Introduction
In December 2019, the World Health Organization was alerted of several cases of pneumonia in Wuhan city, in the Hubei province of the People's Republic of China, which was a novel strain (type) of coronavirus that had not been previously identified in humans. In January 2020, the Chinese authorities confirmed that they had identified a novel coronavirus strain 1. In Brazil, the first case of the disease caused by the novel coronavirus (COVID-19) was reported on February 26, 2020.
The increasing number of cases caused by this disease has led to changes in work organization, particularly that of healthcare personnel providing care to patients suspected or confirmed to have the disease. Nursing and medical personnel have been subjected to long working hours, overtime, and a rushed pace, increasing social, psychological, and physical risks, including coronavirus infection 2. Thus, this disease can be considered the first new work-related disease 3.
COVID-19 high transmissibility and potential for aggravation, the limited availability of personal protective equipment (PPE), the lack of adequate training to respond to outbreaks of highly infectious diseases 4, and the inefficient use of PPE promote better working conditions and the implementation of biosafety measures for healthcare personnel a priority. Brazil is already considered the world leader in nursing personnel deaths due to COVID-19; according to data from the International Council of Nursing, the country represents 38 % of the recorded deaths of nursing personnel in the world 5.
Along with the high risk of infection, COVID-19 has been associated with other health hazards for healthcare personnel. Damage to health is defined as all forms of losses or injuries caused by work-related demands and experiences, designated as physical, psychological, and social 6. It is noteworthy that the increased frequency and time of PPE use and the application of other infection prevention measures, such as hand washing, have determined the occurrence of damage to the physical well-being of personnel, such as skin injuries, pressure spots, headaches 7, dermatitis, eczema 8, among others.
In addition, the uncertainties surrounding the disease, along with the stress and concern experienced in the work environment when responding to COVID-19, have affected the sleep quality of healthcare personnel 9, manifested as insomnia, daytime sleepiness, and nightmares, among others 10, which can compromise their well-being and productivity.
The literature has extensively evidenced the damage to the mental and psychological health of personnel who are responders to COVID-19 11-13. However, there are knowledge gaps regarding these people's physical well-being. In this context, it is crucial to broaden the knowledge on the subject to develop measures that improve the work environment, implement biosafety measures, and provide occupational health. Thus, this study aims to highlight the impact of responding to COVID-19 on the physical well-being of nursing and medical personnel.
Method
This integrative literature review is structured from the following steps: The development of the research question; search and selection of primary studies; data extraction of the selected studies; critical evaluation of the studies included in the integrative review; synthesis of the results and review presentation 14.
The research question was developed according to the PICo strategy, where P stands for population; I for interest; and Co for context. The study population consisted of nursing and medical personnel; the interest was related to physical well-being; the context was related to responding to COVID-19. Thus, the research question established was: What is the scientific evidence on the impact of responding to COVID-19 on the physical well-being of nursing and medical personnel?
Regarding the search and selection of studies, we included primary studies that addressed the impact of responding to COVID-19 on the physical well-being of nursing and medical personnel and were available online in Portuguese, English, and Spanish. Letters, editorials, experience reports, reports, and publications already selected in the search in another database that failed to answer the research question were excluded.
The search was conducted from July 10 to 16t, 2020, via the Capes Journal Website, through the Comunidade Acadêmica Federada. The databases accessed were the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Latin American and Caribbean Health Sciences Literature (LILACS), Web of Science (Clarivate Analytics), SciVerse Scopus (Scopus), and the National Library of Medicine (PubMed).
For the search, the following strategy was developed: ("Covid-19" OR "2019-ncov" OR "2019 novel coronavirus disease" OR "covid19" OR "SARS-CoV-2 infection" OR "coronavirus disease 2019") AND ("health personnel" OR "health care providers" OR "healthcare providers" OR "healthcare workers" OR "medical and nursing staff" OR "medical staff" OR "nursing staff"). This strategy was adjusted to each base considering their specifications. In LILACS, the strategy was also used with the variations of terms for the Portuguese language.
All documents found in the databases were imported into Mendeley reference management software. It is noteworthy that two independent researchers searched and selected materials simultaneously, and, in case of disagreement, another researcher participated in reaching a consensus. The recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were adapted for this review.
On the Mendeley software, after excluding duplicates, the documents were pre-selected by reading the titles and abstracts. From the total of 3,200 articles found, 668 duplicates and 2494 studies were excluded for failing to answer the research question and fitting the exclusion criteria. In total, 25 reports were included in the review.
The information from the articles included in the review was extracted using an instrument developed by the authors with the following items: Title, authors, objective, method, results, evidence level, and observation. Initially, members of the research team in which the authors participated applied the instrument to selected articles on the topic to prepare the researchers for data extraction.
The critical analysis of the studies consisted of a detailed reading and comparison of findings and checking whether the methodology used accomplished the study objective. At this stage, the evidence level was also categorized. For diagnostic, treatment, and intervention studies, the following classification was followed: Level 1 - systematic review or meta-analysis; Level 2 - randomized controlled trials; Level 3 - non-randomized controlled trials; Level 4 - case-control or cohort studies; Level 5 - systematic reviews of qualitative or descriptive studies; Level 6 - qualitative or descriptive studies, and Level 7 - opinions or consensus. Research related to etiology and prognosis was classified as follows: Level 1 - synthesis of cohort or case-control studies; Level 2 - case-control or cohort studies; Level 3 - synthesis of descriptive studies; Level 4 - qualitative or descriptive studies; and Level 5 - opinions or consensus 15.
The results were presented descriptively and in tables for better visibility for readers. Subsequently, there was a synthesis of the main findings, interpretation, analysis, and comparison between studies, inferences, and literature discussion.
Regarding the ethical aspects, the definitions and concepts followed by the authors of the analyzed works were respected and, as this is an integrative literature review, this research was not submitted to the ethics committee.
Results
Based on the articles search and selection process, 25 were included in the review, as shown in Figure 1. Of these, 52 % (n = 13) addressed coronavirus infection and related factors as an impact on the physical well-being of nursing and medical personnel, 28 % (n = 7) covered the sleep quality and predictors, and 20 % (n = 5) contemplated the damage resulting from PPE use or other infection prevention measures.
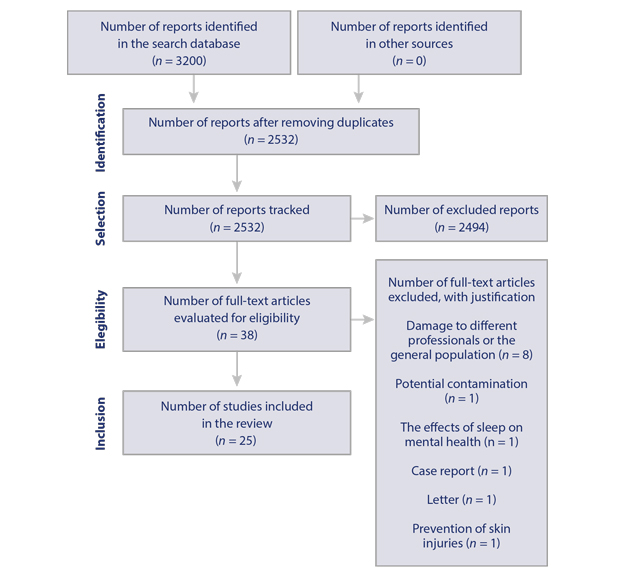
Source: Own elaboration based on research data.
Figure 1 Flowchart of the selection and inclusion process of primary studies in the review adapted from PRISMA
The evidence on coronavirus infection suffered by nursing and medical personnel and related factors was produced predominantly from cross-sectional and cohort studies, half of them (53.8 %) with Level 4 evidence, in countries such as China (46.2 %) and Italy (23.1 %), as shown in Table 1.
Table 1 Evidence synthesis on coronavirus infection suffered by nursing and medical personnel and related factors. Santa Maria, Rio Grande do Sul, Brazil, 2020
| Authors | Research location (service, country) | Study type | Evidence level | Main results |
|---|---|---|---|---|
| Zheng L, Wang X, Zhou C, Liu Q, Li S, Sun Q, et al. | Several hospitals in Wuhan, China | Cross-sectional | 4 | More than half of the infected individuals were nurses working in a general hospital |
| Chu J, Yang N, Wei Y, Yue H, Zhan F, Zhao J, et al. | Tongji Hospital, China | Cohort | 2 | More than half of the positive cases were men working in clinical sectors |
| Lai X, Wang M, Quin C, Tan L, Ran L, Chen D, et al. | Tongji Hospital, China | Cross-sectional | 4 | There is an infection rate of 1.1 % among staff; more than half were women |
| Garzaro G, Clari M, Ciacan C, Grillo E, Mansour I, Godono A, et al. | University hospital, Italy | Series of cases | 4 | Providing care to patients did not increase the risk of infection, but sharing the work environment did |
| Dabholkar YG, Sagane BA, Dabholkar TY, Divity S | Tertiary referral hospital for COVID-19, India | Cross-sectional | 4 | Forty healthcare personnel were infected in two months since the first case in the hospital. Almost half of the staff felt they had been infected at work, and 15 % reported unprotected exposure to a COVID-19 positive patient |
| Fusco FM, Pisaturo M, Iodice V, Bellopede R, Tambaro O, Parrella G, et al. | The emergency room of two clinics, Italy | Cohort | 2 | There is a general prevalence of 3.4 % of coronavirus infections |
| Chen CC, Chi CY | Nanjing Drum Tower Hospital, China | Cohort | 4 | There is a seroprevalence of 17.1 % of personnel (initial outbreak in China). There is a higher prevalence in those with exposure time > 30 min within one meter of contaminated patients. The use of masks was associated with a reduced risk of seroconversion |
| Felice C, Di Tanna GL, Zanus G, Grossi U | Research carried out via social media, Italy | Cross-sectional | 4 | Twenty-five percent of the staff presented with COVID-19 symptoms. Of the 25 % tested, one-third had symptoms; 18 % tested positive. Only 22 % considered the PPE adequate in quality and quantity. |
| Kluytmans-van den Bergh MFQ, Buiting AGM, Pas SD, Bentvelsen RG, van den Bijllaardt W, van Oudheusden AJG, et al. | Two teaching hospitals, the Netherlands | Cross-sectional | 6 | COVID-19 prevalence in 6 % of staff; 3 % with a travel history to China and Italy, and 3 % had contact with a COVID-19 positive patient |
| Barrett ES, Horton DB, Roy J, Gennaro ML, Brooks A, Tischfield J, et al. | Two university hospitals in New Jersey, United States | Cohort | 2 | Higher infection rates among personnel who spent more time in patient rooms, having increased contact with suspected or confirmed COVID-19 patients |
| Ran L, Chen X, Wang Y, Wu W, Zhang L, Tan X | COVID-19 referral hospital, Wuhan, China | Cohort | 2 | The risk of infection increases when personnel contact COVID-19 positive family members, fail to perform hand hygiene properly, use inappropriate PPE, and work for more than 15 hours in high infection risk areas |
| El-Boghdadly K, Wong DJN, Owen R, Neuman MD, Pocock S, Carlisle JB, et al. | Multicenter prospective cohort study carried out in 17 countries | Cohort | 2 | Ten point seven percent of the providers who assisted in intubating patients suspected or confirmed COVID-19 had symptoms. Women were at a significantly higher risk of developing the disease |
| Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D | Zhongnan Hospital in Wuhan, China | Cross-sectional | 4 | Social network density was higher in infected staff. Touching the cheek, nose, and mouth during work considerably raised the rate of coronavirus infection, while wearing PPE in the adequate size and timing was a protective factor. |
Source: Own elaboration based on research data
Still, regarding the infection among healthcare personnel, the studies identified that sharing the environment is considered a risk factor for infection and the time of exposure and participation in the intubation of patients with COVID-19. The use of PPE, especially masks, is a protective factor.
Table 2 explains the properties of evidence and the main results regarding sleep quality and predictors in nursing and medical personnel who respond to COVID-19. It can be noted that almost all were conducted in China using cross-sectional designs, with Level 4 evidence.
Table 2 Evidence synthesis on sleep quality and predicting factors in nursing and medical personnel who respond to COVID-19. Santa Maria, Rio Grande do Sul, Brazil, 2020
| Authors | Research location (service, country) | Study type | Evidence level | Main results |
|---|---|---|---|---|
| Wu K, Wei X | A referral hospital for COVID-19 and one that is not, China | Non-randomized clinical trial | 3 | Frontline medical personnel have worse sleep quality compared to those who are not |
| Huang Y, Zhao N | The Chinese population, China | Cross-sectional | 4 | Compared to other occupational group, healthcare personnel had a higher rate of poor sleep quality |
| Zhuo K, Gao C, Wang X, Zhang C, Wang Z | The Children's Hospital, Wuhan Central Hospital, and other COVID-19 referral hospitals, China | Cross-sectional | 4 | Medical and nursing personnel with insomnia showed clear signs of comorbid sleep apnea attributable to stress |
| Wang Y, Wu Y, Cheng Z, Tan X, Yang Z, Zeng X, et al. | Children's Health Center in Wuhan, China | Cross-sectional | 4 | Thirty-eight percent of the participants had sleep disturbances, regardless of whether being an only child, exposure to COVID-19 patients, and depression |
| Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. | Chinese hospitals, China | Cross-sectional | 4 | More than one-third of the medical team suffered insomnia during the COVID-19 outbreak. Mid-level personnel, medical personnel, personnel working in isolation units, and those concerned about being infected or controlling the COVID-19 outbreak were at higher risk of experiencing insomnia |
| Xiao H, Zhang Y, Kong D, Li S, Yang N | Provinces responding to COVID-19, China | Cross-sectional | 4 | These professionals' sleep quality was poor. The levels of social support affected sleep quality. Stress was negatively associated with sleep quality |
| Jahrami H, BaHammam AS, AlGahtani H, Ebrahim A, Faris M, AlEid K, et al. | Facilities belonging to the Ministry of Health, Bahrain | Cross-sectional | 4 | Seventy-five percent of the professionals have poor sleep quality; 85 % had moderate-severe stress. The female sex and professional background (not being a physician) were predictors of poor sleep quality and stress |
Source: Own elaboration based on research data
The studies presented in Table 2 suggest that, in responding to COVID-19, these professionals had worse sleep quality than others, primarily due to their concerns regarding the disease, stress, other mental disorders, and being female.
Table 3 presents the synthesis of the articles that contemplated the damage stemming from the use of PPE or other measures to prevent coronavirus infections. It is noted that the studies were conducted in different countries, including one that included professionals from 90 countries. All used the cross-sectional study methodology with Level 4 evidence.
Table 3 Evidence synthesis contemplates the damage stemming from PPE or other measures to prevent coronavirus infections. Santa Maria, Rio Grande do Sul, Brazil, 2020
| Author | Research location (service, country) | Study type | Evidence level | Main results |
|---|---|---|---|---|
| Ong JJY, Bharatendu C, Goh Y, Tang JZY, Sooi KWX, Tan YL, et al. | National University Hospital, Singapore | Cross-sectional | 4 | Eighty-one percent of the personnel had headaches due to PPE use (N95 face mask and goggles), which were associated with a preexisting diagnosis of headache and PPE use > 4h per day |
| Guertler A, Moellhoff N, Schenck TL, Hagen CS, Kendziora B, Giunta RE, et al. | Surgical Center and Intensive Care Unit for COVID-19 at the Ludwig Maximilian University Hospital of Munich, Germany | Cross-sectional | 4 | There is a prevalence of symptoms associated with acute hand dermatitis in 90.4 % of personnel. The pandemic caused a significant increase in hand washing, disinfection, and hand creams |
| Tabah A, Ramanan M, Laupland KB, Buetti N, Cortegiani A, Mellinghoff J, et al. | An international study carried out with healthcare providers working in 90 different countries | Cross-sectional | 4 | For 52 % of the providers, at least some standard PPE was unavailable, and 30 % reported reusing single-use PPE. Damage stemming from PPE use: Heat, thirst, pressure spots, headaches, inability to use the bathroom, and extreme exhaustion |
| Jiang Q, Song S, Zhou J, Liu Y, Chen A, Bai Y, et al. | One hundred sixty-one hospitals, China | Cross-sectional | 4 | The general prevalence of skin injuries is 42.8 %. Two or more skin injuries and injuries with multiple locations affected 27. 4 % and 76.8 % of the providers, respectively. Only 45 % of the injuries were treated |
| Jiang Q, Liu Y, Wei W, Zhu D, Chen A, Liu H, et al. | One hundred sixty-one hospitals, China | Cross-sectional | 4 | There is a high prevalence of PPE-related pressure injuries among the medical team. The risk factors for injury were sweating, being male, using level 3 PPE (N95/KN95 respirators with goggles or face masks and protective gowns, latex gloves, and shoes), and extended time of use |
Source: Own elaboration based on research data.
The results in Table 3 demonstrate that, albeit having their respective functionality, the use of PPE and other protective measures against coronavirus infection can also cause damage to the well-being of personnel, most notably headaches, skin injuries, and exhaustion.
Discussion
The available evidence on the impact of responding to COVID-19 on the physical well-being of nursing and medical personnel refers particularly to coronavirus infection, quality of sleep, and the consequences of using PPE or other infection prevention measures. These were mainly found to be cross-sectional type studies, with Level 4 evidence carried out in China.
The low evidence level is justified by the fact that COVID-19 is a novel disease that requires the development of quick and low-cost research, which could direct healthcare and generate new hypotheses for further studies. Therefore, the cross-sectional study methodology, which combines these characteristics 16, was the most used.
The high number of studies of Chinese origin can be explained by the fact that the coronavirus outbreak started in that country with an imminent need for evidence to support clinical practice.
Coronavirus infection among nursing and medical personnel and related factors
The COVID-19 pandemic has been affecting the general population. However, frontline healthcare providers are more susceptible to infection 17. During the initial coronavirus outbreak in China, the healthcare services were unaware of how the virus was transmitted and the necessary precautions. Soon, an increasing number of infected healthcare providers was identified, with a prevalence ranging from 1.1 % 18 to 17.1 % 19. In this context, research in that country found that 40 healthcare providers were infected within two months since the first case in the hospital; half of them became infected at work, and 15 % through unprotected exposure to patients with COVID-19 20.
Even after learning about what was being experienced in China, infections among healthcare providers were still significant in other countries. In Italy, a study in two medical clinics found an overall prevalence of 3.4 % 21, but in a nationwide study, 18 % of all healthcare providers had the disease 22. In the Netherlands, a study found that 6 % of providers had COVID-19 with a travel history to China and Italy or contact with a COVID-19 patient 23.
Regarding infections by contact with patients, studies have found that the infection rates were higher among personnel who worked for more than 15 hours in high-risk areas for infection 24 and who had increased contact with suspected or diagnosed COVID-19 cases 25. A study indicated a higher prevalence of the disease among personnel exposed for more than 30 minutes within a meter of patients and among those in close contact with patients with a higher viral load 26. This evidence may justify the results of a study that identified that 52.06 % of infected personnel were nurses, and 33.62 % were physicians 27.
Sharing the work environment and social network density 28,29 have also been associated with increased risk for coronavirus contamination, as demonstrated in a study conducted in Italy, where sharing a work environment represented an additional 2.63-fold risk of infection. The same study showed that non-medical services had an increased risk of infection (OR = 4.23), as did administrative staff (OR = 5.77) 28. Among the personnel who are a source of infection, those involved in managerial activities with increased human contact were the greatest COVID-19 disseminators 28.
In this same line, another Italian study found that coronavirus infections occurred in personnel who constantly worked the same shifts 21. This data emphasizes the need for infected personnel to be granted leave from their work environment to prevent the infection of their co-workers and patients 30. In Brazil and other countries, thousands of healthcare providers have been relieved from their professional activities because they have become infected 31.
Standard infection prevention measures that were disregarded also elevated the risk of infection. Research has shown that inadequate hand washing before and after contact with patients 24 and touching the cheek, nose, and mouth during work 29 were associated with infection among healthcare personnel. These issues emphasize the need for permanently training nursing and medical personnel regarding infection prevention, including orientation on hand-washing and self-care.
In the context of medical procedures, research has indicated that performing or assisting with intubation is a cause of COVID-19 among medical personnel. Although most providers were wearing PPE (caps, N95 masks, gloves, goggles), 10.7 % experienced the disease symptoms up to 32 days after an intubation procedure. Women were at a higher risk of developing the disease 32. It is noteworthy that this procedure produces aerosol and requires the adequate use of PPE. The high risk faced by women of being infected with COVID-19 supports further research into the influence of sex on infection with this disease.
The use of PPE in the adequate size and timing was considered a protective factor against infection 24,29, especially masks 19. However, an Italian study showed that only 22 % of the personnel considered the PPE adequate in quality and quantity 22. Another study indicated a higher number of infected people originated from clinical settings, where surgical masks were more common than that N95, which was prioritized for professionals working in fever clinics 33. The difficulties in accessing and using adequate PPE are a global problem contributing to professionals' exposure to the coronavi rus and the contamination of patients, other professionals, family members, and communities 34. The guarantee of safe conditions for professional practice requires management strategies regarding resource optimization and allocation.
Given the above, it is inferred that the response to COVID-19 by nursing and medical personnel increased the risk of coronavirus infection in this population, primarily due to the time in contact with infected patients, sharing the work environment, social and work contact, disregard for infection prevention measures, participation in intubations, and inadequate use or lack of PPE. The active search and mass testing of professionals for disease diagnosis promote occupational safety and standardize the protection of these professionals when performing procedures 34. Furthermore, the results also indicate the need for further research on the virus and the disease; the management of health services to promote measures to reduce the exposure of professionals; training related to care for the prevention of infections, and the provision of PPE.
Sleep quality of nursing and medical personnel responding to COVID-19
Sleep is a physiological process considered essential for maintaining physical and mental health. When exposed to stressful situations, individuals can manifest sleep suppression and increased wakefulness, which favors the occurrence of insomnia (difficulty falling asleep, maintaining sleep, and waking up early), drowsiness and daytime dysfunction, and nightmares, among others 10. In this context, the COVID-19 outbreak has triggered a more significant negative impact on the sleep quality of healthcare providers compared to other occupational groups 35.
The prevalence of poor sleep quality among nursing and medical personnel ranged among the studies reviewed from 36.1 % 36 to 100 % 37. A Chinese national study identified that almost one in four healthcare providers had sleep disorders and a high risk for developing psychological disorders and mental illnesses 35.
Other studies highlight that psychological/mental factors interfere with sleep quality. A study found an independent association between sleep disturbance, depression, and exposure to patients with COVID-19 36. Similarly, a study found that anxiety levels were associated with stress, negatively impacting self-efficacy and sleep quality 38. A study corroborates these findings by showing that somatization, depression, terror, and mental state affect sleep time and efficiency 37.
Stress in healthcare providers has also been correlated to insomnia with comorbid sleep apnea. Professionals with moderate to severe sleep apnea-hypopnea syndrome had higher insomnia severity and worse mental states 39. Additionally, a study has shown that the female sex and professional background (not being a physician) were predictors of poor sleep quality and stress combined 40. Both poor sleep quality and stress in healthcare providers may impair their cognitive abilities and decision-making skills 41, requiring managers' awareness to implement measures to promote their well-being.
Furthermore, among the factors related to sleep quality, it was identified that low educational level (middle or lower), concern regarding coronavirus infection, extreme uncertainty about effective COVID-19 control, working in an isolated environment 42, and perceived lack of psychological support are risk factors for insomnia 38,42. Being a physician was found to be a protective factor 42. Thus, it is inferred that health education activities that provide increased knowledge of COVID-19 and the establishment of safety measures and support for professionals can improve their sleep quality and well-being.
In general, poor sleep quality is common among nursing and medical personnel who work responding to COVID-19, associated with exposure to patients suspected or confirmed of having the disease, psychological or mental disorders, somatization of diseases, and lack of social support. The need to expand mental health services for staff in hospital institutions, health education, and psychological support is noted 36,37 to improve their sleep quality.
Damage stemming from PPE or other preventive measures
PPE and hand washing are essential measures to prevent infection in healthcare, protecting the staff and users 43. The coronavirus pandemic has demanded more frequent PPE and hand washing, including damage to professionals' health. In this regard, a study with physicians, nurses, and assistants from more than 90 countries, found reports of surgical masks for routine care by 15 % of professionals and, in intubations, by 2 % of them. The results also showed that PPE was used for a median of four hours and that, although they promoted protection to personnel, they triggered adverse effects, particularly associated with longer shifts, such as heat, thirst, pressure spots, headaches, inability to use the bathroom, and exhaustion 7.
Regarding headaches related to PPE use, a study showed that N95 protective masks was associated with this event, with pain related to the PPE pressure points and straps. The pain caused a slight decrease in work performance for 82.8 % of the professionals. A preexisting diagnosis of primary headache and the combined use of PPE for more than four hours a day were independently associated with this type of headache 44.
As to pressure spots, a study has found the prevalence of skin injuries in 42.8 % of physicians and nurses, and of these, 30 % were device-related pressure injuries, 10.7 % were skin damage associated with humidity, and 2 % were skin cracks 45. Another article reported the prevalence of device-related pressure injuries mostly in stages 1 and 2 (98.8 %), located primarily on the nasal bridge, cheeks, ears, and forehead (98.8 %). The risk factors also included sweating, being male, using grade 3 PPE (N95/KN95 masks with goggles or face masks, protective aprons, latex gloves, and shoes), and extended time of use 46,47.
It is highlighted that the discomforts in the work environment can affect the professionals' ability to work, which is understood as the ability to meet the physical and mental demands resulting from their activity 48. In this sense, occupational protection involves measures for promoting well-being and the development of technologies that protect professionals during their activities without causing adverse effects or damage 49.
The skin on the hands of nursing and medical personnel also requires attention, as the recurrent use of gloves can lead to injury. A study found a significant increase in hand washing, disinfection, and hand cream use in all healthcare providers, regardless of whether they had been in direct contact with COVID-19 patients or not during the pandemic 50. There was a prevalence of symptoms associated with acute hand dermatitis in 90.4 % and under-reported eczema in 14.9 %. The most frequent symptoms were dryness (83.2 %), erythema (38.6 %), itching (28.9 %), burning (21.1 %), scaling (18.4 %), cracks (9.6 %), and pain (4.4 %). The authors inferred that the onset of eczema on the hands was probably associated with their intensified hygiene measures 8.
Considering the above, it can be inferred that the use of PPE and other protective measures, such as hand washing, was intensified with the pandemic; however, additional care should be planned to reduce the associated damage to professionals' health.
Conclusions
The scientific evidence enabled the identification of the impact resulting from responding to COVID-19 on the physical well-being of nursing and medical personnel: The prevalence of coronavirus infection related to the environment, the work process, and the prevention measures; the poor sleep quality due to the uncertainties related to the pandemic, mental disorders, and the lack of psychological support; as well as the damage resulting from the frequency of exposure to PPE and hand washing, such as headaches and skin injuries. The results also make clear the need for measures that can prevent damage to physical well-being and promote the health of professionals.
The small number of publications on physical damage stemming from exposure to PPE and other infection prevention measures requires further research. Furthermore, the insufficient evidence on the research topic highlights the need for studies with a different methodological approach.















