effect. |
Source: Review data, 2009-2019.
Discussion
Below are the findings in the literature for each thematic category.
Characterization of uncertainty in the caregiver
In a descriptive manner, the literature reports that the caregivers of individuals in palliative care have higher levels of uncertainty than other types of caregivers of people in acute or chronic conditions. For example, a study15 assessed the level of uncertainty in caregivers of patients with prostate cancer and found a mean value of uncertainty of 60 out of 140 points; however, such values are lower than those found in another study16, which discovered a medium level of uncertainty of 92 points out of 155 in caregivers of patients in palliative care. The studies suggest that these levels occur due to aspects like the specific characteristics of the palliative care context, the absence of adequate support for the caregivers, the discontinuity of care, and the lack of professional skills to identify the caregiver’s needs, apart from limited planning and evaluation of the objectives of patient’s caregiver17-18.
As observed, there are some unique characteristics associated with caring for a person in palliative care, and they are related to the appearance of uncertainty towards the disease. The caregivers report high prevalence of unmet care needs that trigger negative results in the execution of their role. Those needs include access to truthful information (about themes like the physical care of the patient), psychological support, access to funding support, and spiritual well-being. The studies19 show that there is a 26 % to 100 % prevalence of unmet needs in aspects such as receiving information related to the care for the patient, the disease, its treatment, management of symptoms, nutrition, and medication. The unmet needs of the physical type represent 42 % and are related to the quality of care; the psychological needs vary from 17 % to 78 % and refer to the management of sadness and solitude, among other aspects; the financial needs vary from 17 % to 67 % and are related to finding financial support and governmental benefits for the caregiver and for the patient; the spiritual needs vary from 3.8 % to 100 %, and imply re-signifying the experience; finally, the social needs vary from 42 % to 71 % and are connected to the absence of social support to help in the care provided.
These reported needs differ from those of other caregiver populations, since the health condition and care demands of a person in palliative care increase with time. Additionally, not only care in basic activities of daily life is required but also, as the disease progresses, the management of complex devices such as drainage systems or infusion pumps becomes necessary, as well as of medications like opioids and anxiolytics20. Finally, having to face the end of life, death, and the imminent loss of a loved one21 makes the experience of caring for a person in palliative care unique and complex, for having to fight an anticipated duel every day, faced with the expectation of the condition worsening or of the appearance of new symptoms in the patient, with the addition of uncertainty about the future22.
In many occasions, the uncertainty towards the disease experienced by the caregivers generates negative outcomes in them. For example, mental health problems have been reported due to the fact that the same caregivers mention a care burden which ends up affecting their own psychological well-being. Other negative outcomes are related to the reduction in quality of life, the appearance of fatigue, depression, anxiety, isolation, solitude, sadness, and frustration23-24. Thus, uncertainty towards the disease is characterized by bringing along problems in all the dimensions of the family caregiver’s quality of life.
Factors influencing uncertainty
This part describes what the literature reports about the factors associated to uncertainty in the family caregiver of a person in palliative care; they are circumscribed to lack of knowledge, invisibilization of the caregiver role, absence of social support, and quality of life.
As regards the lack of knowledge about the disease, diverse studies have found that it increases uncertainty towards the disease. It has also been reported that, although there is lack of knowledge in the caregivers, certain duality is experienced between what the caregivers want to know what they actually know. A research study described that caregivers are in for big surprises when they discover that the patient’s disease is incurable or that it is in a terminal phase25, a notion that is seldom clear for the caregivers and is minimally approached by the health professionals26. The consequence of the aforementioned is a phenomenon called ambiguous loss27, which is characterized by the caregivers’ inability to work on the feelings of loss of their loved ones, since the disease prognosis or the final outcome are not clear28.
On the other hand, caregivers refer to having little knowledge related to the physical care for the patient, in aspects like medication, pain control, and support for the activities of daily life. In a study it was reported that, out of twenty caregivers interviewed, only six recognized the term opioid29. It was also found that the caregivers possess false beliefs related to the addiction to pain killers, and that they feel overwhelmed by the complexity of the administration of analgesia, the use of the subcutaneous route, the assessment of pain, and the anxiety for the onset of uncontrolled pain episodes. This situation derives from the health professionals not acknowledging the role of the caregivers and their work in pain management30.
As regards the educational needs targeted to the activities of daily life, the caregivers do not receive any training on mobilization, lifting, change of positions in the bed, taking the patient to the bathroom, hygiene in the bed, care for the skin of the patient, or prescribed diet25,30. For this reason, they must learn them through the trial-and-error method, which exposes the patients and their caregivers to a high risk of physical injuries31, as well as to feelings of frustration in the caregivers, due to the scarce feedback they receive on the success or failure of their efforts.
Regarding the invisibilization of the caregiver role, the literature reports that the non-inclusion of the role by the health professionals in the care processes for the patients generates in them anxiety and fear in relation to the responsibilities they must take on in the home, responsibilities for which they do not feel prepared32-33. An example is the case of the caregivers stating that the health professionals do not listen to them, do not have time to talk and discuss care issues, and do not include them in decision-making, making them more vulnerable to stress and to uncertainty33.
Likewise, non-inclusion and lack of recognition of the caregivers leads to a dynamics in which they do not want to disturb or hinder the work of the health professionals, for perceiving themselves as obstacles for the care provided34; however, they expect that the health professionals establish an assertive, honest, simple, and empathetic communication on the patient’s condition, decision-making on the removal of futile treatments, and the expectations they can have about their care and end of life35. In the caregivers, these behaviors increase self-confidence and reduce the feeling of being navigating with no defined course36.
With respect to social support, the caregiver of a person in palliative care perceives its reduction as the disease progresses. Some studies show that its availability and quality decrease after a year of the diagnosis, which implies a great challenge for the caregivers of patients with pathologies like advanced cancer, who need stronger support systems as the disease progresses37-38. The aforementioned generates in the caregivers consequences like job loss or reduction in the number of hours devoted to it, physical and emotional exhaustion, absence of an effective coping, and limited time for themselves39.
Finally, various research studies concluded that uncertainty towards the disease is an influencing factor on the caregivers’ quality of life. In a study40, it was found that uncertainty towards the patient’s disease was a weak negative predictor in the report of quality of life related to the health of the caregiver [r = -0.29, p = 0.002]. Likewise, another study41 identified that, in family caregivers of adolescents with brain tumors, uncertainty was related to a reduction in the psychological dimension of quality of life. Another study42 showed that, when fewer fears and doubts exist about the disease, uncertainty is low, the caregivers’ quality of life improves, and they better cope with the situation. Such aspects ratify the importance of the support that health professionals must provide to family caregivers.
Resources to manage uncertainty
The resources available for the caregiver play an important role in reducing uncertainty towards the disease, and are related to education for the caregiver, to social support, and to accompaniment by the health professionals.
Diverse studies support the importance of education in the reduction of uncertainty, among them Henson et al.43, who discovered that the caregiver’s decision-making process about going to the urgency service with the patient derived from the education imparted by the health professionals. Additionally, Teno et al.44 determined that lack of education made the caregivers feel excluded from the decisions about the patient’s treatment. They also found that some caregivers do not want to listen to opinions on the progress of the disease45 or receive excess information; they rather reject the subject46.
The studies presented coincide in considering education as a predictor of the caregiver’s overload (B.17, p = 0.017)47. That is to say, the family caregivers of individuals in palliative care who have been advised on the disease, the treatments, the symptoms, and the probable outcome understand the situation they are facing and, by using their coping mechanisms, moderate the onset of the care burden and, consequently, the appearance of uncertainty towards the disease48.
On the other hand, some studies show that social support modulates uncertainty in the caregiver. For example, those caregivers who managed to share their experiences and express their doubts and fears to people in their same situation consider themselves better prepared for providing care (p = 0.014)49. Parallelly, those who have close friends or relatives who are health professionals, and who better explain to them the medical terms, learn to change their life perspectives and to feel validated in their duties50. On the other hand, it has been proved that high levels of uncertainty are associated with a low perception of social support (r = -0.36, p < 0.05)51, as well as with higher levels of anxiety and of depressive symptoms52.
Finally, as regards the due accompaniment by the health professionals to the family caregivers of individuals in palliative care, it was evidenced that the caregivers experience uncertainty towards the disease when they resort to the health professional looking for answers they do not find: this frustrates them53. Hence, as credible authorities, health professionals must be willing to listen to the caregivers and guide them in relation to their concerns. In this regard, another research study54 concluded that, when the caregivers have the opportunity to talk to the health professionals about themes related to the patient’s disease, they feel recognized, empowered and supported, and this reduces their uncertainty towards the disease.
Uncertainty assessment
The context of the care provided to a person with an advanced disease and in palliative care differs from the conditions that arise when caring for someone with another chronic or critical disease, since the complexity of the care situation increases as the patient nears end of life. The assessment that the caregivers make about the uncertainty they experiment is often negative, that is, they evaluate it as a constant chaos where no relationship among the events experienced is perceived55. For example, it has been found that uncertainty is assessed negatively when there is a daily fluctuation in the symptoms, such as pain in the patient56.
In view of the panorama described, it is fundamental that the caregivers familiarize themselves with the situation, the disease, its evolution, and its care, which is attained with time and through experience. Those caregivers who do not receive information on the prognosis of their patients report high levels of uncertainty, as a result of facing reality differently than what they had expected57, because they did not expect the patients’ conditions to worsen so markedly or for them to approach end of life so suddenly. Experiences like seeing that the patient was fine in the morning and then entered into an agony situation in the afternoon are frequent58.
In contrast, some studies have found a positive assessment of uncertainty in contexts of less adverse diseases, with caregivers of patients under prolonged treatments59. In these cases, as time passes, uncertainty is seen as an opportunity for personal growth and for strengthening the relationship with the loved one in palliative care. Added to this is the re-establishment of hope about new goals, the re-signification of the experience, and a better coping process for death and its subsequent grief60-61.
Therapies and interventions to approach uncertainty
In the literature included in this review, few studies deal with uncertainty towards the disease in the family caregiver. Additionally, the few studies reported have not been effective in the approach of this phenomenon. The most representative study62 applied an intervention to early- and late-stage cancer patients and their family caregivers. By means of three family visits lasting 90 minutes each and two telephonic sessions of 30 minutes each, it was found that the caregivers in the experimental group improved their negative assessment of the care provided after the intervention, but no changes were detected in the level of uncertainty towards the disease or in coping in either group. The author describes that these results were due to the fact that the research did not focus exclusively on patients in palliative care, who have special needs given the context of their advanced diseases, but also in patients with early stages of cancer.
The contributions of this research for the development of knowledge in Nursing are mainly related to describing the level of evidence around the five themes extracted for the review of the articles. As regards the characterization of uncertainty in the caregiver and the influencing factors, the findings allow the Nursing professionals to know the levels of uncertainty in palliative care and to identify some of its triggering factors. In the same sense, it describes the possibility of continuing researching the uncertainty levels by comparing them with other populations. In relation to the resources to manage uncertainty, the evidence shows that it is necessary to continuously train the caregivers on palliative care, as it is a basic resource for its management. Regarding the uncertainty assessment, the review shows the need to conduct systematic assessments of the level of uncertainty in the caregiver and, with this information, set forth therapies to approach it since, according to the results, few therapies and interventions have been set out to manage this phenomenon in the caregivers.
Conclusions
Uncertainty towards the disease of family caregivers of cancer patients in palliative care obeys multi-factorial causes such as knowledge on the disease, communication, recognition of their role in palliative care, fulfillment of needs, and social support. When caregivers experience uncertainty towards the disease, they are unable to determine the meaning of all its related events, that is, to assign definite values to objects and events, as well as to accurately predict consequences related to the disease, due to the scarcity of information and knowledge to do so.
The reviewed literature of a twenty-year period only reports a formal intervention for the management of uncertainty towards the disease. From this finding the need is interpreted of developing Nursing interventions that may offer accompaniment to the caregivers who experiment uncertainty towards the disease of patients in palliative care and, in the same way, impact on other variables, like their quality of life. Such interventions are necessary in contexts like the Colombian one, where the care provided to patients in palliative care and the accompaniment of their family caregivers are still precarious.















