Introduction
The new infection by coronavirus, Severe Acute Respiratory Syndrome (SARS-CoV-2), was described for the first time in December 2019 in the city of Wuhan, China1,2. The World Health Organization called this disease “COVID-19”, which is highly contagious, mainly because it presents aerosols (coughing or sneezing) from symptomatic or asymptomatic infected people as a form of transmission3.
SARS-CoV-2 belongs to the Coronaviridae family, composed of single-stranded RNA viruses that cause respiratory infections, which can vary from mild catarrhal symptoms to severe pneumonia4. In addition to SARS-CoV-2, six other types of coronavirus infect human beings, four of which cause minor respiratory infections (229E, OC43, NL63 and HKU1) and two causing epidemics (SARS-CoV and the Middle East Respiratory Syndrome coronavirus: MERS-CoV)5,6.
The symptoms of infections by coronavirus are non-specific, but they include fever, dry cough, myalgia, fatigue and dyspnea2,7, which can lead to severe hypoxemia requiring mechanical ventilation in up to 20 % of the cases7, as the virus binds to the angiotensin-converting enzyme 2 (ACE-2R) in human beings with greater affinity in the respiratory system8; however, it can affect other organs, such as the stomach, small intestine, kidney, adrenal glands, skin, parathyroid glands, heart, brain, liver and pancreas. This is due to the presence of ACE-2R in these organs, but with a lower density compared to the respiratory system9.
Mortality in infections by coronavirus is associated with age (generally people over 60 years old) and with the presence of chronic non-communicable diseases (CNCDs), with emphasis on systemic arterial hypertension (SAH), cardiovascular diseases, diabetes mellitus (DM) and chronic lung and kidney diseases; in addition, the presence of two or more comorbidities increases the mortality rates10,11.
The SARS-CoV pandemic in 2002 spread to 29 countries, lasting seven months, with 8,000 cases and a mortality rate of 10 %; while MERS-CoV in 2012 was detected in 27 countries, with approximately 2,500 cases and a mortality rate of 37 % 12. In SARS-CoV-2 in China, the reported mortality rate was 2.3 %, with no deaths in children under nine years old and 21 % occurring in individuals over 70 years old, of whom 10.5 % had some cardiovascular disease, 7.3 % had DM, 6.3 % had some chronic respiratory disease, 6 % had SAH and 5.6 % had cancer13.
Until the date of this study, there is not enough evidence to determine the effectiveness of treatments for COVID-19, although therapies used in previous pandemics with viruses from this same family are being tested, such as speculations on hydroxychloroquine, ritonavir, lopinavir, favipiravir, arbidol (umifenovir), oseltamivir, interferon and immunoglobulins, in the hope of finding an antigen against the disease14.
Thus, the fundamental role of Nursing in the care of people with CNCDs infected by coronavirus is unquestionable, which should be focused on the support of self-care, monitoring, follow-up and advanced care15.
Considering the magnitude of the infections by coronavirus, the previous experiences with viruses from this family, the possibilities, the strengthening and the knowledge about the preparation to care for the health of people with CNCDs, this review aims at identifying the implications, for Nursing, of pulmonary infections by coronavirus in people with CNCDs and to propose actions for care.
Materials and method
Review studies allow identifying the general perspective of a given subject matter, as well as the levels of evidence and the strength of the recommendations for applicability in the clinical practice16. Therefore, this study adapts to this type of review as it provides the basis for reflections and recommendations for the Nursing practice. In this sense, this is an integrative review based on five stages.
In the first stage, the guiding question was elaborated based on the PIC acronym, where “P” is Population (people with chronic diseases), “I” is Intervention (Nursing care) and “C” is Context (pulmonary infections by coronavirus). Thus, the following question was formulated: What are the implications for Nursing care that can be obtained from the literature on pulmonary infections by coronavirus in people with CNCDs in the last 10 years?
The search for studies took place between March 15th and March 30th, 2020, in Biblioteca Regional Virtual de Saúde (BVS), based on the following descriptors and Boolean operators: “doença crônica” AND “infecções respiratórias” AND “coronavirus humano 229E ” OR “coronavirus humano NL63 ” OR “coronavirus humano OC43 ”, and with the following search strategy: “chronic disease” AND “respiratory tract infections” AND “coronavirus OC43, human” OR “coronavirus NL63, human” OR “coronavirus 229E, human” in the Cumulative Index to Nursing and Allied Health Literature (CINAHL), National Library of Medicine (PubMed), Scopus and Web of Science databases.
A second search was conducted in the same databases and in the same period, with the following strategies: “doença crônica” AND “infecções respiratórias” AND “coronavírus humano 229E” OR “coronavírus humano NL63” OR “coronavírus humano OC43” AND “cuidados de enfermagem” and “chronic disease” AND “respiratory tract infections” AND “coronavirus OC43, human” OR “coronavirus NL63, human” OR “coronavirus 229E, human” AND “nursing care” (Chart 1).
Table 1: Search strategies to select the studies
| Portal/Databases | Strategy | Number of articles |
| BVS | “doença crônica” AND “infecções respiratórias” AND “coronavírus humano 229E” OR “coronavírus humano NL63” OR “coronavírus humano OC43” | 214 |
| “doença crônica” AND “infecções respiratórias” AND “coronavírus humano 229E” OR “coronavírus humano NL63” OR “coronavírus humano OC43” AND “cuidados de enfermagem” | 0 | |
| CINAHL, Scopus and Web of Science | “chronic disease” AND “respiratory tract infections” AND “coronavirus OC43, human” OR “coronavirus NL63, human” OR “coronavirus 229E, human” | 703 |
| “chronic disease” AND “respiratory tract infections” AND “coronavirus OC43, human” OR “coronavirus NL63, human” OR “coronavirus 229E, human” AND “nursing care” | 1,501 | |
| PubMed | “chronic disease” [Mesh] AND “respiratory tract infections” [Mesh] AND “coronavirus OC43, human” [Mesh] OR “coronavirus NL63, human” [Mesh] OR “coronavirus 229E, human” [Mesh] | 166 |
| “chronic disease” [Mesh] AND “respiratory tract infections” [Mesh] AND “coronavirus OC43, human” [Mesh] OR “coronavirus NL63, human” [Mesh] OR “coronavirus 229E, human” [Mesh] | 0 |
Source: Own elaboration based on research data.
The inclusion criteria for the articles were observational, cohort, cross-sectional, case-control, quantitative, and qualitative studies; adults with chronic non-communicable diseases with respiratory infection by viruses of the coronavirus family; published from 2010 to 2020, in Portuguese, English and Spanish, and available in full. Systematic, integrative, narrative and scoping reviews or mini-studies were excluded, as well as consensus and letters to the editor.
In the second stage, the duplicate articles were removed, the filters were applied, and a full reading of the titles and abstracts was performed, considering the eligibility criteria. A total of 26 articles remained for full-reading, of which 11 comprised the final sample, presented in the Preferred Reporting Systematic Reviews and Meta-Analyses of Studies (PRISMA) flowchart (Figure 1)17.
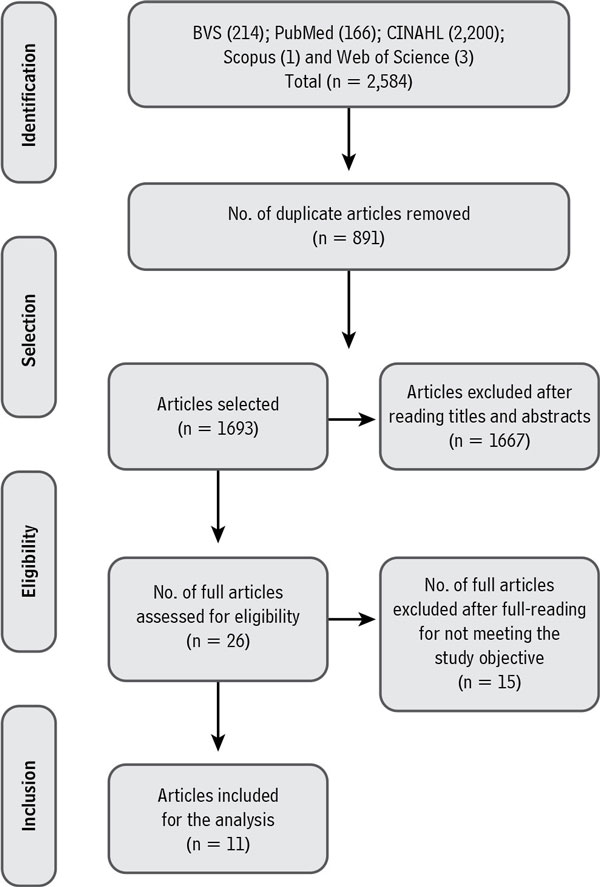
Source: Own elaboration based on research data.
Figure 1. Flowchart corresponding to the identification, selection and inclusion of the studies, prepared based on the PRISMA recommendation.
In the third stage, the data were collected and analyzed at two moments. At the first moment, the authors, year and place of the study, sample number, main results and level of evidence were verified according to the Oxford Center for Evidence-based Medicine18; secondly, categories inferred from the main results were elaborated for Nursing care directioning and actions.
In the fourth stage, the actions were separated into three levels: community care, hospital care and advanced care; the ones classified at the community level are those likely to be carried out in primary care, related to human resources, care for registered users and preventive training in the community; the actions at the hospital level by the Nursing team are the following: training, communication, diagnostic aid, and care according to the new guidelines and protocols for the treatment of infections by coronavirus; the third level is aimed at advanced care, such as training and using the best evidence in health care.
In the fifth stage, the care proposals were discussed with the current parameters established by the competent authorities for the management of COVID-19, in the search of possibilities for effective and safe Nursing care at all assistance levels, as a contribution to the health and nursing practice.
Results
The selected studies were retrospective, observational, prospective and case studies, with a quantitative approach; seven of them were from Saudi Arabia, three were from the United States and one was from South Korea, all in English with levels of evidence 2B, 2C and 4; none mentioned Nursing actions or care.
Regarding the prevalence of CNCDs, eight of the nine studies that addressed infection by the MERS-CoV strain reported SAH and DM; the other studies reported prevalence of chronic respiratory and cardiac diseases with infections by OC43 and 229E strains. However, it is not possible to establish a causal relationship of DM and SAH as risk factors, because they are also the two most prevalent comorbidities in the world19.
The most reported symptoms in MERS-CoV infections were fever, cough and dyspnea; while in the other strains, there was a predominance of nasal congestion and runny nose. It is to be noted that the male gender was predominant and, also, the age group between 30 and 70 years old, among the infected individuals. The mortality rates in the Intensive Care Unit (ICU) exceeded 70 % for MERS-CoV, affecting more men than women, aged between 50 and 70 years old. The non-survivors were longer-lived older adults, obtained higher scores in the Acute Physiology and Chronic Health Disease Classification System II (APACHE II) and in the Sequential Organ Failure Assessment Score (SOFA), and were prone to invasive mechanical ventilation interventions and vasopressor therapies at admission.
Chart 2presents the results of the analysis of the articles and the care proposals, separated by the three proposed action levels: community care, hospital care and advanced care.
Table 2: Results of the articles and of the proposals of Nursing actions for the clinical practice
| Level | Authors, years, place of publication and level of evidence | Directioning | Nursing actions | Means |
| Community care | Alraddadi et al., 2016, Saudi Arabia20, Level of evidence 2B Kim et al., 2016, South Korea21, Level of evidence 2B | Risk prevention and control Diagnostic aid Health promotion Education in health and self-management Life habits Environment Encouraging the prevention of vaccine-preventable diseases Training for the Primary Care health professionals | To identify suspected or confirmed cases of infection by coronavirus, based on the criteria and on the operational definitions for COVID-19 in frequent updates by the competent bodies. To assess community factors for the transmission chain: life habits, schooling, stereotypes and hereditary diseases, among others. To encourage people with CNCDs to follow the preventive respiratory measures related to vaccine-preventable diseases: education in health, vaccination, lifestyle change and treatment adherence. To inform the community about infection prevention, such as the importance of social isolation. To prepare for situations of catastrophes with dimensioning of personnel, space, supplies and service flow with referral and counter-referral. To identify possible limitations or barriers in access to health, evaluating the existing family health management programs, mainly verifying the mapping of older adults, pregnant and puerperal women, to provide them with care by means of Telemedicine and Telenursing. To conduct training and qualification of health professionals and the community, to improve sanitary practices in public environments with 70 % alcohol supply, encouraging hand washing. | Continuing education for the professionals. Teamwork. Adequate human, material and physical resources. Education in health for the community according to the needs resulting from the emergent diseases. |
| Hospital Care | Walsh et al., 2013, United States22, Level of evidence 2B Gorse et al., 2015, United States23, Level of evidence 2B Kim et al., 2016, South Korea21, Level of evidence 2B Amer et al., 2018, Saudi Arabia24, Level of evidence 4 Alqahtani et al., 2019, Saudi Arabia 10, Level of evidence 2B Al-Abdely et al., 2019, Saudi Arabia25, Level of evidence 2C | Diagnostic aid Treatment aid Training for the health professionals Access to the health service/ network, management in health and public health Mental health | To guide the support and welcoming team regarding the signs and symptoms of respiratory diseases, to indicate the use of masks from the main entrance of the hospital institution. To carry out screening, with initial anamnesis focused on prioritizing the main topics to identify the respiratory disease caused by the coronavirus, such as asking about travels to countries where there is local transmission, contact with suspected or confirmed cases, age (with relevance to greater risk of the severe form in older adults), people with immunological impairment, comorbidities (SAH, Types 1 and 2 DM, heart disease, kidney disease and lung disease). To identify and investigate, in people with CNCDs, signs and clinical complaints reported, time and duration, to seek information from previous appointments in the medical record to survey situations of uncontrolled diseases. To use the isolation protocol provided for in the screening room in the care for communicable respiratory diseases. To identify and prevent adverse events, with reorientation of flow, staff, supplies, space and time in the cases of respiratory disease caused by the coronavirus, from the initial approach to the outcome of the case in discharge for any type. To monitor signs and symptoms of respiratory complications, performing daily physical examinations or through clinical involution, aimed at recording the clinical signs, such as current and past temperature using a daily map, cardiac and respiratory rates together with the findings, systemic blood pressure, peripheral capillary perfusion, central and peripheral pulses, use of accessory muscles, presence of cyanosis, pulmonary auscultation and its findings. To guide the family members and other professionals about the care for infection prevention, restricting access or the number of visitors per bed; to provide the family members with access to the patient’s information through health status reports following the institution’s protocol. To use tools to assess the risk of complications through Nursing diagnoses and interventions, aimed at the cases of respiratory diseases caused by coronaviruses, such as risk of shock, multiparametric monitoring and standard precautions, droplets and aerosols. To identify suspected or confirmed cases of infection by coronavirus and to appropriately isolate the cases through multidisciplinary screening, as well as evaluation of exams according to the existing clinical protocol. To encourage the proper use of personal protective equipment (PPE: gloves, masks, aprons, goggles and others) for professionals, patients and family members. To conduct training sessions for the health professionals, to improve hospital practices. To ensure the proper collection, handling and transportation of the diagnostic samples, defining the management of the responsibilities of each professional. Environmental hygiene, enabling effective communication between the general service professionals and the Nursing team about the accommodation and transport of patients with respiratory disease caused by the coronavirus. To prevent and identify psychological or emotional changes in the patient, to provide quality dialog between the professionals and the patient, promoting the effective participation of the Psychology team. To prevent adverse events and complications. To pay attention to the humanization of care. | Evidence-based practices. Use of guidelines, bundles and protocols specific to the institution and based on scientific evidence for the care of patients infected with coronavirus. Continuing education for health professionals. Adequate human, material and physical resources. To promote effective communication within the team. |
| Advanced care | Arabi et al., 2014, United States26, Level of evidence 4 lmekhlafi et al., 2016, Saudi Arabia27, Level of evidence 2B Ko et al., 2016, Saudi Arabia28, Level of evidence 2B Garout et al., 2018, Saudi Arabia29, Level of evidence 2B | Constant monitoring of the patient, the team, and the environment Training in advanced care for the health professionals Diagnostic aid Treatment aid | To provide advanced Nursing care, according to the legislation in force. To prevent adverse events and complications. To articulate the team members in the provision of care. To use risk assessment tools for complications. To use techniques to improve the respiratory conditions, to meet the care needs in all systems and to prioritize humanization of care. To ensure adequate collection, handling and transportation of the diagnosis samples. To provide guidelines for waste management. To monitor the patient’s vital signs, level of consciousness and nutrition. | Advanced Nursing practices based on scientific evidence (application and training). |
Source: Own elaboration based on research data.
Discussion
The actions proposed for the community level by the study carried out in Saudi Arabia are related to the definition of the probable case as one that has an inconclusive laboratory result, and that of a confirmed case of infection by a conclusive laboratory test, regardless of symptoms. The possible actions and responsibilities of the Nursing Staff at the community level are the identification of suspected cases of infection by coronavirus, based on the operational definition criteria for infections by this virus, similar to those currently established by the Ministry of Health and by competent bodies for COVID-19, defining as suspected cases those with fever, at least one respiratory symptom, and with a history of travel to areas with local transmission in the last 14 days or contact with a suspected or confirmed case of coronavirus in the same period20,30.
The Brazilian Ministry of Health, the National Health Surveillance Agency (Agência Nacional de Vigilância Sanitária, ANVISA) and the Brazilian Association of Professionals in Infection Control and Hospital Epidemiology have established the following as possible Nursing actions in the community: assessment of the life habits, underlying diseases and other factors that influence transmission; promotion of education and preventive measures in health, immunization, lifestyle changes and treatment adherence, especially for people with CNCDs; it is also noteworthy to identify the limitations in access to the health services, mainly in the aged population and pregnant and puerperal women, cases in which Telemedicine and Telenursing can be promoted30-32.
In this sense, we considered that, in addition to the above, Nursing must include strengthening of education in health for the community, since the population is informed through the social networks, which, on many occasions, publish false data, which contributes to misinformation, causing anxiety and other psychiatric disorders associated with pandemics33. In Brazil, there has been an increase in the Telenursing activities to assist the community with information related to the COVID-19 pandemic34; however, it becomes necessary to encourage universities and other educational institutions to lead the community to carry out practices based on current scientific evidence.
It is also imperative to establish guidelines for home care after hospital discharge of the infected people: such care includes verification of the home environment, to ensure care and compliance with the preventive measures so that other people are not contaminated (hand hygiene, respiratory hygiene with the use of tissues or disposable paper and environmental cleaning); assessment of the possible environmental safety problems (places with risk of falls, presence of children in the house, airy and ventilated environments); and provision of health education support for the person and his/her caregivers35.
In a study on the lessons learned from COVID-19, the authors indicated that the most important measures to slow down the spread of respiratory viruses in the community include closing mass meeting places (schools, libraries, shopping malls and cinemas), suspending all social events (sports, celebrations and meetings) and temperature screening at airports, bus stations and entrances to hospitals, banks or courts36.
In turn, concerning care at the hospital level, aged individuals and/or people with comorbidities infected by coronavirus must be prioritized, given the higher rate of complications and mortality in this population10,22,23,25. The main deficits that led to viral spread during previous coronavirus pandemics were reported, namely: late diagnosis, lack of isolation of suspected cases, lack of regulation of family visits, lack of facilities and equipment necessary for care, overcrowded emergency rooms with inadequate ventilation, problems with the screening systems, and lack of education on the infection control practices among the health professionals21,24.
Corroborating the reflections of this review regarding Nursing care, other studies highlight the actions at the hospital level, such as guidelines for the team regarding the infection signs and symptoms; correct use of masks and other PPE (gloves and goggles) from the moment they enter the health service, screening of the suspected cases, especially older adults, people with comorbidities and/or immunocompromised patients; the protocol for the isolation of suspected cases at admission; identification and prevention of adverse events through risk management with adequate equipment, supplies, space and time to deal with the cases; constant monitoring of vital signs; and recording of the clinical evolution37.
The guidelines to family members and health professionals about the care and preventive measures for the infection are directed towards the restrictions on the number of visitors, correct hand washing and use of PPE. The professionals are encouraged to appropriately collect, handle and transport the samples for diagnostic confirmation, as well as to periodically ensure environmental hygiene with appropriate disinfectants, as the virus permanence time on surfaces can reach 72 hours; as well as to prevent and identify possible psychological and emotional crises in the people assisted or their family members, articulating the effective participation of the Psychology team30.
For the control and treatment of COVID-19, the Ministry of Health emphasizes the provision of masks, alcohol dispensers (in gel or solution) and other means for handwashing when entering the institution. The importance of keeping the environments ventilated and disinfecting surfaces and equipment used in care is also highlighted. In the case of transfers, the reference center must be notified in advance about the conditions and status of the suspected or confirmed case, to provide private environments with adequate ventilation and isolation30.
The ANVISA recommends other preventive measures for viral transmission by coronavirus, which were not identified in the articles included in this review, namely: use of cloth masks for asymptomatic people and of surgical masks for symptomatic people and health professionals throughout their stay in the institution; and distance of at least one meter between individuals. Emphasis is added to the implementation of diagnostic protocols, special care and isolation, which allow for the early identification and proper management of suspected COVID-19 cases, as well as a contingency plan with actions that are necessary to face critical situations in the health services32.
Pandemics require a Nursing leadership that distributes roles and maintains effective communication with the multidisciplinary team. This is because education on infection control practices among health professionals is a fundamental aspect in the preparation for public health crises, in which it is urgent that everyone knows and enforces the national guidelines in a coordinated manner, adapted to the institutional conditions for adequate assistance21.
Regarding care in the ICU, it is highlighted that the complications due to infections by coronavirus are associated with multiple organ failure and occur mainly in men, older adults and with comorbidities; among the frequently reported are SAH, DM and kidney failure38,39.
In these cases, the recommendations were use of corticosteroids, strict monitoring of biochemical parameters for renal replacement therapy, individual isolation within the ICU and adequate mechanical ventilation adjustments, monitoring using laboratory tests for diagnostic and prognostic parameters, maintaining strict hand hygiene measures, environmental disinfection, and continuous monitoring of the vital signs26-29.
It is considered that the possible Nursing actions in the advanced care required in the ICU are articulation and actions together with the members of the health team, correct management of contact isolation, prevention of adverse events with the use of tools to assess risks, continuous monitoring and vital signs records, guidance to the team members on the correct use of PPE, as well as the removal and disinfection of reusable equipment and the disposal of others40.
Conserning the measures to be adopted in the hospital environments to prevent and/or reduce transmission of respiratory infections by coronavirus, isolation for at least 14 days is indicated among those infected, as well as scheduled discharge after two negative Reverse Transcription Polymerase Chain Reaction (RT-PCR) tests, with an interval of at least 24 hours and/or resolution of fever and respiratory symptoms in the last 72 hours31,41. Consequently, it becomes fundamental that the health professionals, mainly nurses, are trained and qualified to manage the challenges imposed by the disease.
The training and qualification of nurses must follow the current technological evolution worldwide. This trend can provide opportunities for the use of advanced resources and improve knowledge and reasoning for the care practice42, such as clinical simulation, which enables the representation of a real event to practice, learn and safely assess the care provided. Among the advantages of this method is the reduction in the time needed to develop skills, considering that the training can be repeated as many times as necessary, in addition to stimulating clinical reasoning, leadership skills, teamwork and the development of skills for advanced Nursing practices based on scientific evidence43,44.
The need to implement evidence-based Nursing practices is highlighted, which is a clinical decision-making process grounded on the best available evidence, based on research, clinical experience, preferences of the person assisted and available resources, to improve quality of care45.
The advanced Nursing practices supported by evidence-based practices must be applied in the care of people infected by coronavirus in ICUs. The prone position has been a technique used since the 1970s, to increse arterial oxygenation, redistributing pleural pressures to make lung volumes more homogeneous, and improving alveolar recruitment in the collapsed dorsal areas. In the COVID-19 pandemic scenario, this technique has been used in severe cases of acute respiratory infection by SARS-CoV-2 and as a prior protective measure46,47.
Nurses must minimize the risks of the prone position by managing and preventing problems, such as loss or obstruction of the tracheal tube, severe hypotension, bradycardia and desaturation associated with fluid movement and changes in the intrathoracic pressure, pressure ulcers, corneal ulcers, facial, eyelid or conjunctival edema, regurgitation or intolerance to enteral nutrition, muscle spasms and brachial plexus injury46.
In Nursing care in the ICU, attention to the basic hygiene needs and to the comfort of the people assisted must be considered, which should be established in a joint and orderly manner with the multidisciplinary team, within the person’s clinical conditions and, if possible, it represents the opportunity for nurses to identify systemic disorders, especially of the skin. During these procedures, there must be continuous monitoring to recognize any change in the vital signs and to prevent or minimize the adverse events48.
In addition to advanced care and prevention of complications, humanized care and psychological monitoring of the infected people and their family members must be considered. The professionals can facilitate communication through virtual technologies and phone calls, keeping current and accurate information on the clinical conditions, respecting the family values and beliefs, understanding people’s fears, anxieties and uncertainties in the context of the pandemic49,50.
In this sense, it becomes important to provide care for people with no expectations of cure, such as the use of analgesics to relieve pain and discomfort, personal hygiene and minimizing adverse events. Clarity, ethics and decision-making together with the family members are highlighted, respecting the acceptance time and providing them with emotional support51.
The limitations of this study include the dates proposed for searching the articles, the difficulty in finding guidelines for Nursing care in the literature, the reduced number of articles that met the inclusion criteria and were selected for the final analysis, the scarce literature found on coronavirus strains other than those that cause MERS-CoV, and the research period of the articles used (from 2010 to 2020), considering that the reports of pandemics by coronavirus strains date back to the beginning of the present millennium.
Conclusions
The results of this article highlight the need for evidence to guide health and nursing professionals in dealing with emergency public health situations. The previous SARS-CoV and MERS-CoV pandemics offered clues to control and optimize the care of people infected by these viruses, although this knowledge was not widespread in many countries. The absence of guidelines for care leads to inappropriate solutions, unsafe practices, and mass spread of the disease.
Undoubtedly, evidence-based attitudes and practices strengthen and encourage the health team in the fight against pandemics. For this reason, the continuous education of the health and nursing teams, the establishment of protocols, workflows and standardized instructions and prevention and control measures for the community with good levels of evidence are important to ensure life and environmental control with the reduction of transmissibility, complications and death caused by the disease, with the guarantee of ethical and quality care.















