Introduction
The prone position is a postural adjuvant therapy first presented in the literature in 1974. It is defined as a maneuver of rotation from a supine to a prone position, effective in managing specific patients1. Used in surgical procedures from ancient times to the present day, prone positioning allows better visualization and access to the particular location of the therapy, as in head, neck, and spine surgeries2. In addition to surgical procedures, it has been observed in recent years that the prone position in patients with Acute Respiratory Distress Syndrome (ARDS) can improve oxygenation and reduce mortality3-4.
Despite the benefits, the prone position is not without risks. It presents the possibility of complications, such as facial edema and pressure lesions in the face region, the thoracic region, and lower and upper limbs. Among these complications, eye injuries are evident, including conjunctival edema and direct pressure on the orbit or eyeball5.
Studies point out that the incidence of pressure injuries due to the prone position is more frequent when compared to patients in the supine position. One study confirmed that the risk of developing pressure injury in the prone position is 57.1 %, while the risk in the supine position is 42.5 °%. In addition, it demonstrated that lesions on the face and chest were the most prevalent6.
The prone position enhances contact between the patient's face and the pillow or cushion. Corneal abrasions from tissue shear may occur if the eyelid is not entirely closed. In this way, the authors report the importance of eye protection so that the complete closure of the eyelid is possible, minimizing the risks of eye complications until the potential loss of vision7.
Among complications, a large part is related to the management by the nursing team, given that nursing is closer to patient care. Therefore, it is up to the nurse professionals to develop care plans to minimize the incidence of complications. It is known that care for critical and surgical patients is complex due to the required procedures. Therefore, some care is overlooked by the teams, such as eye care. However, vision preservation must be prioritized, considering the eyes are critical sensory organs8-9.
Some interventions are used for eye care in critically ill/surgical patients in the prone position, such as hydrocolloid patches, ointments, and lubricating eye drops. However, no studies were found in the literature that addressed the degree of recommendation of interventions for eye protection. Despite the scale of the problem, eye care protocols are generally not encouraged, and documentation of this care is often deficient10.
In this context, the study is justified by the need to obtain scientific knowledge about possible eye care/interventions to be implemented in the care of patients in a prone position. There is a clear need for specific care protocols to manage complications and reduce patient risks. New studies on this topic add even more quality to health care since protocols for eye care are scarce10.
This study aimed to map evidence of interventions applied to eye care in managing critical or surgical patients submitted to the prone position.
Material and methods
Design
It is a scoping review, prepared according to the methodological assumptions of the Joanna Briggs Institute of 2020, following criteria defined by the checklist Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR)11-12. The study in question was registered on the Open Science Framework study platform and generated a sequential identifier from Uniform Resource Locator13.
Through the guidance of a research protocol, the five methodological steps were followed: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) mapping and extracting the results; and (5) making a narrative synthesis of the results11.
Identifying the research question
As a way of defining the guiding question of the review, the PCC mnemonic strategy was used, where P: population (critical or surgical patients); C: concept (strategies and interventions for eye care), and C: context (critical or surgical patients who need the prone position during care). Based on this strategy, the following research question was delimited: What strategies and interventions are used for eye care in managing critical or surgical patients submitted to the prone position?
Identifying relevant studies
To identify relevant studies for the presented theme, a search was carried out from July to August 2020 on the following databases: SCOPUS, Web of Science, Science Direct, PubMed Central, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and COCHRANE. Access for the search was supported by the Federal University of Rio Grande do Norte, via the Federated Academic Community, through the Coordination for the Improvement of University Education Personnel.
As a search strategy in the databases, the descriptors ordered in Medical Subject Headings (MeSH) were defined: "Eye," "Eye Health," "Nursing Care," "Critical Care," "Ocular Care," "Intensive Care Units," and "Prone Position." To identify other relevant studies, a search was performed on Google® scholar using the keywords identified in the studies in the first phase of the search. Crossings used the Boolean operator AND, as shown in Table 1.
Table 1 Search strategies used in each database. Natal-RN, Brazil, 2020
| DATABASE | CROSSING |
| SCOPUS | ALL("Eye Health"' AND '"Prone Position"' ALL("Eye Health"' AND '"Prone Position"' AND '"Nursing Care"' ALL("Eye"' AND '"Prone Position"' AND '"Nursing Care"' ALL("Eye Health"' AND '"Prone Position"' AND '"Critical Care"' ALL("Eye"' AND '"Prone Position"' AND '"Critical Care"' ALL("Eye Health"' AND '"Prone Position"' AND '"Intensive Care Units"' ALL("Eye"' AND '"Prone Position"' AND '"Intensive Care Units"' ALL("Eye"' AND '"Prone Position"' |
| WEB OF SCIENCE | ALL='"Eye Health"' AND '"Prone Position"' ALL='"Eye Health"' AND '"Prone Position"' AND '"Nursing Care"' ALL='"Eye"' AND '"Prone Position"' AND '"Nursing Care"' ALL='"Eye Health"' AND '"Prone Position"' AND '"Critical Care"' ALL='"Eye"' AND '"Prone Position"' AND '"Critical Care"' ALL='"Eye Health"' AND '"Prone Position"' AND '"Intensive Care Units"' ALL='"Eye"' AND '"Prone Position"' AND '"Intensive Care Units"' ALL='"Eye"' AND '"Prone Position"' |
| SCIENCE DIRECT | TITLE, ABSTRACT, KEYWORDS: "Eye Health" AND "Prone Position" "Eye Health" AND "Prone Position" AND "Nursing Care" "Eye" AND "Prone Position" AND "Nursing Care" "Eye Health" AND "Prone Position" AND "Critical Care" "Eye" AND "Prone Position" AND "Critical Care" "Eye Health" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" |
| PUBMED CENTRAL | ALL FIELDS: "Eye Health" AND "Prone Position" "Eye Health" AND "Prone Position" AND "Nursing Care" "Eye" AND "Prone Position" AND "Nursing Care" "Eye Health" AND "Prone Position" AND "Critical Care" "Eye" AND "Prone Position" AND "Critical Care" "Eye Health" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" |
| CINAHL | "Eye Health" AND "Prone Position" "Eye Health" AND "Prone Position" AND "Nursing Care" "Eye" AND "Prone Position" AND "Nursing Care" "Eye Health" AND "Prone Position" AND "Critical Care" "Eye" AND "Prone Position" AND "Critical Care" "Eye Health" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" |
| COCHRANE | TITLE, ABSTRACT, KEYWORDS: "Eye Health" AND "Prone Position" "Eye Health" AND "Prone Position" AND "Nursing Care" "Eye" AND "Prone Position" AND "Nursing Care" "Eye Health" AND "Prone Position" AND "Critical Care" "Eye" AND "Prone Position" AND "Critical Care" "Eye Health" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" AND "Intensive Care Units" "Eye" AND "Prone Position" |
| GOOGLE® SCHOLAR | "Eye Health" AND "Nursing Care" AND "Prone Position" "Eye Health" AND "Critical Care" AND "Prone Position" "Eye Health" AND "Intensive Care Units" AND "Prone Position" "Ocular Care" AND "Prone Position" "Ocular Care" AND "Intensive Care Units" AND "Prone Position" |
Source: Own elaboration.
A reverse search was performed using references identified in the selected articles to identify additional studies. This way, it is possible to capture articles relevant to the study that were not viewed in the databases. The reverse search allows for a broader sample, making it possible to understand more comprehensively the study process of a given research subject matter11.
The inclusion criteria used were studies that addressed evidence about eye care interventions in patients in a prone position, full-text articles in the databases, original articles, and review articles e articles available in English, Portuguese, and Spanish. Regarding the year of publication, the studies were selected between 1999 and 2020. Editorials, letters to the editor, abstracts, and articles that did not address the relevant topic within the scope of the review objective were excluded from the sample.
Identifying relevant studies
The search process was carried out in pairs on different computers at the same time. At the end of each part of the search, the results were analyzed by dynamically reading the titles and abstracts, and subsequently, they were read in full by two reviewers independently. Studies that did not meet the eligibility criteria were excluded, duplicates were counted only once, and divergences between reviewers were decided by consensus.
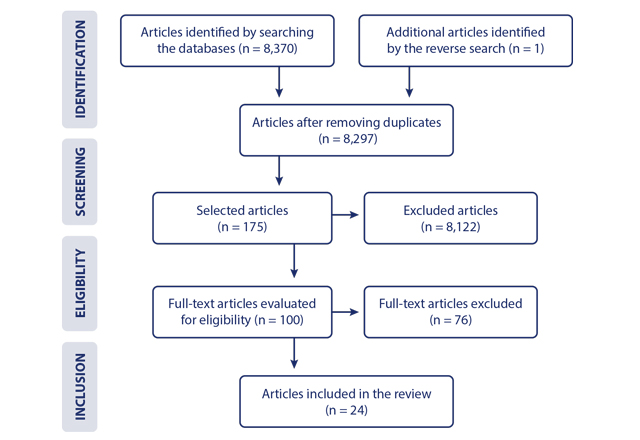
The search stage in databases and Google® scholar resulted in a total of 8,371 identified articles. After applying the inclusion and exclusion criteria, 23 were selected. In a similar search in references, one article was included. Thus, 24 studies made up the final sample, according to the flowchart shown in Figure 1.
Mapping the data
Data mapping and extraction were performed using an instrument prepared with the following items: title of the study, authors, year of publication, country, type of study, evidence level and degree of recommendation, source data, objective of the study, central interventions, and conclusions on eye care in the prone position.
Regarding the evidence level and the degree of recommendation, we decided to follow the Oxford Center for Evidence-Based Medicine guidelines. Thus, the classification of the evidence level followed the pattern that the lower the number, the higher the level. In addition, the degree of recommendation considers "A" as the highest recommendation and "D" as the lowest recommendation14.
Results
As for the characterization of the studies selected and analyzed in the review, the data were presented according to year, data source, and place of publication (Table 2).
Table 2 Characterization of studies according to year, data source, and country of publication (n = 24). Natal-RN, Brazil, 2020.
| Variables | N | % |
|---|---|---|
| Year of publication | ||
| 2016 ‖- ‖ 2020 | 10 | 41.6 |
| 2011 ‖- ‖ 2015 | 09 | 37.5 |
| 2004 | 02 | 8.3 |
| 2009 | 01 | 4.1 |
| 2006 | 01 | 4.1 |
| 1999 | 01 | 4.1 |
| Data source | ||
| SCOPUS | 13 | 54.1 |
| Science Direct | 05 | 20.8 |
| CINAHL | 02 | 8.3 |
| Web of Science | 01 | 4.1 |
| PubMed Central | 01 | 4.1 |
| Google® Scholar | 01 | 4.1 |
| Parallel search | 01 | 4.1 |
| Country of publication | ||
| USA | 13 | 54.1 |
| United Kingdom | 04 | 16.6 |
| Turkey | 02 | 8.3 |
| Australia | 02 | 8.3 |
| Spain | 01 | 4.1 |
| France | 01 | 4.1 |
| Singapore | 01 | 4.1 |
Source: Own elaboration.
Studies that addressed the surgical patient were more frequent with 66.7 % (n = 16), followed by studies with critical patients 25.0 % (n = 6). Only 8.3 °% (n = 2) addressed the two populations in the same study.
After a complete analysis of the 24 studies selected for the scoping review, we could identify the title, authors, year, country of publication, type of study, evidence level, degree of recommendation, and interventions on eye care in critical or surgical patients in the prone position of the selected studies, as shown in Table 3.
Table 3 Identification of studies and eye care interventions in patients in the prone position. Natal-RN, Brazil, 2020
| Title | Authors (year) | Country of publication | Type of study/ Evidence level /Degree of recommendation* | Eye care interventions in patients in the prone position |
|---|---|---|---|---|
| The prone position during surgery and its complications: A systematic review and evidence-based guidelines | Kwee et al. (2015)15 | Australia | Systematic review/1A/A | Reverse Trendelenburg; use of head restraints; Mayfield headrest; monitoring eye position every 20 minutes with a mirror attached to the headrest; computer video streaming system to monitor the eye position throughout the process; preoperative ophthalmological examination |
| Systematic review and meta-analysis of prone position on intraocular pressure in adults undergoing surgery | Wilcklin (2020)16 | USA | A systematic review and meta-analysis/1A/A | Preoperative eye exams; reverse Trendelenburg from 5 to 10°; monitoring intraocular pressure; providing periodic changes in position or rest periods, and administering specific medications or anesthetics can help reduce the risk of eye damage |
| The comparison of four different methods of perioperative eye protection under general anesthesia in prone position | Kocatürk et al. (2012)17 | Turkey | Randomized clinical trial/1B/A | The following eye protection methods were applied: Hypafix® hypoallergenic adhesive tape, Terramycine® antibiotic ointment, artificial tear gel containing Viscotears® polyacrylic acid, and Duratears ointment eye lubricant. There was no significant difference between groups regarding adhesive tapes. All methods are suitable for protecting against corneal injuries |
| The effect of head rotation on intraocular pressure in prone position: a randomized trial | Deniz et al. (2012) 18 | Turkey | Randomized clinical trial/1B/A | Patients in a prone position with the head turned 45° sideways to the right side had significantly lower intraocular pressure than those in a prone position without head rotation |
| Clinical trial design effect of prone positioning on clinical outcomes in infants and children with acute respiratory distress syndrome | Curley et al. (2006) 19 | USA | Randomized clinical trial/1B/A | If the patient is receiving a paralytic pharmacological agent or if there is incomplete eyelid closure, eye protection is provided to prevent corneal abrasions |
| The effect of body inclination during prone positioning on intraocular pressure in awake volunteers: A comparison of two operating tables | Ozcan et al. (2004) 20 | USA | Clinical trial/1B/A | The reverse Trendelenburg position of 10° improves intraocular pressure in patients in the prone position |
| Comparison of medical adhesive tapes in patients at risk of facial skin trauma under anesthesia | Zeng et al. (2016) 21 | Singapore | Randomized controlled clinical trial/1B/A | The use of silicone tapes 'removal type 3M™' for eyelids significantly reduces skin lesions compared to standard acrylate tapes |
| Effect of the degree of reverse Trendelenburg position on intraocular pressure during prone spine surgery: A randomized controlled trial | Carey et al. (2014)22 | USA | Randomized controlled clinical trial/1B/A | Reverse Trendelenburg positioning decreases intraocular pressure in patients in a prone position for spinal surgery |
| Effects of crystalloid versus colloid and the a-2 agonist brimonidine versus placebo on intraocular pressure during prone spine surgery | Farag et al. (2012) 23 | USA | Randomized clinical trial/1B/A | Using 2 % brimonidine administered preoperatively helps reduce intraocular pressure during spine surgeries in the prone position |
| Pressure on the Face While in the Prone Position: ProneView™ versus Prone Positioner™ | Atwater et al. (2004)24 | USA | Clinical trial/1B/A | ProneViewTM produces a lower face surface pressure than the Prone PositionerTM device, reducing the incidence of skin damage |
| Modified prone position using lateral brace attachments for cervico-dorsal spine surgeries | Kadam et al. (2013) 25 | USA | Clinical trial/1B/A | Cervical tweezers with two cylindrical padded supports and two lateral supports were applied to a conventional operating table to stabilize the head and reduce eye and facial complications related to the pressure of the prone position |
| Care of the eye during anaesthesia and intensive care | Small et al. (2019) 8 | United Kingdom | Descriptive study/2C/B | In critically ill patients, the eyes should be examined, relubricated, and closed with tape every four hours. The position must remain neutral or with the head higher than the heart. In surgical patients, head support (Mayfield) is recommended |
| Eye protection in anaesthesia and intensive care | Keita et al. (2017) 26 | France | Literature review/2C/B | It is recommended that lubricants containing an aqueous solution in a single dose be used, such as methylcellulose or viscosogel, combined with occlusion of the eyelid using adhesive tapes. In addition, the use of appropriate head restraints (Mayfield or specific cushion) and a slight inclination, such as the Trendelenburg position, are advisable |
| Prone position of patients with COVID-19 and acute respiratory distress syndrome | Makic (2020)27 | USA | Literature review/2C/B | The patient's eyes should be lubricated and closed to protect against corneal injury |
| Artificial ventilation in the prone position | Gibson et al. (1999) 28 | Australia | Literature review/2C/B | Training on implications and complications of making the patient prone. Regular eye care and protection from the pillow surface may be necessary to prevent abrasion of the cornea |
| Helmet continuous positive airway pressure and prone positioning: A proposal for an early management of COVID-19 patients | Longhini et al. (2020)29 | Spain | Literature review/2C/B | Continuous positive airway pressure during the prone position is more comfortable since it allows for constant and extended treatment and fewer complications related to the interface (that is, irritation in the eyes, gastric distension, and skin necrosis) |
| Eye care in the intensive care unit during the COVID-19 pandemic | Sansome et al. (2020)30 | United Kingdom | Literature review/2C/B | Daily eye examination; lubricating ointment every 4 hours; referral to ophthalmology when necessary; if there are concerns about damage to the cornea, further examination can be performed; before applying the lubricating ointment, the eye should be bathed in gauze soaked in saline and cleaned inside out |
| Ocular care and complications in the critically ill | Kam et al. (2011)31 | United Kingdom | Literature review/2C/B | Adhesive tapes are recommended, as lagophthalmia is frequently checked or viscous lubricating drops are instilled often. Patients should be referred to ophthalmologists if there is constant exposure |
| Current intraoperative devices to reduce visual loss after spine surgery | Urine et al. (2012) 32 | USA | Literature review/2C/B | The review showed the classic horseshoe-shaped headrest, the face mask with foam pad and transparent operating table, the OPTI-GARD eye protector, the VOSS Prone positioner, the ROHO neoprene cushion, the "float a dry," the Proneview® helmet system, and the Proneview® video camera monitoring system as new devices to prevent mechanical eye compression during surgical procedures in the prone position |
| Positioning patients for spine surgery: Avoiding uncommon position- related complications | Kamel et al. (2014) 33 | USA | Literature review/2C/B | Evidence shows that the head must be in a neutral position on the head support structure to avoid direct pressure on the eye (Proneview®'. Proneview® allows for prone positioning without any pressure on facial structures. The extendable mirror allows frequent checking of facial structures in the prone position |
| How to avoid perioperative visual loss following prone spinal surgery | Epstein (2016)34 | USA | Literature review/2C/B | Preventive measures such as routine use of an arterial line, intraoperative monitoring, 3-pin head support, and elevation of the head 10° from the horizontal decrease the risk of perioperative visual loss in spine surgeries performed in the prone position |
| Perioperative visual loss: What do we know, what can we do? | Roth (2009)35 | USA | Literature review/2C/B | Using foam headrests and a mirror to allow a direct view of patients' eyes during spinal surgery in a prone position prevents the loss of perioperative vision |
| Extendable mirrors to improve anesthesia provider comfort for eye and positioning checks in prone patients: A pilot study | Lin et al. (2020)36 | USA | Pilot study/2C/B | The use of an extensible mirror is recommended for frequent eye checking and careful neck positioning |
| Strategies to prevent ischemic optic neuropathy following major spine surgery: A narrative review | Fandino (2017)37 | United Kingdom | Narrative review/3A/B | The review presented interventions such as keeping the head at the same level or higher than the heart and maintaining approximately 10° in the direction of reverse Trendelenburg for spinal procedures in a prone position to improve the increase in intraocular pressure |
*Evidence level: 1A, 1B, 1C (degree of recommendation A); 2A, 2B, 2C, 3A, 3B (degree of recommendation B); 4 (degree of recommendation C); and 5 (degree of recommendation D)13
Source: Own elaboration.
Table 4 features the primary eye care interventions according to the population (critical and surgical patients).
Table 4 Characterization of the primary interventions for eye care in patients in a prone position (n = 24). Natal-RN, Brazil, 2020
| Main interventions | N | %* |
|---|---|---|
| Eye examination | ||
| Critical patients | 03 | 12.5 |
| Surgical patients | 07 | 29.1 |
| Use of lubricants/specific ophthalmic solution | ||
| Critical patients | 06 | 25.0 |
| Surgical patients | 03 | 12.5 |
| Reverse Trendelenburg positioning | ||
| Critical patients | 01 | 4.1 |
| Surgical patients | 07 | 29.1 |
| Protection with adhesive tape | ||
| Critical patients | 05 | 20.8 |
| Surgical patients | 03 | 12.5 |
| Adequate head support | ||
| Critical patients | - | - |
| Surgical patients | 06 | 25.0 |
| Cleaning with saline solution | ||
| Critical patients | 02 | 8.3 |
| Surgical patients | - | - |
| Head rotation at 45° | ||
| Critical patients | - | - |
| Surgical patients | 01 | 4.1 |
| Professional training | ||
| Critical patients | 01 | 4.1 |
| Surgical patients | - | - |
*The variable assumes multiple responses.
Source: Own elaboration.
Regarding the central interventions for eye care in patients in the prone position, eye examination, the use of lubricants/specific ophthalmic solution, the reverse Trendelenburg positioning, and the protection with adhesive tape stand out.
Discussion
Noteworthy are the scientific productions published in the last year, demonstrating the relevance of the theme today. Next, the evidence identified will be addressed in two categories: eye care in critically ill patients and eye care in surgical patients. The study was limited by the low number of more specific recommendations, especially concerning ophthalmic care in critically ill patients. As corroborated by the study, there is a need for further studies in intensive care units to assess eye injury, including the follow-up of patients38.
Eye care in critically ill patients in the prone position
Related to critical patients, it is known that the intervention of the prone position is an essential therapy for hypoxemic respiratory failure and ARDS, including for patients with COVID-19 in the current context27.
Concerning patients undergoing treatment for COVID-19, they are more susceptible to eye complications due to prone positioning and the increased demand by the intensive care team39-41. Critically ill patients can be in the prone position for at least 16 hours a day to improve oxygenation. One study observed patients in the prone position for long periods who had bilateral funduscopic findings of optic disc edema and retinal hemorrhages, in addition to a substantial increase in intraocular pressure42.
However, prone position intervention in critically ill patients with breathing difficulties has often been discussed only in recent years. As a result, few published studies are related to critically ill patients. The study points out that despite our routine ophthalmic protocols, invasive mechanical ventilation applications predispose to corneal surface damage in patients in the intensive care unit43-44. Thus, knowledge of complementary protocols for eye care in critically ill patients is necessary.
Regarding eye care in patients with COVID-19, the authors did not present any intervention other than those recommended in uncontaminated patients. Because it is a recently discovered virus, further studies are needed to define care with lower infection risks25,27,30. Among the interventions, lubricants and eye protection with adhesive tape were the most frequent in the sample for critically ill patients, followed by eye examination and cleaning with saline.
In general, in patients receiving an anesthetic pharmacological agent or with incomplete eyelid closure, the authors recommend that, before performing the prone positioning maneuver, the eyes should be cleaned with saline, preferably inside out in a single direction, applied lubricant drops, and protected with adhesive tapes19,27. After performing the maneuver, it is recommended that the eyes be examined, relubricated, and closed with tape every four hours8.
Regarding the eye examination, it is recommended that it be done daily. If there is a concern related to the damage, a deeper examination of the eyes can be performed with the application of drops of fluorescein and viewing the cornea through blue light, often found in ophthalmoscopes. Patients who are constantly exposed should be referred to ophthalmologists27,34.
The study identified patients in the prone position who required treatment for eye diseases through detailed examinations, first with a handheld biomicroscope and direct ophthalmoscope for each patient. Then, the eyes were dilated with 1 % tropicamide, and retinal and optic nerve examinations were performed with an ophthalmoscope45.
As for positioning during the prone position, patients should be kept in a neutral position or with the head higher than the heart level (reverse Trendelenburg)8. Studies with critically ill patients did not address the degree of elevation for the reverse Trendelenburg.
Concerning the devices used, a recent study showed that the prone position becomes more comfortable when using Continuous Positive Airway Pressure (CPAP), as this approach develops fewer complications, such as eye irritation30.
It is also observed that the teams' training on the possible complications of the prone position is indispensable to managing patients adequately and preventing risks35,46. The training of care professionals in handling patients in the prone position is less frequent; however, it is an intervention that must be considered.
A clinical trial performed on patients with reduced or absent blink reflex after losing consciousness or using sedatives determined that implementing the eye care protocol could significantly reduce complications and eye problems47. Based on these data, developing protocols for eye care is essential.
Eye care in surgical patients in the prone position
Studies involving surgical patients in the prone position appear more frequently in the sample. Due to the long surgery period, it is necessary to intervene so that new complications do not occur, prioritizing patient safety. In patients undergoing spinal surgery, for example, the prone position has a tenfold increased risk of eye injury compared to the supine and lateral positions48.
Reverse Trendelenburg positioning, eye examination, and adequate head support were the most addressed interventions among the studies. The reverse Trendelenburg is used as a strat egy to reduce intraocular pressure and, consequently, perioperative visual loss21,24. The authors recommend that the head elevation should be 10°16,33.
As for eye examination, a preoperative ophthalmological examination is recommended to form an opinion about the 'patient's vision. As intraoperative interventions, some authors have addressed using an extensible mirror for frequent eye checking32,34. One study showed eye position monitoring every 20 minutes with an attached mirror as a strategy. A computer video streaming system was implemented to monitor the eye position throughout the process, proving to be a practical technological innovation in health15.
Concerning adequate head support, an effective strategy to reduce the risk of direct pressure on the eye involves using a three-pin Mayfield head support, which fixes and holds the head during surgical procedures8,24. Another device used to reduce direct pressure is the ProneViewTM protective helmet system with facial contour, which allows for prone positioning and reduces the incidence of facial damage. Compared to the Prone PositionerTM without facial contour, this system proved more effective25,27-28,49.
The use of tapes for eye protection and lubricants was less frequent in the sample. Regarding the protection with adhesive tape, a study concluded that the use of silicone tapes with the removal of the type 3M for eyelids used in long surgeries significantly reduced skin lesions when compared with acrylate tapes, thus presenting itself as a strategy that can be considered for eye protection24,27-28,50.
In contrast, a study compared the effectiveness of four protection methods, involving the use of Hypafix® hypoallergenic adhesive tape, Terramycine® antibiotic ointment, artificial tear gel containing Viscotears® polyacrylic acid, and Duratears® ointment eye lubricant. It was concluded that there was no significant difference between the protection methods, showing that all the methods presented are suitable for protecting against corneal injuries17,23,51.
Corroborating the findings of the review, a prospective study performed a trial with a foam-based facial protection method to cover bony prominences during spinal surgical procedures, decreasing the incidence of iatrogenic facial ulcers in surgery by reducing friction and shear force52.
Some studies have addressed using a specific ophthalmic solution to lower intraocular pressure in surgical patients. In one of these studies, the authors recommended using 2 % brimonidine, which should be used preoperatively, for about one hour before anesthesia and every eight hours for 24 hours, helping reduce intraocular pressure in spine surgeries25,53-54. Only one study pointed to head rotation at 45° turned to the right as a technique for lowering intraocular pressure in patients placed in a prone position18.
Conclusion
Among the findings of the selected studies, care was suggested using lubricants to prevent dry eyes and specific ophthalmic solutions to reduce intraocular pressure. It is also essential to associate the prone position with the reverse Trendelenburg to minimize the risk of pressure in the face region and the proper headrest. The studies also propose recommendations on eye protection with adhesive tapes, frequent eye examination, cleaning with saline solution, and head rotation at 45° as essential precautions for preventing risks associated with eye health.
More collaborative clinical studies on eye care are suggested in isolation, as a shortage of scientific evidence that addressed more specific recommendations was identified, especially in critically ill patients.