Introduction
The number of people with some type of disability is high. It is estimated that 1.3 billion people (16 % of the world population) will have some disability in 2023. People with disabilities (PwD) die prematurely, present worse health conditions, and need more health care. In addition, they face inequalities in access to health services 1-4.
Stroke represents one of the main causes of death, disabilities, and hospitalizations worldwide. It is estimated that 70 % of the cases occur in low-and middle-income countries. From 1990 to 2019, the number of stroke cases increased substantially: 102 % prevalence, 70 % incidence, 43 % deaths, and 143 % disability-adjusted life years lost 1,5,6.
Regarding cranioencephalic trauma, it stands out as one of the causes of morbidity and mortality for external reasons and long-term disability among young adults 2,7. Mortality is high in low- and middle-income countries, and sociodemographic factors such as race and schooling level played an important role in that result 7. Spinal Cord Injury (SCI), on its part, affects nearly 500,000 people worldwide; urban violence constitutes the most common cause for this type of lesion, which in most cases compromises the individual with serious and disabling sequelae 3,8,9.
In this context, some people with motor disabilities after an acquired neurological lesion are in situations of greater vulnerability to secondary health conditions, which are physical and psychosocial health conditions associated with the primary disability, such as complications, comorbidities, and other conditions after the disability 10-14. Such conditions can exert a major impact on health and well-being 14,15, compromise the quality of life, and lead to hospitalizations and premature death 14,16,17, especially when there is no adequate intervention for the person or family 18. At a global level, 95.8 % of the individuals with SCI report having experienced at least one secondary health problem that might be reduced or prevented 13.
Meleis’ Nursing Theory of Transitions reveals that people who are in an adjustment process are more vulnerable. In turn, transition means “changes,” whether in health status or the role or skill relationships. According to the theory, a person in this process needs care targeted at a healthy transition; in other words, to better health conditions and to better cope with this situation. For this, it is necessary to understand the experiences regarding how each individual undergoes their transition process considering the “personal” aspect: meanings, attitudes, beliefs, and knowledge; the “social” aspect: social reintegration, stigmas, gender inequalities, and stereotyping, and the “community” aspect: aid and support, and availability of information and human/material resources for health care 18.
In the collective health view, according to Ayres, vulnerability can be understood in a broad and multidimensional way. This is people’s chance of exposure to diseases and health problems and, consequently to illness, considering individual aspects, that is, the conditions a person has to protect themselves in a given social context and of access to public policies, in the programmatic scope. Unlike risk, vulnerability seeks to analyze a set of the various factors involved in people’s health-disease process 19.
In this perspective, the validation of a scale based on the concept of Ayres and Meleis’ Nursing Theory of Transitions is justified to identify the situation of vulnerability of people with motor disabilities after an acquired neurological lesion (EVU-PcD scale). Identifying the situation of vulnerability can guide nurses in the care and development of actions to prevent complications, comorbidities and other secondary health conditions throughout life in PwD after the acquired neurological lesion (18, 19), also favoring comprehensive and individualized care for this group. However, the lack of knowledge about constructs that involve the vulnerability of PwD after suffering a neurological topography lesion is highlighted and, consequently, the absence of a specific instrument that provides information about this situation 20.
It is expected that the EVU-PcD scale proposed may be used in research studies and nursing professionals’ practice, both in the primary care context and in specialized rehabilitation centers, which broadly contributes to health promotion, as well as to the rehabilitation of PwD after a neurological lesion.
Rehabilitation nursing care is fundamental, regardless of the disease or motor/sensory disabilities, aiming to promote independence and autonomy, developing strategies for self-care, quality of life and prevention of complications and for social inclusion 17,21,22. In this sense, the objective was to validate the EVU-PcD scale.
Materials and Methods
This was a methodological development and psychometric study with a quantitative approach. For construct validity, a cross-sectional study was conducted from July 2019 to February 2020 in a specialized rehabilitation center located in the city of Campina Grande, Paraíba, Brazil. According to the Brazilian Institute of Geography and Statistics, the Northeast Region has the highest percentage of PwD 23.
The probability sample was estimated with the aid of the Epi Info 7 software. THz following was considered for the calculation: the population of people with motor disabilities at the specialized rehabilitation center (N = 2,116), the tolerated error (e = 0.05), the prevalence of people with physical disabilities in the city of Campina Grande (P = 7.14), and 95% confidence. A total of 97 individuals was obtained after the calculation. Subsequently, with a 5 % correction applied for losses inherent to the sample selection process, the result was a sample comprised of 102 users with motor disabilities. Simple random sampling was used, drawing from the users’ medical records. The reference by Hair Junior 24 was adopted for sample size, which suggests a sample size equal to or greater than 100 in factor analyses.
The inclusion criteria were being aged from 18 to 59 years old and presenting some motor disability arising from an acquired brain and/ or SCI. People with neurodegenerative neurological diseases were excluded, as they comprise a more specific group that progressively loses functional capacity, in addition to those with psychiatric diseases diagnosed by a specialist, people with altered cognition and hospitalized patients during the research period.
The construct validation study stages were as follows: applying EVU-PcD; performing a reliability analysis using Cronbach’s alpha; and carrying out a Confirmatory Factor Analysis. The EVU-PcD was created in Brazilian Portuguese, with 60 items, and validated in terms of content by nine experts from Brazil. The Content Validity Index (CVI) corresponding to the scale items evidenced 38 valid items, with a minimum agreement of 0.80. The binomial test acknowledged agreement of all 38 items with a p-value>0.05. The significance level adopted was 95 %.
The EVU-PcD has 38 items and consists of three domains: “Personal,” with 19 items (from 1 to 19); “Social,” with 13 items (from 20 to 32); and “Community,” with six items (from 33 to 38). Conserning the EVU-PcD answer format, a Likert-type scale with five self-reported options was used, namely: 0 - Never, 1 - Rarely, 2 - Sometimes, 3 - Frequently and 4 - Always, for items with a positive denotation; and 4 ― Never, 3 ― Rarely, 2 ― Sometimes, 1 ― Frequently and 0 ― Always, for those with a negative one. The lower the score, the greater the situation of vulnerability.
Data collection took place by applying EVU-PcD to users who met the eligibility criteria and agreed to participate in the study, formalizing their consent by signing the free and informed consent terms. The collection procedures took place before the users were assisted at the specialized rehabilitation center or after that in a private place, or, for those who were not attending the center, home visits were also carried out.
The set of data inherent to the research was initially tabulated in Microsoft Excel from the Office package and later incorporated into the SPSS software (Statistical Package for the Social Sciences) to carry out the entire pre-processing, descriptive and reliability analysis phases. The Confirmatory Factor Analysis was performed with the aid of the R software, version 4.2.1, resorting to the “ltm”, “lavaan” and “semplot” packages.
Absolute and relative frequencies were calculated in the descriptive analysis. Cronbach’s alpha was used to assess reliability and measure internal consistency. Minimum, total and by domain alpha values ≥ 0.7 were considered 24.
In the Confirmatory Factor Analysis, the estimation between items and factors was analyzed using the Critical Ratio test, considering p<0.05 as significant. The EVU-PcD factor structure hypothesis test was performed by implementing the structural equations model for latent variables, using a path diagram. For the implementation of structural equations modeling, the “Personal” (Factor 1), “Social” (Factor 2) and “Community” (Factor 3) factors were considered as latent variables, and the observed variables corresponded to the 38 items of the EVU-PCD scale.
To test the quality of the fit to the structural model, the χ2/DoF ratio, RMSEA, TLI, Comparative Fit Index (CFI) and PGFI were estimated. The following values were considered acceptable: TLI and CFI ≥ 0.90; RMSEA from 0.05 to 0.08; PGFI ≥ 0.6; and χ2/DoF between 1 and 5 25.
The ethical and legal aspects considered in the National Health Council Resolution No. 466/2012 were safeguarded for compliance with the guidelines and regulatory standards for research studies involving human beings. The project was approved by the Research Ethics Committee of Universidade Estadual da Paraíba under Opinion number 3,401,254. The research participants were guaranteed data secrecy and anonymity.
Results
Among the 102 individuals with motor disabilities after neurological lesions, there was a predominance of men, with low schooling levels, without a partner, low incomes and limited access to work, as well as people with acquired brain injuries, with less than one year since the lesion.
The reliability of the 38-item EVU-PcD scale before factor analysis showed a total Cronbach’s alpha of 0.86, considering that, by domain, the alpha value corresponded to 0.79 in the “Personal” domain, 0.75 in the “Social” domain, and 0.48 in the “Community” domain.
Regarding the confirmatory factor analysis, the estimate between items and factors showed that items P7 (p = 0.169), P11 (p = 0.139), P12 (p = 0.816) and P15 (p = 0.829) related to Factor 1; P21 (p = 0.207), P26 (p = 0.086) and P27 (p = 0.587) related to Factor 2; and P34 (p = 0.252) and P35 (p = 0.059) related to Factor 3, did not present significance, thus being removed from the first model. In a subsequent analysis with the second model, one non-significant item (P24, p=0.061) related to Factor 2 was obtained, thus removing it. In the third analysis, a third model comprised of 28 statistically significant items was obtained, as presented in Table 1.
Table 1 Estimate between Items and Factors from the Final Structural Model of the Vulnerability Scale for People with Motor Disabilities after an Acquired Neurological Lesion (n = 102), Campina Grande, Paraíba, Brazil, 20192020 (Free translation into English)
| Item | Estimate | Error | z | value* |
|---|---|---|---|---|
| P1. Do you take care of yourself as you would like to (for example: eating, taking a bath, getting dressed, going to the bathroom, taking care of personal hygiene? | 1.000 | |||
| P2. Do you perform your activities of daily living on your own (Example: shopping, household chores, managing your own money, using the telephone? | 1.178 | 0.161 | 7.311 | <0.001 |
| P3. Does tiredness prevent you from performing any activity you would like to do? | 0.570 | 0.156 | 3.655 | <0.001 |
| P4. Do the strategies you use to do what you need work? | 0.941 | 0.139 | 6.774 | <0.001 |
| P5. Do you accept your condition as a person with a disability? | 0.961 | 0.160 | 5.995 | <0.001 |
| P6. Do you feel rehabilitated given your new life condition? | 0.750 | 0.154 | 4.868 | <0.001 |
| P8. Do you feel satisfied with your sexuality? | 0.369 | 0.147 | 2.513 | 0.012 |
| P9. Do you feel capable of taking care of your health? | 1.171 | 0.171 | 6.863 | <0.001 |
| P10. Do you practice any type of physical activity? | 0.531 | 0.147 | 3.612 | <0.001 |
| P13. Do you sleep the necessary number of hours to feel good and recovered every day? | 0.586 | 0.146 | 4.022 | <0.001 |
| P14. Do you feel stressed? | 0.564 | 0.136 | 4.154 | <0.001 |
| P16. Can you eliminate feces in a spontaneous and controlled way? | 0.255 | 0.124 | 2.049 | 0.040 |
| P17. Do you change positions on your own or with help to avoid skin wounds? | 0.115 | 0.058 | 1.985 | 0.047 |
| P18. Do you have positive feelings (for example: trust, optimism, motivation)? | 0.398 | 0.111 | 3.578 | <0.001 |
| P19. Do you have negative feelings (for example: fear, anxiety, frustration, or sadness)? | 0.461 | 0.116 | 3.957 | <0.001 |
| P20. Do you have enough money to meet your needs? | 1.000 | |||
| P22. Do you feel capable of doing your job? | 2.477 | 1.015 | 2.440 | 0.015 |
| P23. Can you access the labor market? | 2.131 | 0.860 | 2.478 | 0.013 |
| P25. Do you feel that you are a burden to your family? | 1.206 | 0.579 | 2.081 | 0.037 |
| P28. Do you use transportation means on your own? | 2.638 | 1.074 | 2.457 | 0.014 |
| P29. Do you take part in social activities as you would like to? | 2.443 | 0.982 | 2.488 | 0.013 |
| P30. Do you have good family relationships? | 0.872 | 0.435 | 2.006 | 0.045 |
| P31. Do you have good friends? | 1.565 | 0.685 | 2.284 | 0.022 |
| P32. Do you take part in leisure, cultural or artistic activities, among others? | 2.024 | 0.814 | 2.485 | 0.013 |
| P33. Do you seek health assistance to remain healthy? | 1.000 | |||
| P36. Do you make your health-related decisions with the support of health professionals? | 1.117 | 0.345 | 3.240 | 0.001 |
| P37. Do you feel that you have sound information about your health? | 1.450 | 0.420 | 3.450 | 0.001 |
| P38. Do health professionals provide you with guidelines about how to avoid complications after the neurological lesion? | 1.182 | 0.374 | 3.164 | 0.002 |
Source: Prepared by the authors.
Notes: *p<0.05.
The following was obtained for the quality fit indices of the model: Chi-square by degrees of freedom (χ2/DoF) of 1.63; RMSEA of 0.08; and PGFI of 0.61. CFI was 0.73 and TLI was 0.70. It was shown that the fit indices, chi-square ratio, RMSEA and PGFI presented acceptable indicators of adequacy to the final model. Consequently, the third model (comprised of 28 items), defined the best fit for the final model.
Figure 1 presents the final structural model, which proved to present a good fit. Greater distribution of items with a strong influence on the factors was observed. P4, P8, P16, P17, P18, P20, P25 and P30 exerted lower influences. The relationship between the latent variables is unidirectional, as well as the one between the factors under study is more intense, between F2 (“Social”) and F1 (“Personal”), between F3 (“Community”) and F2 (“Social”) and between F3 (“Community”) and F1 (“Personal”).
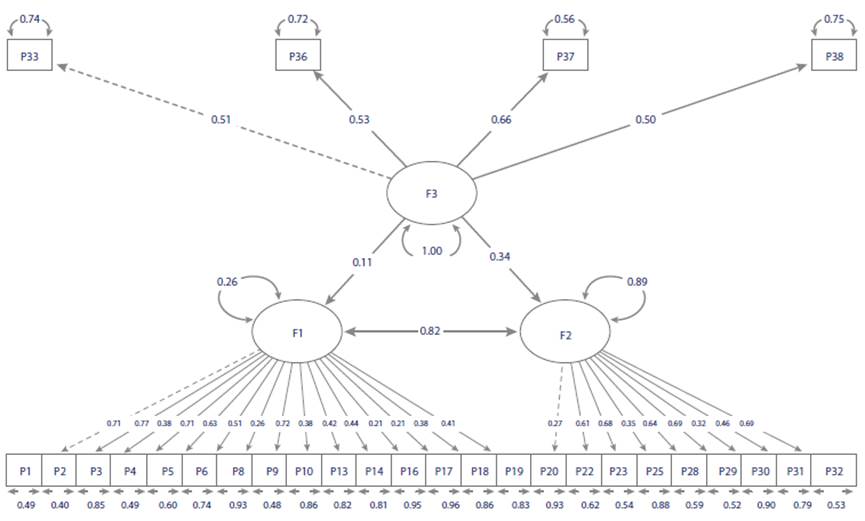
Source: Prepared by the authors. *F1: Factor 1 (“Personal”), F2: Factor 2 (“Social”), F3: Factor 3 (“Community”).
Figure 1 Path Diagram Corresponding to the Final Structural Model of the Vulnerability Scale for People with Motor Disabilities after an Acquired Neurological Lesion (n = 102), Campina Grande, Paraiba, Brazil, 2019-2020
After defining the final model, the internal consistency of the EVU-PcD scale was tested again; it revealed an increase in the total Cronbach’s alpha from 0.86 to 0.87 and, by domain, the alpha values were 0.82, 0.76, and 0.64 for the “Personal”, “Social” and “Community” domains, respectively. The final version of the reliable and valid EVU-PcD scale is presented in Table 2.
Table 2 Final version of the Vulnerability Scale for People with Motor Disabilities (in Portuguese) after an Acquired Neurological Lesion (n = 102), Campina Grande, Paraíba, Brazil, 2019-2020
| Escala de vulnerabilidade de pessoas com deficiência motora após lesão neurológica adquirida | |||||
|---|---|---|---|---|---|
| As questões nesta escala estão relacionadas com as suas experiências após lesão neurológica. Por favor, indique a frequência com que ocorrem as seguintes situações no seu dia a dia: | Nunca | Raramente | ALgunas veces | Frequentemente | Sempre |
| Domínio “pessoal” | |||||
| 1. Você cuida de si mesmo(a) como gostaria (exemplo: alimentarse, tomar banho, vestirse, ir ao banheiro, cuidar da higiene pessoal)? | 0 | 1 | 2 | 3 | 4 |
| 2. Você realiza sozinho(a) suas atividades diárias (exemplo: fazer compras, realizar tarefas domésticas, gerir o próprio dinheiro, usar telefone)? | 0 | 1 | 2 | 3 | 4 |
| 3. O cansaço lhe impede de realizar alguma atividade que gostaria? | 4 | 3 | 2 | 1 | 0 |
| 4. As estratégias que você utiliza para fazer o que precisa funcionam? | 0 | 1 | 2 | 3 | 4 |
| 5. Você aceita a sua condição de pessoa com deficiência? | 0 | 1 | 2 | 3 | 4 |
| 6. Você se sente reabilitado(a) diante da sua nova condição de vida? | 0 | 1 | 2 | 3 | 4 |
| 7. Você está satisfeito(a) com a sua sexualidade? | 0 | 1 | 2 | 3 | 4 |
| 8. Você se sente capaz de cuidar da sua saúde? | 0 | 1 | 2 | 3 | 4 |
| 9. Você pratica algum tipo de atividade física? | 0 | 1 | 2 | 3 | 4 |
| 10. Você dorme diariamente o número de horas suficientes para se sentir bem e recuperado? | 0 | 1 | 2 | 3 | 4 |
| 11. Você se sente estressado(a)? | 4 | 3 | 2 | 1 | 0 |
| 12. Você consegue eliminar as fezes de maneira espontânea e controlada? | 0 | 1 | 2 | 3 | 4 |
| 13. Você realiza mudança de posição, sozinho(a) ou com ajuda, para evitar o aparecimento de feridas na pele? | 0 | 1 | 2 | 3 | 4 |
| 14. Você tem sentimentos positivos (exemplo: confiança, otimismo, motivação)? | 0 | 1 | 2 | 3 | 4 |
| 15. Você tem sentimentos negativos (exemplo: medo, ansiedade frustração, tristeza)? | 4 | 3 | 2 | 1 | 0 |
| Domínio “social” | |||||
| 16. O seu dinheiro é suficiente para satisfazer as suas necessidades? | 0 | 1 | 2 | 3 | 4 |
| 17. Você se sente capaz de realizar o seu trabalho? | 0 | 1 | 2 | 3 | 4 |
| 18. Você tem acesso ao mercado de trabalho? | 0 | 1 | 2 | 3 | 4 |
| 19. Você sente que sobrecarrega sua família? | 4 | 3 | 2 | 1 | 0 |
| 20. Você utiliza os meios de transporte sozinho(a)? | 0 | 1 | 2 | 3 | 4 |
| 21. A sua participação nas atividades sociais ocorre como gostaria? | 0 | 1 | 2 | 3 | 4 |
| 22. Você mantém um bom relacionamento familiar? | 0 | 1 | 2 | 3 | 4 |
| 23 Você mantém boas relações de amizade? | 0 | 1 | 2 | 3 | 4 |
| 24. Você participa de atividades de lazer, culturais, artísticas etc.? | 0 | 1 | 2 | 3 | 4 |
| Domínio “comunitário” | |||||
| 25. Você procura assistência à saúde para se manter saudável? | 0 | 1 | 2 | 3 | 4 |
| 26. Você toma suas decisões em saúde com apoio de profissionais de saúde? | 0 | 1 | 2 | 3 | 4 |
| 27. Você sente que é bem-informado(a) sobre a sua saúde? | 0 | 1 | 2 | 3 | 4 |
| 28. Você recebe orientações dos profissionais de saúde sobre como evitar as complicações após lesão neurológica? | 0 | 1 | 2 | 3 | 4 |
Source: Prepared by the authors.
Discussion
The confirmatory factor analysis with acceptable fit indices (χ2/ DoF, RMSEA, PGFI) and satisfactory reliability by the total Cronbach’s alpha resulted in construct validity of the EVU-PcD scale, comprised of 3 domains and 28 items in its final version.
Characterization of the sample, with a mean age of 44 years old and predominance of men, brown-skinned, married, with elementary school education, unemployed, and with low socioeconomic status corroborates with national and international studies 2,9,26.
Regarding the clinical data, motor sequelae can reduce the functional capacity of individuals affected by neurological lesions, limiting their independence and autonomy and, consequently, their quality of life 17; they also contribute to depression, difficulties returning to work, low socioeconomic status, social activities and accessibility 5,26-28.
In this context, it is necessary to present the sociodemographic and clinical characteristics to show the validity of the EVU-PcD scale focused on a given situation and for a given purpose. As the psychometric parameters are not fixed, they can change according to the population characteristics 29.
Concerning the analysis of the psychometric properties, Cronbach’s alpha results showed excellent internal consistency between the items and the scale at the global level and, consequently, its reliability, according to parameters reported in the literature 24. In addition to that, removing any of the items did not exert any significant influence on the alpha value of EVU-PcD.
From the final structural model, in the confirmatory factor analysis, internal consistency was considered with even more satisfactory Cronbach’s alpha values, showing how reliable the final EVU-PcD scale was. Internal consistency meant asserting the items are inter- and correlated, although it does not mean that they are measuring the same construct. To such end, it was indispensable to apply factor analysis to validate the construct 29.
Confirmatory factor analysis was necessary to confirm the structural model, pre-established in the light of Meleis’ Theory of Transitions, the concept of vulnerability and integrative review, which reflected vulnerability through three domains (“Individual/Personal,” “Social/Society”, and “Programmatic/Community”). Through structural equations modeling, the Confirmatory Factor Analysis proposed to analyze to which extent the latent and observed variables approached reality, as empirically observed, and thus validate the results generated by EVU-PcD 24,25,30.
Another study is similar to the elaboration and validation stages: the questionnaire on interpersonal relationships in Nursing care, which followed the three procedures proposed by Pasquali’s psychometry: theoretical, empirical and analytical. In this study, Imogene King’s Nursing theory was used to support the definition of the construct, CVI to validate the content, and Cronbach’s alpha and factor analysis to validate the construct of the questionnaire items, which were adequate reliability and validity parameters 31.
The nine non-significant items specified which of them were not related to the construct. This verification may have been due to the lower frequency of “Never” and “Rarely” answers for these items, thus weakening their estimates. For this reason, it is believed that applying the EVU-PcD to a larger sample may reduce the error and increase the estimate 24.
With the acceptable fit indicators of the EVU-PcD model (χ2/DoF, RMSEA and PGFI), the hypothesis that the pre-established model represents the construct is confirmed. Such indices are typically considered in a Confirmatory Factor Analysis, thus enabling the validity of the model 24. The TLI and CFI indices, both comparison indicators, are sample-size-sensitive indices; therefore, the EVU-PcD application in a larger sample may increase the indicators, thus obtaining acceptable values 24,25.
A study on the validation of the Three Factors Influence Scale applied to university students, used similar indices in the analysis (χ2/DoF = 2.97, RMSEA = 0.08, CFI = 0.87, TLI = 0.86), evidencing an adequate instrument to measure the construct 32.
After defining the final structural model, there was an increase in the overall and by domain Cronbach’s alpha values. This result showed that the reliability of the 38-item EVU-PcD scale was not influenced by the number of items since, even when removing one-third of them, there was an improvement in the coefficient estimate, evidencing better consistency between the items of the final scale. Validation of the construct under study, the EVU-PcD scale, constitutes a major advance for the praxis and for research in the Rehabilitation Nursing field, evolving health care for people with motor disabilities, who need to have their health problems investigated and, above all, nursing care focused on and specific to their health needs 33.
Diverse evidence points to the need for services and interventions for the prevention of secondary health conditions in PwD with lifelong acquired motor disabilities (15, 34); this type of prevention should be a priority to improve PwD’s experience and health 35. For this purpose, it is of utmost importance to adopt an interdisciplinary approach and holistic care to minimize the impact of such conditions 34. In addition, effective technologies and training are necessary to better support vulnerable populations 36.
It is worth noting that Nursing professionals’ performance is significant in a person’s transition process after a neurological lesion, from hospitalization to the post-discharge discharge, at home and with full care continuity, that is, at all health care levels 37, in the rehabilitation of people undergoing health-disease transition processes for the development of skills and coping after acquired neurological lesions 38.
The study limitations correspond to the sample size and to the number of items in the Community factor in the final model, events that may have influenced its relationship with other factors (Personal and Social) and the values of the CFI and TLI quality indices. Therefore, reproducibility analyses such as test-retest need to be collected, in search of a greater understanding of the situations that predispose PwD to secondary conditions after a neurological lesion.
Conclusion
The final factor structure of the 28-item EVU-PcD scale showed satisfactory reliability and validity results to identify the vulnerability situation of people with motor disabilities after an acquired neurological lesion. Other validation stages are suggested to reach a more in-depth construct.
It is believed that the validated EVU-PcD scale collaborates with other studies and research involving the vulnerability construct of people with motor disabilities after an acquired neurological lesion and in the development of other instruments; in addition to that, its applicability can collaborate in the clinical and care practice for the health care of PwD in the Brazilian Unified Health System.
In the results obtained by the Confirmatory Factor Analysis, the exclusion of items, especially from the “Community” domain, modified the original EVU-PcD scale, meaning that new studies should be carried out using the adjusted EVU-PcD version to verify its factor structure.















