Introduction
Population aging is now a phenomenon in developed and developing countries 1. The proportion of people in their 60s and older worldwide is growing faster than the other age groups. It is estimated that by 2050 there will be two billion older people, of which 80 % will live in developing countries 2. Despite these estimates, the Pan American Health Organization 3 published the World Report on Aging in 2022, expressing concern over widespread age-related healthcare rationing and indicating that health research tends to exclude older adults, even though several health conditions are more prevalent in elderly individuals.
The population's longevity, associated with social and family changes, such as the increasing insertion of women in the workplace and the reduction in the size of families, raise concerns regarding the care provided to the elderly who depend on third parties 4. It stands out that the increase in life expectancy and the high morbidity rate due to chronic-degenerative diseases are some of the most significant challenges for public health today 5-7.
Although the disease affects the individual, its consequences also affect the family and the people who live and work with the patient, in a process that challenges and modifies family roles and group dynamics 8. In addition, the older adult's aging process leads to feelings that involve the perspective of life terminality, both for their families and the professional team 9-11. Thus, with an aging population that will live and die under more complex conditions, the demand for care tends to increase, along with the demand for palliative care 12-14.
Palliative care (PC) was defined in the 1990s and restated in 2002 by the World Health Organization (WHO) as a multidisciplinary approach that aims to improve the quality of life of patients and their families in the presence of a life-threatening illness through the prevention and relief of suffering, accurate and careful assessment, treatment of pain, and other demands (physical, psychosocial, or spiritual) 5,8. More recently, this concept has been redefined, and PC now includes chronic conditions that are progressive from diagnosis, along with therapies that can modify or potentially cure the disease 15,16.
PC must be regarded as a fundamental right of individuals and an essential component of comprehensive and integrated care throughout life, including at the end of life 10. Although a relatively new component of modern healthcare, it is becoming increasingly recognized as an essential part of all health systems 12. It should be available in any healthcare setting, such as hospitals, long-term care facilities, health centers, and even in patients' homes 16,17.
In 2018, recognizing the need to improve and implement evidence-based PC policies and to support the comprehensive improvement of health systems at all levels, the Ministério da Saúde (Ministry of Health) of Brazil published Resolution 41, which provides guidelines for the organization of PC in light of integrated continuous care within the scope of Brazil's Sistema Único de Saúde (Unified Health System) 18.
However, the implementation of comprehensive care in the Rede de Atenção à Saúde - RAS (Healthcare Network System - HNS) implies strategies that anticipate the transition of this type of care across various levels within this System. The transition of care is a strategy that involves a group of planned measures to ensure the continuity and safe coordination of the care provided, which can increase the quality of life of patients and their families 19,20.
Therefore, conducting studies that allow a broader view of PC in the HNS is considered relevant, so patients and their families can receive comprehensive care. Given the above, this study aims to map the scientific evidence related to the organization of PC practices for older adults in the HNS.
Materials and methods
This scoping review is based on the international guidelines of the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR [21]), whose protocol was registered in the Open Science Framework (https://osf.io/83p7u/). The review was conducted according to the Joanna Briggs Institute 22 methodological guidelines, with the following steps: 1) identification of the research question; 2) identification of relevant studies; 3) study selection; 4) data analysis; 5) data grouping, synthesis, and presentation.
The review question and the inclusion and exclusion criteria were discussed and agreed upon by the researchers. The guiding question was defined using the PCC strategy, where P (population) is older adults, C (concept) is PC, and C (context) is the HNS. The question was: "How are PC practices organized for the elderly in the HNS?"
The sample was composed of studies that met the following inclusion criteria: Articles published in national and international journals from January 2010 to March 2021 in Portuguese, English, and Spanish. Articles that were not available in full-text were excluded, as well as gray literature, such as monographs, dissertations, theses, books, blogs, editorials, and guidelines. It is noteworthy that the gray literature was excluded to eliminate possible biases related to the inclusion of evidence with value judgment or opinions that failed to represent the subject matter; furthermore, due to the possibility of excessive volume of material, it would require the expansion of the inclusion criteria, possibly affecting the sample of scientific articles found. Studies that described and discussed the organization of PC practices for the elderly from the perspective of the HNS were considered eligible.
The search strategy was carried out by a librarian at the Biblioteca Baeta Vianna (Baeta Vianna Library) of the Universidade Federal de Minas Gerais (Federal University of Minas Gerais), Brazil. The articles found were managed using the Endnote software, which allowed peer review to be carried out independently. The search was conducted in April 2021 in the following databases: Medline®/ National Library of Medicine (PubMed), Scopus, Cumulative Index to Nursing and Allied Health Literature (Cinahl), Web of Science (WoS), Embase, Cochrane, and Biblioteca Virtual de Saúde (BVS). The Health Sciences Descriptors (DecS) and Medical Subject Headings (MeSH) related to the elements of the research question were used, as shown in Table 1.
Table 1 Definition of database search strategies, Belo Horizonte, 2022
| Database | Search strategy |
|---|---|
| BVS* | (idoso OR idosos OR "pessoa idosa" OR "pessoa de idade" OR "pessoas idosas" OR "pessoas de idade" OR "população idosa" OR "idoso fragilizado") AND ("cuidados paliativos" OR "assistência paliativa" OR "cuidado paliativo" OR "cuidado paliativo de apoio" OR "tratamento paliativo" OR "cuidados paliativos na terminalidade da vida" OR "cuidado paliativo a doentes terminais" OR "cuidados a doentes terminais" OR "cuidados de conforto" OR "programas de cuidados intermitentes" OR "programas de cuidados paliativos" OR "estado terminal" OR "doença terminal" OR "estado crítico") AND ("assistência integral à saúde" OR "atenção primária à saúde" OR "atenção secundária à saúde" OR "atenção terciária à saúde" OR "colaboração intersetorial" OR "serviços de saúde para idosos") |
| Medline/PubMed Cochrane Cinahl Scopus WoS | (aged OR "frail elderly") AND ("palliative care" OR "hospice care" OR "critical illness") AND ("comprehensive health care" OR "primary health care" OR "secondary care" OR "tertiary healthcare" OR "intersectoral collaboration" OR "health services for the aged") |
| Embase | (aged OR "frail elderly") AND ("palliative therapy") AND ("primary health care" OR "secondary health care" OR "tertiary care center" OR "intersectoral collaboration" OR "elderly care") |
Source: Elaborated by the authors.
The first step involved searching the databases and extracting the identified articles into the EndNote® software. The articles then had their titles and abstracts read and analyzed by six reviewers, who worked in pairs in a double-blind format to select the potential eligible articles. In cases of doubts regarding inclusion, the researchers performed the inclusion analysis jointly.
The articles that composed the final sample were read in full by all reviewers independently, aiming to answer the review question and extract the data of interest. It should be noted that the reference lists of the article sample included in the review were examined for additional sources. However, no articles were added. Subsequently, the data were organized in a spreadsheet created in Microsoft Excel 2016, whose structure contemplated essential elements of the studies: Publication year, country of origin, objectives, study type, population, study site, and main results. The data synthesis is descriptively presented in this article and discussed with the relevant literature.
Results
A total of 1,150 articles were identified in the database search, and the final sample consisted of 12 articles, as shown in Figure 1.
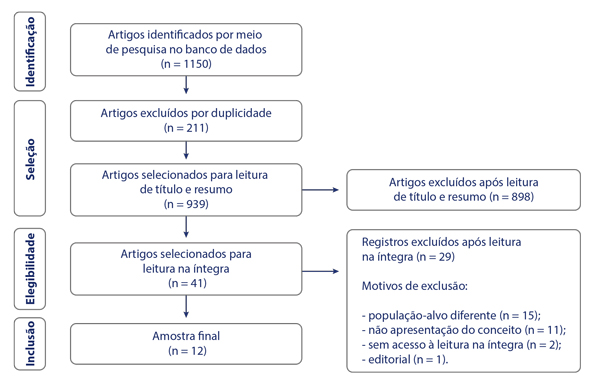
Source: Elaborated by the authors.
Figure 1 Study selection flowchart, adapted from PRISMA-ScR, Belo Horizonte, Minas Gerais, Brazil, 2022
The 12 articles included in this review were organized into a bibliographic framework presented in Table 2, containing the article title, country of origin, publication year, type of study, and result synthesis.
Table 2 Articles included in the scoping review, Belo Horizonte, Minas Gerais, Brazil, 2022
| Author(s) | Title | Location, year | Type of study | Article result synthesis |
|---|---|---|---|---|
| AlbersG, Froggatt K, Van den Block L, Gambassi G, Vanden Berghe P, Pautex S, et al.23 | A qualitative exploration of the collaborative working between palliative care and geriatric medicine: Barriers and facilitators from a European perspective | Europe, 2016 | Qualitative study | • States that the care system for the elderly in PC should be based on the premise of interdisciplinary coordination • Points to the fragmentation of care for the elderly in PC and the frailty of communication between disciplines • Stresses the relevance of interdisciplinary teamwork as an opportunity for mutual and collaborative learning |
| Ankuda CK,Petterson SM, Wingrove P, Bazemore AW 24 | Regional variation in primary care involvement at the end of life | The United States of America, 2017 | Cross-sectional study | • Discusses how the participation of primary care medical professionals in PC for the elderly reduces health system costs, the length of stay in hospital institutions, and invasive procedures • Indicates that care at the primary level reduces the fragmentation of care for the elderly in end-of-life care |
| Brasil K, Galway K, Carter G, Van der Steen JT 25 | Providing optimal palliative care for persons living with dementia: A comparison of physician perceptions in the Netherlands and the United Kingdom | The Netherlands and The United Kingdom, 2017 | Cross-sectional study | • States that the main obstacles faced by the healthcare system in managing older adults with dementia in PC are professionals' limited education and limited access to specialized care • Suggests that care for older people with dementia in PC should be person-centered, with family involvement and staff training on effective communication |
| Ahia C, Blais CM 26 | Primary palliative care for the general internist: Integrating goals of care discussions into the outpatient setting | The United States of America, 2014 | Case study | • Discusses that accompanying the elderly in PC at the primary level contributes to their trajectory in the healthcare system and effective communication and assists in decision making • Reports that general practitioners and family physicians at the primary level are crucial to discussing the treatment objective and achieving better outcomes |
| Lanza CC, O'Shea CJC, Herrera JL, Pena CG 27 | Cuidados paliativos: la opción para el adulto en edad avanzada | Mexico, 2015 | Review study | • States the need for PC for the elderly to be coordinated and integrated into the health system • Cites primary care as the organizer of care and highlights its proximity to the patient's home in PC • Highlights that, in the primary care context, it is necessary to guide caregivers and family members in collaborative interdisciplinary care with the health team |
| Toye C, Blackwell S, Maher S, Currow DC, Holloway K, Tieman J, et al.28 | Guidelines for a palliative approach for aged care in the community setting: A suite of resources | Australia, 2012 | Systematic review | • Highlights primary care in the center of care in the health system and the importance of considering the home for PC practice • Stresses that the home is a preferred PC locus for the elderly, as it integrates family and relational elements that already exist and reduces expenses and avoidable procedures • Contextualizes that many older people spend their end of life in hospital institutions against their wishes and notes that there are unnecessary transfers |
| Tuckett A, Parker D, Clifton K, Walker H, Reymond E, Prior T, et al.29 | What General Practitioners said about the palliative care case conference in residential aged care: An Australian perspective. Part 2 | Australia, 2015 | Qualitative study | • States the importance of the multi-professional primary care team in the care provided to the elderly in PC • Highlights the role of nurses as powerful agents for reducing the frailty of PC supply • Emphasizes the home as the preferred locus of PC for the elderly, emphasizing the need for a formalized care plan, effective communication, teamwork with the family, and prioritization of the bond with the team instead of a professional |
| Van der Steen JT, Dekker NL, Gijsberts MJHE, Vermeulen LH, Mahler MM, The BAM 30 | Palliative care for people with dementia in the terminal phase: A mixed-methods qualitative study to inform service development | Australia, 2017 | Qualitative study | • Discusses the relevance of primary care as settings for PC practices for the elderly • Highlights the importance of providing PC to the elderly at home, especially in the terminal phase • States that the elderly spend the end of life in hospital institutions against their will and justifies that this is due to the health system's frailty, as it fails to focus on chronic diseases, the long wait for consultations, and the lack of dedicated PC professionals • Suggests specialized mobile teams that accompany the elderly in PC and their families instead of unnecessary transfers to hospitals |
| Ayyar A, Varman S, De Bhaldraithe S, Singh I 31 | The journey of care for the frail older person | The United Kingdom, 2010 | Review study | • Recognizes that the healthcare of the elderly in PC needs to be provided in an expanded format in the different devices of the health system • Stresses the importance of the interface between primary and secondary care of the elderly based on information exchange and reliable and quality care. • Suggests an integrated care model for the frail elderly, composed of a multi-professional team in the different healthcare devices, which should be prepared to promote bonding and perform safe transfers |
| Jadhav AV 32 | Rural elderly and access to palliative care: A public health perspective | India, 2020 | Review study | • Identifies frailty in the organization of PC in the public health system • Highlights that PC for the elderly is neglected in the health system context, especially regarding the patients' access and the investment allocated to oncologic hospitals • States the importance of primary care as the organizer of care |
| Deborah R, Waterworth S, Merryn G 33 | The role of practice nurses in providing palliative and end-of-life care to older patients with long-term conditions | Australia, 2014 | Qualitative study | • Highlights the role of primary care nurses in PC and end-of-life in the elderly • States the professionals' need to develop PC skills and knowledge • Criticizes the nurses' limited autonomy in PC participation, conditioned to the referring physician • Recognizes the importance of nurses and multi-professional performance in PC for the elderly |
| Hermans S, Sevenants A, Declercq A, Broeck NV, Deliens L, Cohen J, Audenhove CV 34 | Inter-organisational collaboration in palliative care trajectories for nursing home residents: A nation-wide mixed methods study among key persons | Belgium, 2019 | Sequential mixed method | • Discusses the relationship between the PC system devices such as nursing homes, hospitals, and home • Reflects on the limited production of research in this field • States that the collaboration process in PC for the elderly at the inter-organizational level is fragile • Reports that the frailties of the inter-organizational relationship are the divergence of routines, poor communication, lack of a unified information system between services, and the professionals' wrong perception of PC |
Source: Elaborated by the authors.
The results, in general, demonstrated the importance of PC practices for the elderly to be organized in the HNS, with primary healthcare, home care, and interdisciplinary coordination with the geriatrics specialty as key to the comprehensiveness and continuity of care.
Discussion
Although the articles analyzed mention the importance of inserting and discussing PC in an integrated health system, in practice, there is still fragmentation in the provision of this care, with limited considerations regarding the challenges and possibilities of the effectiveness of PC at all levels of care. We noticed that most of them choose to emphasize one of the levels of healthcare, prioritizing primary healthcare and home care. From this perspective, they understand that primary care explores the light care technologies, which include communication, welcoming, bonding, listening 35, establishing trust, and allowing more significant interaction with the elderly and their families/caregivers in the development and implementation of the care plan.
The increase in life expectancy and population aging leads the elderly to die primarily due to chronic diseases 36. With aging and the progression of these diseases, older adults tend to be subjected to unnecessary suffering, resulting in a compromised quality of life at the end of life 37,38. This happens because public health has failed to manage and follow up on the burden of non-communicable diseases in the aging population, such as chronic diseases, whose challenge is the loss of functional health 36.
From this perspective, the WHO suggests integrating and providing PC throughout the lifespan 27,39. In this review, we inferred that the insertion of PC throughout the entire HNS is a powerful strategy to promote the integration of PC practices for the elderly. In this sense, it was possible to identify in the sample initiatives and reflections that propose PC to the elderly from the perspective of an integrated healthcare system.
It is highlighted that care is a continuous process, where an individual may, at any given time, need to access more than one health system service, especially in aging populations that face the challenges of chronic diseases 40. Moreover, the continuity of care is more than only the connection between the different levels, but it also depends on the information flow regarding the assistance provided between the different services 40. In this regard, the authors 31 point out that the care provided in the different scenarios should be coordinated and easily transferable, constituting a safe and seamless care journey for the elderly and ensuring the patient's holistic experience. The successful joint operation of this system depends on an active interface between the various parts of the system 31.
A study 34 conducted in Belgium suggests that the organization of a care system is essential for the provision of integrated PC. This description is like the proposed care model of the Brazilian health system organized from the perspective of care integration through the HNS 18. However, it is noteworthy that PC integration in a system requires administrative, organizational, clinical, and service aspects that enable the continuity of care throughout all agents involved 34. Moreover, formalizing the system structure through government policies is insufficient to ensure successful inter-organizational collaboration. In practice, the collaboration process is complex. It entails overcoming challenges such as leadership, coordination, lack of critical organizational members to drive the cooperation, power imbalances, agents' varying expectations, cultural diversity, corporate governance, means of communication, and opportunities for interaction 34.
Given these challenges mentioned by the authors, it is understandable why primary healthcare has been indicated in several of the studies analyzed as the care organizer in the care system 24,26-28,31,32. Primary healthcare was recognized in such studies for its relevance in developing PC measures for the elderly. The articles explored primary healthcare considering its role as a care organizer in the system, its properties of integrating different services and prioritizing light care technologies, and its proximity and relationship with the region and home setting.
Primary healthcare engagement and participation in the coordination and continuity of care are factors that operate to maximize general health outcomes 24. Patient-centered care and continuity of care improve discussions, resulting in the unity of patient and health provider objectives for future care and improved end-of-life outcomes 26. Regarding PC at the primary level, a study carried out in the United States 24 indicated that primary care physicians are vital to providing competent PC at this level of care, with preliminary evidence that the engagement of these professionals is a source of regional variation in the standard of care offered at the end of life. The study results 24 indicate that patients who received greater engagement in primary care provided by physicians experienced fewer hospitalizations and intensive care procedures in the last six months of life and, consequently, lower healthcare costs.
Also of note is that the care provided to the frail elderly at this level of care improves patient satisfaction and reduces the transfer of the elderly to long-stay institutions and inadequate hospital admissions 31. The present study results corroborate a literature review 41 conducted on the role of primary healthcare in PC for the elderly, which indicates as benefits of PC at this level of care factors such as the improvement of symptoms manifested by patients, their satisfaction, and the reduction of hospitalizations at the tertiary level and expenses with specialized services.
However, challenges remain in the organization of the health system in primary healthcare to be overcome for incorporating PC in its scope of action, especially regarding the lack of professional training and educational activities aimed at the patients and their families 42. The importance of nurses and managers at this level of care to recognize PC opportunities that offer families and patients adequate and quality care is highlighted. Therefore, they suggest two fronts of action in this scenario: The training and discussion forum on the topic and community awareness regarding the importance of PC 42.
Still, on the importance of primary healthcare in PC, the study analyzed 27 in this review indicates that PC for the elderly should include the promotion, prevention, and rehabilitation measures, with guidelines for training volunteers and caregivers for the elderly at the primary level and considering the participation of family and society in the interdisciplinary work with the health team 27. In this sense, it is essential to emphasize that primary healthcare in PC needs a healthcare network system that offers specialized services in PC, among the other services, whose criteria for referral are the patients' needs and not only their limiting characteristics 43,44.
It was highlighted in the studies as the basic level of care for the continuity of healthcare between the different levels of care, considering the role of primary healthcare in the health system 26. It can be attributed to the fact that primary healthcare is the closest to patients, their families, and homes, the favored care location for the elderly in PC, with the possibility of better bonding and resolution 43.
Regarding the continuity of care, a study 26 analyzed in this review states the importance of every care transition of the older adults in PC (specialized consultation, hospital discharge, performance of procedures, or referral to long-term care facilities) as an opportunity for monitoring, adjustment, and definition of care goals. The authors emphasize that this is a potential developed by primary healthcare professionals, as it implies the availability of the physician's time for consultation and contact with specialists who provide care to the patient. This process is assisted by professionals at the primary level, as it is perceived that they have the time, ability, and willingness to discuss PC with patients and their families, in addition to a dynamic health team 26. Primary healthcare, in addition to centering patient care, also improves the emotional support provided to patients and their families since the professionals engage in empathic communication, promoting the discussion of the objectives of PC 26,30.
However, it should be considered that the continuity of care for the elderly in PC is still fragile due to the professionals' lack of knowledge concerning this type of care, the health system's lack of planning for the epidemiological transition with population aging, and the lack of integration between health services 41,44,45, especially when patients are transferred to hospital care and in the processes related to discharge from this service 45. Continuity of care happens effectively when the dimensions of time/environment, patient-professional relationship, communication, and management are aligned 44,45. In addition, planning, information exchange (face-to-face, telecommunication, or electronic medical records), ongoing interaction and coordination, and clear roles between services, whether for home or another level of care, are essential for the transition of care 44,45.
It is also noteworthy the emphasis of studies 29,33 on the role of primary healthcare nurses in promoting PC to the elderly. Although the multi-professional team is considered relevant, the nurses are recognized as critical agents in overcoming the limitation of PC availability in different contexts 46. Several aspects were mentioned regarding the nurses' attributes that favor their participation in end-of-life care: Their greater availability of time than physicians to be with patients; the promotion for patients to receive the best PC possible; the centrality of patients in holistic care; the competence to manage pain and other symptoms; the ability to share care with other professionals and services, focusing on the continuity of care and not only on transfer 29,33. However, the nurses' autonomy in PC is still limited, primarily associated with the referring physician, and their participation in care depends on them 33. Other studies 47-49 corroborate the present review, as they recognize the importance of nurses in PC for the elderly, especially considering their relational and technical skills. However, they emphasize the limitations of nursing work due to the lack of specialized qualifications and limited recognition by the health team.
That said, considering the epidemiological and demographic overview of the population, it is increasingly necessary to focus on healthy aging, with the comfort and well-being of patients in line with a sustainable health system, which has the home as the primary location for care 27-30. These authors indicate the importance of the home being part of the care network for the elderly in PC. In addition to being a strategy to reduce avoidable expenses for the system, society, and family, it is an environment defined by the patients and their families capable of meeting the patients' demands, which encompass more than the physical aspect, including existing relationships.
An analysis of the operational viability of PC intervention at home offered to elderly returning from intensive care units showed improvements in physical functioning, quality of life, and symptom management, leading to patient satisfaction 50. In this regard, studies 28,30 indicate that most elderly eligible for PC currently spends their end of life in hospital institutions, often against their will, due to unnecessary transfers. The health system's frailties include the absence of a health system designed for the care of chronic diseases, the impaired relationship between professionals and patients due to the short consultation time, the long wait for appointments, and the limited number of professionals dedicated to PC 27. Overcoming these frailties implies forming a system in a network, with the primary level of healthcare as the structuring line of care, with improved range, home, and families 27.
For good practices to be established at home, the authors 28-31 mention the importance of a formalized care plan with supporting information for the elderly, caregiver, and family; the need for communication, teamwork, and the availability of time and interaction with the family; the integration of a multi-professional approach rather than a physician-centered approach; the monitoring of the quality of care, requiring robust clinical governance, research, and adequate professional training; the prioritization of the bond with a team rather than several professionals and single specialists in the treatment 28-31 PC at home increases patients' and caregivers' sense of security as they must deal with life-threatening diseases in this environment 51.
Another vital aspect mentioned in studies 23,31 regarding the health network for elderly care in PC is the importance of services having interdisciplinary coordination with the geriatrics specialty as a connection to best practices, providing an integrated care approach. Regarding this coordination, a study that sought to identify barriers and enablers of integration in the European context 23 indicated that the form of organization and fragmentation of healthcare, along with the participation of several health professionals in care, seem to hinder this process. In contrast, strong leadership was identified as an enabler at both the clinical practice and the strategic and political levels. Strong leadership locally and nationally can support ongoing communication between organization members and the development of new initiatives in the integration of PC and geriatrics 23.
In a prospective controlled study 52 that compared elderly patients in home PC, followed up by primary healthcare and elderly patients who, in addition to this follow-up, received a geriatric home intervention and the availability of 24-hour geriatric service, the rate of hospitalizations and emergency care, as well as unnecessary hospitalizations after the first year of intervention, were reduced. There was an increase in the proportion of patients who died at home. The authors emphasize that although death at home was considered a favorable outcome, an integrated care model in the service network is essential so that patients who prefer or need to be hospitalized have easy access to this resource.
Also worth highlighting is the care provided to older people with dementia. In an aging society, dementia, a chronic, progressive, and terminal disease leading to complex care needs, is increasingly present. The cognitive decline caused by this disease weakens the patients' leading role in their care process, requiring intense family participation 30. Authors 25 indicate that dementia is still neglected mainly from the perspective of PC for the elderly since it is considered a natural aging condition. Person-centered care, with family participation for optimal communication and decision making, as well as training in communication skills and orientation for professionals, are still barriers to the consolidation of PC for the elderly with dementia 25. From this perspective, the ideal PC for the elderly with dementia includes discussing the prognosis and care plan with patients and caregivers, patient access to services, and standardized guidelines, as these can contribute to the first approach but may lead to the loss of patient-centered care 53.
As a study limitation, it is worth mentioning that the theme is still nascent in the literature, and only 12 articles were selected from the researched databases. In addition, the option to use DeCS and MeSH may have limited the search scope and resulted in the loss of essential documents that discussed the theme in question.
Conclusions
When mapping the scientific evidence related to the organization of PC practices for the elderly in the HNS, it is noted that, given the impact of aging on society, discussions around PC for the elderly and their families are still modest. Although the studies indicate the importance of the insertion of PC within a care network, having primary healthcare as the organizer of these practices, the concept of a network effectively established is still developing, which indicates fragmented assistance. However, the coordination between more than one level of care is eventually addressed. They also address the importance of PC being provided in the home/residence of the elderly, which favors the interface with primary care. At this level, it has the location and people's homes as the object of care.
One of the gaps identified in this review was the low number of studies published by countries that have been facing the challenges of aging, highlighting the limited discussion around solid national policies and guidelines that direct these practices. It is believed that this study can contribute to shedding light on the theme, broadening discussions that reach society, multi-professional teams, and health system managers in the search for an HNS that integrates PC at all levels of care.















