Introduction
The Acquired Immunodeficiency Syndrome (AIDS) caused by the Human Immunodeficiency Virus (HIV) has represented an extremely relevant global public health problem for over three decades. In 2020, nearly 37.7 million people were living with HIV in the world, of which 73 % had access to the treatment, and 16.18 % were unaware of the diagnosis. During the same period, 680,000 people died due to AIDS worldwide 1.
An increasing incidence of HIV/AIDS is globally noticeable in adolescence —which encompasses the age group from 10 to 19 years old— and in youth —between 20 and 24 years old 2. In Brazil, among adolescents and young people, mainly males, the number of new HIV cases increased gradually between 2010 and 2020, with a 29 % increase in the age group from 15 to 19 years old and 20.2 % between 20 and 24 years old, whose main transmission route was sexual 3. This situation can reflect the health risk behavior among this population segment, such as precocity for sexual life initiation, resistance to condom use, concurrent partners, and use of licit and illicit drugs 4.
Even with advances in the treatment of the disease, generating health benefits and better quality of life for people living with HIV/ AIDS, it is known that one of the health professionals’ most significant challenges is non-adherence to the antiretroviral therapy (ART) among adolescents and young people 5.
With the emergence of ART, HIV/AIDS presents a new clinical and epidemiological profile and is now considered a chronic condition. It is believed that, with the correct use of this therapy, among other actions, it will be possible to achieve the goals stipulated by the Joint United Nations Program on HIV/AIDS for the end of the epidemic worldwide by 2030. Among the goals were identifying 90 % of the people living with the virus, treating 90 % of the individuals diagnosed with HIV, and achieving viral suppression in 90 % of the people on ART 6.
It is noted that treatment non-adherence or abandonment is defined as the patients interrupting the intake of antiretroviral drugs, as well as the absence of follow-up in the outpatient service (team guidance, examinations, and consultations [7]). Even with many studies focused on the HIV/AIDS theme, it is clear that the reasons associated with ART discontinuation and non-adherence or its abandonment by adolescents and young people are not entirely known 8, which represents a challenge for health professionals.
Based on this context, it is believed that all the information presented in this study may assist managers and health professionals in developing strategies that improve adherence to ART in this population group. Thus, the objective of this study was to identify and map the scientific literature on the reasons for treatment non-adherence or abandonment among adolescents and young individuals living with HIV/AIDS.
Materials and method
This is a scoping review based on the recommendations set forth by the Joanna Briggs Institute (JBI), intended to structure, explore, expand, and clarify the central information that may support a given research field 9.
The option of conducting a scoping review was considered because it provides elucidation of the main concepts, definitions, characteristics, or related factors present in the literature and the gaps in knowledge about the theme under study 10.
For elaborating the review question 9, “What are the scientific literature contents on the reasons for treatment non-adherence or abandonment among adolescents and young people living with HIV/AIDS?” the “PCC” acronym (P: Population, C: Concept, and C: Context) was used, where P refers to adolescents and young people (from 10 to 24 years old); C to reasons for abandoning treatment; and C to people living with HIV/AIDS.
The bibliographic survey was in charge of two researchers who worked independently from December 2021 to January 2022, following all three stages proposed by the scoping review. It was also defined that, in case of any divergence between both reviewers, a third one would be called upon. However, there was no disagreement between the researchers. The eligibility criteria corresponded to primary studies, editorials or books and guidelines that covered the theme of treatment non-adherence or abandonment among adolescents and young people living with HIV/AIDS and which answered the review question. In addition, no limitation regarding language or publication date was established, considering the scarcity of studies related to the theme. In the first stage, a limited database search was performed to identify the keywords and descriptors used later. The second stage contemplated more encompassing research for the other databases included in the study, resorting to all the descriptors identified in the previously selected studies. The third stage consisted of searching the references of the chosen articles.
The JBI instrument 9 was used for data collection, which included the following items: title of the study, year of publication, author(s), study objective, methodological design, and main findings. Initially, the search was performed with the “HIV,” “Acquired Immunodeficiency Syndrome,” “adolescent,” “young adult,” “abandonment,” and “antiretroviral therapy highly” descriptors in the Medical Literature Analysis and Retrieval System Online (Medline) via PubMed and Web of Science databases. Subsequently, the search for the Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Base de Dados de Enfermagem (BDEnf), Scopus and Embase information sources was expanded, totaling seven sources, also known as “health databases,” with access by means of the Capes Journals Portal, through remote access via the Federated Academic Community.
It is noted that each study’s titles, abstracts, and respective descriptors were analyzed in all stages. The researchers read in full the articles that answered the review question, which had their references examined, thus ending the third step. To conduct the search strategy, descriptors controlled by the Descriptors Health Sciences (Descritores em Ciências da Saúde, DeCS) tool were used for the database in Portuguese and by the Medical Subject Headings (MeSH) for English, in addition to the non-controlled descriptors. According to the access specificities in the databases selected, the controlled and uncontrolled descriptors were crossed, using the AND and OR Boolean operators, creating the search strategy used in all databases: “patient dropouts” OR “abandonment” OR “lack of medication adherence” AND “adolescent” OR “young adult” AND “Acquired Immunodeficiency Syndrome” OR “HIV” AND “antiretroviral therapy highly active” OR “medication adherence.”
After a complete reading to evaluate the eligibility criteria, four articles that met the assumptions of this study were listed. Subsequently, their references were verified, and another four articles from the analysis of these references were listed, thus, reaching a final sample of eight that met the inclusion criteria of this study. A flowchart was prepared, which used the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR [11]) tool as a basis to ease visualization of the methodological path and selection of the studies, as shown in Figure 1.
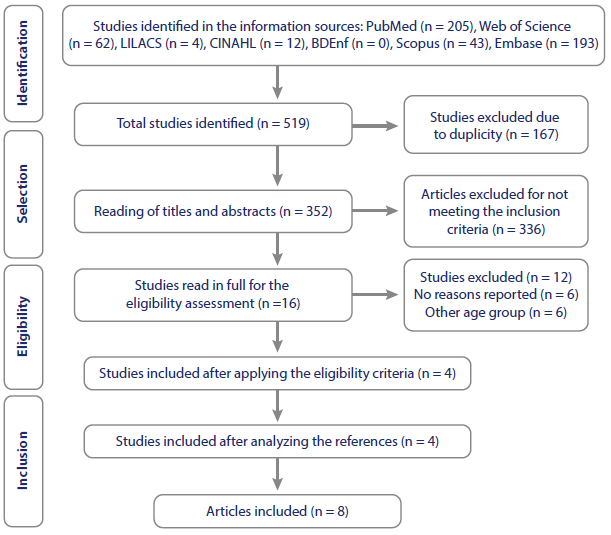
Source: Prepared by the authors
Figure 1 PRISMA-ScR Flowchart Corresponding to Identification and Selection of the Articles Included in the Scoping Review by Means of the Information Sources. Maringá, Paraná, Brazil, 2022
The study was developed following the guidelines established by Resolution 466/2012 of the National Health Council/Ministry of Health and approved by the Standing Committee on Ethics in Research Involving Human Beings under opinion No. 5,202,623 (Certificate of Presentation of Ethical Appraisal 52331221.3.0000.0104), as it is part of a more extensive study referring to a Master’s thesis.
Results
The search strategy identified 519 publications. After excluding 167 duplicates and 336 due to eligibility criteria, only 16 studies were read in full for the eligibility assessment; of these, six were excluded for not reporting reasons for non-adherence or abandonment, and six evaluated another age group. Thus, four publications were included in the complete reading phase. After reading references of the articles listed for the final sample, another eight studies were included in this scoping review.
Table 1 allows seeing the articles (A) included according to the general characteristics: author/year, title, information source (IS), which indicates where the study was made available, locus, and language. The results of this review evidenced that the articles included were developed in Botswana 12, the United Kingdom 13, Malawi 14, Kenya 15, Ghana 16, Cameroon 17, and Cape City 7, and published in the English language between 2013 and 2021.
Table 1 Presentation of the Studies Included in the Review According to Identification, Year, Author, Information Source, Locus, Language, and Level of Evidence. Maringá, Paraná, Brazil, 2022
| ID | Author/Year | Title | IS | Locus | Language |
|---|---|---|---|---|---|
| A1 12 | Ndiaye M, Nyasulu P, Nguyen H, Lowenthal ED, Gross R, Mills EJ, Nachega JB/2013 | Risk Factors for Suboptimal Antiretroviral Therapy Adherence in HIV-Infected Adolescents in Gaborone, Botswana: A Pilot Cross-Sectional Study | Reference of the articles listed | Botswana | English |
| A2 13 | Hawkins A, Evangeli M, Sturgeon K, Le Prevost M, Judd A/2016 | Episodic Medication Adherence in Adolescents and Young Adults with Perinatally Acquired HIV: A Within-Participants Approach | PubMed | The United Kingdom | English |
| A3 14 | Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN et al./2017 | High Self-Reported Non- Adherence to Antiretroviral Therapy Amongst Adolescents Living with HIV in Malawi: Barriers and Associated Factors | Web of Science | Malawi | English |
| A4 15 | Gaitho D, Kumar M, Wamalwa D, Wambua GN, Nduati R/2018 | Understanding Mental Health Difficulties and Associated Psychosocial Outcomes in Adolescents in the HIV Clinic at Kenyatta National Hospital, Kenya | CINAHL | Kenya | English |
| A5 16 | Anokye-Kumatia AB, Enimil A, Afriyie DK, Tetteh R, Mensah NK, Amo AA et al./2019 | Highly Active Antiretroviral Therapy Adherence among Perinatally Infected HIV Adolescents at a Teaching Hospital in Ghana. | Web of Science | Ghana | English |
| A6 17 | Ketchaji A, Assah F, Fokam J, Tanue EA, Monebenimp F, Ngowe MN/2019 | Predictors of Non-Adherence to Antiretroviral Therapy among Adolescents Living with HIV in the Centre Region of Cameroon | Reference of the articles listed | Cameroon | English |
| A7 5 | Van Wyk BE, Davids/2019 | Challenges to HIV Treatment Adherence amongst Adolescents in a Low Socio-Economic Setting in Cape Town | Reference of the articles listed | Cape City | English |
| A8 18 | Lantche MW, Fokam J, Cheudjui AJN, Tchatchueng JBM, Noumsi TSJ, Ateba FN et al./2021 | Factors Associated with NonAdherence to Antiretroviral Therapy among HIV-Infected Adolescents Aged 15-19 Years: A Snapshot from the Mother and Child Center in Yaounde, Cameroon | Reference of the articles listed | Cameroon | English |
Source: Prepared by the authors.
Table 2 presents the characteristics of the articles selected for this review according to identification, method, and main results about the reasons for ART non-adherence or abandonment among adolescents and young people.
Table 2 Distribution of the Articles Selected According to Identification, Method and Main Results on the Reasons for ART Non-Adherence or Abandonment among Adolescents and Young Individuals. Maringá, Paraná, Brazil, 2022
| ID | Method | Reasons for treatment non-adherence or abandonment |
|---|---|---|
| A1 12 | A cross-sectional study conducted with 82 adolescents living with HIV. | Belonging to the male gender. Forgetfulness in ART use. |
| A2 13 | A cohort study conducted with 29 adolescents and young adults living with HIV in the United Kingdom. | Failure to maintain a routine during the weekends (from Friday to Sunday). Staying out of the house for extended periods of time. Reduced self-confidence and behavioral inabilities for ART self-suggestion and self-administration. Difficulty incorporating ART into the daily routines and managing possible undesirable effects that interfere with continuous adherence. |
| A3 14 | A cross-sectional study conducted with 519 adolescents living with HIV due to vertical transmission in Malawi. | Forgetfulness in ART use. Geographical accessibility. Feeling stigmatized due to their condition or being victims of bullying due to medication use. Witnessing or suffering domestic violence. Alcohol consumption. Perception of ineffective treatment. Presence of side effects. Manifestation of depression symptoms. Sensation of overload in terms of the care demands. Hospitalizations. Non-attendance to clinical appointments to access the medication in the last six months. Other everyday demands interfere with the care routine. |
| A4 15 | A cross-sectional study conducted with 270 adolescents living with HIV and treated in a Comprehensive Care Clinic at the Kenya National Hospital, in Nairobi. | Manifestation of depression symptoms. |
| A5 16 | A cross-sectional study conducted in a university hospital from Ghana with 106 adolescents aged from 10 to 20 years old. | Forgetfulness of ART use. Access impossibility to refill medications. |
| A6 17 | A cross-sectional study conducted with 401 adolescents who underwent antiretroviral therapy in 13 health units from the Cameroon Central Region. | Vertical transmission of the virus. Medication dispensing is the same service as for adults. Geographical accessibility. Being on ART for more than 12 months and an unsuppressed viral load. Inconvenient appointments. HIV status disclosure before the 10-year time frame. Stopping the treatment on time. Presence of side effects. Not participating in actions that promote counseling and awareness raising. Being single. |
| A7 5 | This was an exploratory and qualitative study conducted through four focus group discussions with 15 adolescents monitored at a Primary Healthcare clinic in a low socioeconomic urban environment from Cape Town and followed-up with eight structured interviews with two adolescents from each focus group. | Difficulty attending the appointments for being students. Lack of financial support interfering with access to the health service. Feeling stigmatized by the family due to their diagnosis. Difficulty adapting to the health unit’s routine. Fear of involuntarily disclosing their serological status. Differentiated treatment and verbal abuse on the part of the health professionals in relation to the patients that missed the appointments. Extremely strict ART-associated treatment routine. |
| A8 18 | A cross-sectional study conducted with 191 adolescents living with HIV monitored in Yaoundé Reference Pediatric Center. | Low monthly income. Antiretroviral therapy time was less than five years. |
Source: Prepared by the authors.
Discussion
Given the findings of the survey performed, it was noticed that there were no published studies on treatment non-adherence or abandonment with adolescents and young people living with HIV/ AIDS as their population. Even without defining any time frame for data collection, it was possible to identify and map only eight articles that discussed the reasons for treatment non-adherence or abandonment among adolescents and young people living with HIV/AIDS.
In the studies included in the synoptic chart, it was noticed that the geographical distance between the home and the health service, the need to travel to have an appointment, the commute time and waiting for the consultation and acquisition of the antiretrovirals were reasons for treatment non-adherence or abandonment 5,14,16.
Geographical accessibility to health services is characterized by the possibility of the subject going to the service in search of a solution for their problem. However, easing access is directly associated with the days the care can be offered and the prospect of establishing alternative times for the patient with the possibility of unscheduled care and logistics to reach the reference locus 18,19.
The patient’s commute time to the specialized health service often exceeds hours. Thus, people living in more distant places may face accessibility challenges, as difficulties moving to access treatment aimed at HIV/AIDS —crucial to achieving total suppression— compromises adherence to the treatment in adolescents and young people, exerting adverse impacts on the lives of those with morbidity and mortality factors 8,20,21. Thus, centralization of specialized care and lack of integration with other healthcare levels, especially primary care, are considered negative factors for developing strategies and preventing and promoting actions in people living with HIV/AIDS, especially adolescents and young individuals 20.
Some sociodemographic conditions, such as being male and single, socioeconomic factors and school status proved to be associated with difficulty adhering to the treatment among adolescents and young people with HIV/AIDS 5,12,17.
The influence of biological sexual distinction, especially being male, of seeking health services less or oftentimes abandoning follow-up is due to cultural issues and access difficulties and, also, for being a period of the individual’s life characterized by the exploration of feelings that are experienced over time. However, the biological sexual distinction has implications for gender issues (sexual identity, sexual orientation, etc.) that must be considered to assist in adherence to the treatment. Thus, it becomes indispensable that these young people are encouraged to stick to the treatment and, when seeking health services, feel welcomed by the health professionals 22.
In addition to that, regarding sexual orientation, men who have sex with men aged from 15 to 24 years old are at a higher risk of HIV infection when compared to young heterosexual and older men 23. This is even more so when associated with factors of greater vulnerability, such as lack of access to information on health education and preventive strategies for unprotected sex, pre-exposure prophylaxis and sex with multiple partners without an HIV testing history 24,25.
Marital status has influenced the follow-up of the treatment of patients with HIV/AIDS, in which single people are more likely to abandon treatment when compared to those who have partners. This data can be justified by the fact that individuals with partners receive more support and are more motivated by them to avoid transmission of the virus. In addition, it can be related to the need to achieve viral suppression have children without them being at risk of HIV infection 26.
Socioeconomic differences are widespread in developing countries. Reductions in social inequalities are a challenge for public policies, mainly in places experiencing an economic, political, or social crisis 27. The increase in new HIV infections and changes in the funding landscape cause the global health community to accelerate the development of early HIV diagnosis to complement existing HIV prevention measures 28. In addition, the absence of financial support negatively implies family dynamics and hinders adherence even more when low socioeconomic status is related to lower schooling levels and understanding of the real importance of the treatment. Thus, it becomes necessary to follow the equality principle based on developing care strategies to monitor all young people in the specialized service 27,29.
The factors related to the presence of adolescents or young people in school environments, such as their commitment to studying and the professors’ attitudes regarding possible absences of these students, may hinder attendance in outpatient consultations and ART adherence 7. However, secrecy and confidentiality about the HIV diagnosis have been an ethical foundation that ensures the preservation of the person’s integrity, especially of people living with HIV/ AIDS, due to the social stigma faced due to the diagnosis 30.
The complexity of living with HIV/AIDS in adolescence and youth has been triggered by changes in everyday life imposed by the chronic condition, fostering feelings and behaviors that interfere with social, personal, and family relationships. Therefore, health education actions and strategies aimed at this problem are urgently needed to alleviate the social stigma and prejudice imposed by society 8.
It is important there is a collaboration between managers, health professionals and the community for accurate information about HIV/AIDS to be disseminated to society and for this to contribute to a better understanding of this condition (31, 32). One of the existing strategies to safely contribute knowledge is using mobile apps and social marketing based on reliable and safe scientific evidence, but that can be taken to the lay community. Thus, increasing the knowledge related to HIV/AIDS may reduce stigma and prejudice 33.
The studies pointed out that some adolescents and young people did not regularly attend their medical appointments and did not pick up the medications as recommended. This lack of attitude reflects the reality of many young people, as the search for autonomy, active social life and educational and financial responsibilities compete with involvement in HIV care.
The stigma faced by adolescents and young people living with HIV/ AIDS, both in the family and society, was listed as a reason for non-adherence to the treatment. The exclusion from the family for being people living with HIV, the presence of violence at home, the fear of involuntary disclosure about their serological status, non-welcoming by the professionals due to absences in previously scheduled appointments and non-withdrawal of medications are recurrent justifications for young people to abandon treatment 5,14.
The importance attributed to stigma is closely linked to the dimensions that impact the health and well-being of this population group. In addition to that, feelings of shame or guilt about living with the infection (internalized stigma) and that person’s mood state (depression) significantly impact their health. Thus, there is a relationship between stigma and self-rated health, mediated by internalized stigma and depression, which consequently affect the decision to continue or not the treatment and to maintain or abandon ART. It is noted that the discrimination and stigma experienced by people living with HIV/AIDS, especially adolescents and young people, cause problems with their mental health. The overlap of different stigmas they experience triggers certain exacerbation of sensitivity, which contributes to negative results for their health, leading these individuals not to seek the specialized health service and not to adhere to the treatment 34.
Domestic violence is among the causes that negatively affect patients’ adherence to treatment. Some adolescents and young people experience violence among members of their own families. In addition to that, domestic violence is an indicator of suffering, in which drug administration is not a priority. Thus, young people who experience violence may suffer emotionally to the point of showing depressive signs, which increases the chance of interrupting the HIV/AIDS treatment 35. Despite the difference between both age groups 4, adolescents and young people share the same risk characteristics for violence, such as vulnerability related to changes in cognitive, physical, social, emotional and sexual development 36.
Another point that deserves attention is the fact that adolescents and young people are reprimanded negatively by health professionals when they miss appointments or do not pick up the medications. Thus, these individuals do not feel welcomed by the health service and are intimidated to continue the monitoring program 37.
It should be noted that there are many symbolic constructions around HIV/AIDS that reflect how health professionals have been developing strategies for everyday life and their experiences with the care of people living with the infection. Therefore, it raises the importance of strengthening permanent education actions among health professionals to broaden the reflection on the management of patients and their treatment in specialized services, ensuring improvements in the care actions 36 and, consequently, reducing abandonment and strengthening adherence to treatment and monitoring.
Gender issues that interfere with adherence to the treatment reflect historically evidenced situations in which ethnic and racial minorities, sexual minorities and low-income individuals experience worse health results and social conditions, which lead to negative results for their health 37.
In addition to that, depressive symptoms, alcohol use, changing routines, forgetting to take the medication, and frequent hospitalizations are common reports among adolescents and young people who abandon the treatment 5,12,14,16).
The effect of depression and the sensation of being overwhelmed reflect on health, implying harm to the person. Mild and moderate depression were present in 31.5 % and 21.3 % of the patients diagnosed with HIV/AIDS, respectively. This shows that HIV/AIDS can affect mental health and may even hinder treatment adherence, consequently increasing the progression of infection 38.
Alcohol use is also pointed out in most studies as the main factor contributing to the risk of non-adherence to follow-up among adolescents and young people living with HIV/AIDS who interrupt the treatment to consume the substance 39.
Many participants did not regularly use antiretrovirals more than once a month due to forgetting to take the medication. This factor corresponds to one of the leading causes of non-adherence. In addition to that, during the weekends, getting out of the routine and being away from home also ease forgetfulness about using the antiretrovirals 12,13.
It is noteworthy that prejudice has collaborated to non-adherence, becoming a social problem. Family support for treatment is considered of great value, as it improves adherence to the antiretrovirals in a relevant way. However, eventually revealing the diagnosis to family or friends can lead to negative outcomes and non-acceptance. For this reason, people frequently find it difficult to share their diagnosis due to the prejudice against people living with HIV and using antiretrovirals, directly interfering with adherence and making their adherence to secrecy less embarrassing 39.
Even so, one of the reasons for hospitalization among adolescents and young people can be related to untreated HIV/AIDS, which consequently increases the cases of repeated infections. The age group between 10 and 24 has the highest follow-up loss rates and worst virological results 40. It is essential to highlight that, in addition to demographic and clinical factors, socioeconomic disadvantages, social circumstances, mental health disorders and adverse lifestyles are also factors for hospitalization 41.
It was noticed that ART abandonment could be related to the infection itself and to the medications, such as the fact that the adolescents and young people were infected by vertical transmission, the absence of clinical consultation in the last six months, taking the medication in the same service with an adult, antiretroviral therapy time being less than five years, low self-efficacy in treatment, the treatment routine, and the presence of side effects 5,13,17.
Vertical transmission only appeared in one study as a predictor for treatment non-adherence or abandonment. This reason can be due to the follow-up carried out in specialized pediatric clinics since the discovery of the virus, generally at birth, when the child is stimulated to collaborate with the treatment and made aware of the importance of the therapy for its total growth and development 42.
However, even in this context, there are results in which vertical transmission is seen in non-adherence to the therapy 17. This condition can be related to postponing the diagnosis by parents or legal guardians, as around 20 % of adolescents ignore their health condition and frequently discover it at conflicting moments and are full of insecurities while being educated on good sexual practices 42. Discovery of the diagnosis of a stigmatizing disease such as HIV can provoke feelings of fear and revolt, especially in adolescents, who experience biopsychosocial changes, a fact that can lead to non-adherence to the treatment.
The fact that vertical transmission is a factor for treatment abandonment reinforces that the adolescent and young population is vulnerable regarding HIV/AIDS; therefore, specialized care needs to be attentive to successfully ensure the transition from pediatric to adult care 43.
It has been noticed that the profiles of the patient’s conditions and treatment patterns seem to vary according to transmission mode; thus, identification of HIV disease progression and the determinants of access to treatment among adolescents and young people can assist in understanding the outcome in adherence or abandonment 44.
Among the healthcare factors for young people, taking medication in the same service as adults and not being regularly advised by health professionals reflect non-adherence to treatment; this suggests that specialized care professionals are attentive to the patient’s needs and preferences to ensure adherence 45.
Also, considering medication, some patients are more sensitive to the drugs and, consequently, are at a higher risk of negative treatment results, which can be explained by the side effects and intentional non-adherence. Such fact has impacted general adherence to ART and in the HIV viral load 46.
The absence of HIV/AIDS follow-up clinical consultations, that is, lack of monitoring and clinical treatment, has been a predictor of abandonment, which suggests the strengthening of the active search for missing patients at the beginning of the follow-up period to reduce morbidity, re-engage them in HIV/AIDS care and improve their maintenance and adherence to the service. The extended duration of the treatment has also contributed to non-adherence. Thus, it becomes necessary for health professionals to (re)think and (re)devise actions and strategies to optimize adherence to ART to keep patients engaged in their HIV/ AIDS treatment 47.
The use of highly active ART has been essential in managing viral replication, where adherence to the therapy is fundamental for such control. External and individual factors in relation to the patient influence treatment adherence and abandonment. In environments where resources are limited, approximately three-quarters of the adolescents may not adhere to ART, in addition to late diagnoses that may reflect in adherence 17.
A study conducted in India shows that nearly 20 % of the patients had HIV symptoms for more than six months, which indicates the absence of HIV screening practices, consequently causing delays in diagnosis and ART initiation. In addition to that, some patients delay going to the antiretroviral delivery service; such context can be due to the absence of adequate communication with the patients or to the service’s unavailability, resulting in faster progression and a worse evolution of the disease 44.
The low self-efficacy and the rigid treatment routine for adolescents and young people reflect non-adherence. Part of HIV/AIDS care and management has involved changes in the treatment with an ART regimen with possible failures for another class of antiretrovirals. However, it is known that these regime changes are fundamental to achieving and maintaining virological suppression without compromising future treatment options 45.
A study conducted in South Korea identified that second-generation antiretroviral medications or single-pill regimens presented lower toxicity and viral resistance rates, contributing to better medication adherence and viral suppression effect. As patients living with HIV/ AIDS have a longer life expectancy, it becomes increasingly essential to manage medication adherence 48.
Given this context, health professionals, especially nurses, should evaluate adherence in various aspects, ensuring and respecting the individuality and vulnerabilities of people in specialized healthcare services. The knowledge about the existing influences regarding non-adherence to ART allows Nursing professionals to establish care directed to people diagnosed with HIV/AIDS to improve their quality of life and promote care continuity and adherence to ART through comprehensive care 49.
It is known health professionals are aware that adolescents and young people living with HIV/AIDS have specific health needs unique to the age group and should be treated through services aimed at this population segment and guided by scientific information 50,51.
Despite the limitation demonstrated by the small number of studies included in the sample, they were relevant to the reflection on treatment abandonment among adolescents and young people living with HIV/AIDS. Additionally, all the information in this study may help not only health professionals within the service but also undergraduate students and society interested in comprehensive healthcare in key or minority population groups.
Conclusions
The findings of this study evidenced how vulnerable adolescents and young people are to the issues inherent to the treatment even more when living with HIV/AIDS and that several reasons can influence adherence or abandonment.
The research contributes to the health professionals’ practice because it offers subsidies to understand the realities experienced by the individuals who abandon treatment. Furthermore, the study’s findings show the need to conduct further research on non-adherence to ART or its abandonment, both with those living with HIV/AIDS and with health professionals, to understand the phenomenon of HIV/AIDS treatment abandonment.















