Introduction
Declining birth rates and increased life expectancy are some factors that have led to a demographic transition in the global population. However, the senescence process leaves aging individuals more susceptible to the development or aggravation of chronic health problems. In this sense, studies show that multimorbidity is present in up to 70 % of people aged 65 and over, which is a challenge for public health systems, not only due to the cumulative effect of concurrent diseases, but also to the physical, cognitive, and psychosocial consequences and the loss of quality of life 1.
With the aging process, individuals become more fragile and susceptible to the development of chronic health problems, of which cardiovascular diseases are the leading cause of death worldwide, with systemic arterial hypertension (SAH) being the main risk factor for other diseases. The odds of developing SAH increase proportionally with age, rising from 27 % in patients under 60 to 74 % in those aged 80 and over 2. Evidence from the Framingham Heart Study shows that approximately 60 % of the population develops hypertension by the age of 60, and approximately 65 % of men and 75 % of women develop it by the age of 70 3.
In relation to hypertension and other chronic problems, especially regarding mental health, patients with depression and/or anxiety represent a particularly vulnerable population, as they are at a higher risk of developing SAH. In addition, patients with comorbid hypertension associated with mental health disorders represent a population at a higher risk of mortality related to cardiovascular diseases 4.
Depression, for instance, can significantly worsen the prognosis for stroke, regardless of other risk factors such as hypertension and diabetes. In addition, anxiety and depression pose a 30 % higher risk of heart attack and a 44 % higher risk of stroke, respectively 5. In addition to this data, there is a study conducted in Australia that relates more severe depressive disorders to an increased risk of heart problems such as ventricular arrhythmia and acute myocardial infarction 6.
Evidence indicates that addressing physical comorbidity —especially cardiovascular diseases— may be essential in the management of depression. Furthermore, managing depression in the setting of physical comorbidity may be more acceptable to patients than managing depression in isolation, as several stigmas regarding mental health issues remain 7. A study shows that, in the Brazilian context, psychological complaints are one of the leading causes of demand for care in primary health care (PHC) in Brazil, corroborating its key role in monitoring and diagnosing people with mental disorders 8.
Given the challenges posed by the aging process, it is necessary to investigate care and assistance strategies to provide a better understanding of workers who face such events daily. This raises the question of what scientific evidence is available in the literature regarding mental health care implemented in PHC for elderly hypertensive patients. This review aimed to identify the evidence and systematize the knowledge produced on mental health care for hypertensive elderly people in PHC.
Materials and Methods
This is an integrative literature review, which is a method defined by its capacity to synthesize relevant scientific evidence on a given topic. The following items were rigorously followed: definition of the theme and research question, from which the descriptors and search strategy in the databases were defined; the selection of inclusion and exclusion criteria for studies; identification of the selected studies; categorization; analysis and interpretation of the results and knowledge synthesis, following the guidelines provided by the Joanna Briggs Institute (JBI [9]). The guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Prisma [10]) were also followed, and the study was registered on the International Prospective Register of Systematic Reviews (Prospero) platform, with the registration number CRD42022376277.
The research question “What scientific evidence is available in the literature on mental health care provided in PHC to elderly hypertensive patients?” was prepared using the “PICo” strategy 11, where “P” stands for population (healthcare professionals); “I” stands for intervention (mental healthcare [work process] for elderly hypertensive patients); “Co” stands for context (PHC).
For the level of evidence, the classification of the Oxford Center for Evidence-based Medicine was adopted, which has the following classification: 1A — systematic review of randomized controlled clinical trials; 1B — randomized controlled trial with a narrow confidence interval; 1C — therapeutic results of the “valid or invalid” type; 2A — systematic review of cohort studies; 2B — cohort study; 2C — analysis of therapeutic results or ecological studies; 3A — systematic review of case-control studies; 3B — case-control study; 4 — case reports; 5 — specialist opinion devoid of explicit critical evaluation or based on physiology or basic research 12.
Data Collection
Data collection was performed in January 2023 in the following databases: National Library of Medicine (PubMed), Virtual Health Library (BVS/Bireme), Medical Literature Analysis and Retrieval System Online (Medline), Latin American and Caribbean Health Sciences Literature (Lilacs), Cumulative Index to Nursing and Allied Health Literature (Cinahl), SciVerse Scopus (Scopus), and the American Psychological Association (APA PsycINFO).
After defining the research question, the search strategy was devised with the assistance of a librarian, using controlled descriptors from the Medical Subject Headings (MeSH), Health Sciences Descriptors (DeCS), and Cinahl headings, in addition to using synonyms of the controlled descriptors, combining the descriptors from each set of the PICo strategy with the Boolean OR and AND operators. To cover the peculiarities of each database, the search strategy was devised according to their particularities, and no period or language restriction filters were added. Thus, the search strategy was defined for each database and the respective number of articles was retrieved, totaling 865 articles.
The selected articles were then entered into the Rayyan® reference management tool for organization, where duplicate articles were excluded, resulting in a total of 559 articles (Table 1).
Table 1 Study Search Strategy According to the Databases Found. Brazil, 2023
| Source | Strategy | No. of articles |
|---|---|---|
| PubMed | ((((Aged OR Elderly) OR (“Aged, 80 and over” OR “Oldest Old” OR Nonagenarians OR Nonagenarian OR Octogenarians OR Octogenarian OR Centenarians OR Centenarian)) AND ((Hypertension [MeSH Terms]) OR (Hypertension [Text Word] OR “Blood Pressure, High” [Text Word] OR “Blood Pressures, High”[Text Word] OR “High Blood Pressure” [Text Word] OR “High Blood Pressures” [Text Word]))) AND ((Mental Health[MeSH Terms]) OR (“Mental Health” [Text Word] OR “Health, Mental” [Text Word] OR “Mental Hygiene” [Text Word] OR “Hygiene, Mental” [Text Word]))) AND ((Primary Health Care[MeSH Terms]) OR (“Primary Health Care” OR “Care, Primary Health” OR “Health Care, Primary” OR “Primary Healthcare” OR “Healthcare, Primary” OR “Primary Care” OR “Care, Primary” [MeSH Terms])) | 149 |
| BVS/Medline/ Lilacs | ((aged OR elderly) OR (“Aged, 80 and over” OR “Oldest Old” OR nonagenarians OR nonagenarian OR octogenarians OR octogenarian OR centenarians OR centenarian)) AND (hypertension OR “Blood Pressure, High” OR “Blood Pressures, High” OR “High Blood Pressure” OR “High Blood Pressures”) AND (“Mental Health” OR “Health, Mental” OR “Mental Hygiene” OR “Hygiene, Mental”) AND (“Primary Health Care” OR “Care, Primary Health” OR “Health Care, Primary” OR “Primary Healthcare” OR “Healthcare, Primary” OR “Primary Care” OR “Care, Primary”) | 130 |
| Cinahl | ((Aged OR Elderly) OR (“Aged, 80 and over” OR “Oldest Old” OR Nonagenarians OR Nonagenarian OR Octogenarians OR Octogenarian OR Centenarians OR Centenarian)) AND (Hypertension OR “Blood Pressure, High” OR “Blood Pressures, High” OR “High Blood Pressure” OR “High Blood Pressures”) AND (“Mental Health” OR “Health, Mental” OR “Mental Hygiene” OR “Hygiene, Mental”) AND (“Primary Health Care” OR “Care, Primary Health” OR “Health Care, Primary” OR “Primary Healthcare” OR “Healthcare, Primary” OR “Primary Care” OR “Care, Primary”) | 48 |
| Scopus | ((ALL (aged OR elderly) OR ALL (“Aged, 80 and over” OR “Oldest Old” OR nonagenarians OR nonagenarian OR octogenarians OR octogenarian OR centenarians OR centenarian))) AND (TITLE-ABS-KEY (hypertension OR “Blood Pressure, High” OR “Blood Pressures, High” OR “High Blood Pressure” OR “High Blood Pressures”)) AND (TITLE-ABS-KEY (“Mental Health” OR “Health, Mental” OR “Mental Hygiene” OR “Hygiene, Mental”)) AND (TITLE-ABS-KEY (“Primary Health Care” OR “Care, Primary Health” OR “Health Care, Primary” OR “Primary Healthcare” OR “Healthcare, Primary” OR “Primary Care” OR “Care, Primary”)) | 288 |
| APA PsycINFO | ((Any Field: (“Primary Health Care”) OR Any Field: (“Care, Primary Health”) OR Any Field: (“Health Care, Primary”) OR Any Field: (“Primary Healthcare”) OR Any Field: (“Healthcare, Primary”) OR Any Field: (“Primary Care”) OR Any Field: (“Care, Primary”))) AND ((Any Field: (“Mental Health”) OR Any Field: (“Health, Mental”) OR Any Field: (“Mental Hygiene”) OR Any Field: (“Hygiene, Mental”))) AND ((Any Field: (Hypertension) OR Any Field: (“Blood Pressure, High”) OR Any Field: (“Blood Pressures, High”) OR Any Field: (“High Blood Pressure”) OR Any Field: (“High Blood Pressures”))) AND ((Any Field: (Aged) OR Any Field: (Elderly)) OR (Any Field: (“Aged, 80 and over”) OR Any Field: (“Oldest Old”) OR Any Field: (Nonagenarians) OR Any Field: (Nonagenarian) OR Any Field: (Octogenarians) OR Any Field: (Octogenarian) OR Any Field: (Centenarians) OR Any Field: (Centenarian))) | 250 |
| Total | 865 | |
| Total of duplicate references after Rayyan | 306 | |
| Total after duplicate exclusion | 559 |
Source: Prepared by the authors.
The inclusion and exclusion criteria were also formulated based on the PICo strategy. The inclusion criterion was intervention studies addressing mental health care provided in PHC for elderly hypertensive patients and the exclusion criteria were experience reports, specialist opinion articles, literature reviews, letters, editorials, and other articles that failed to comply with the scope of this review.
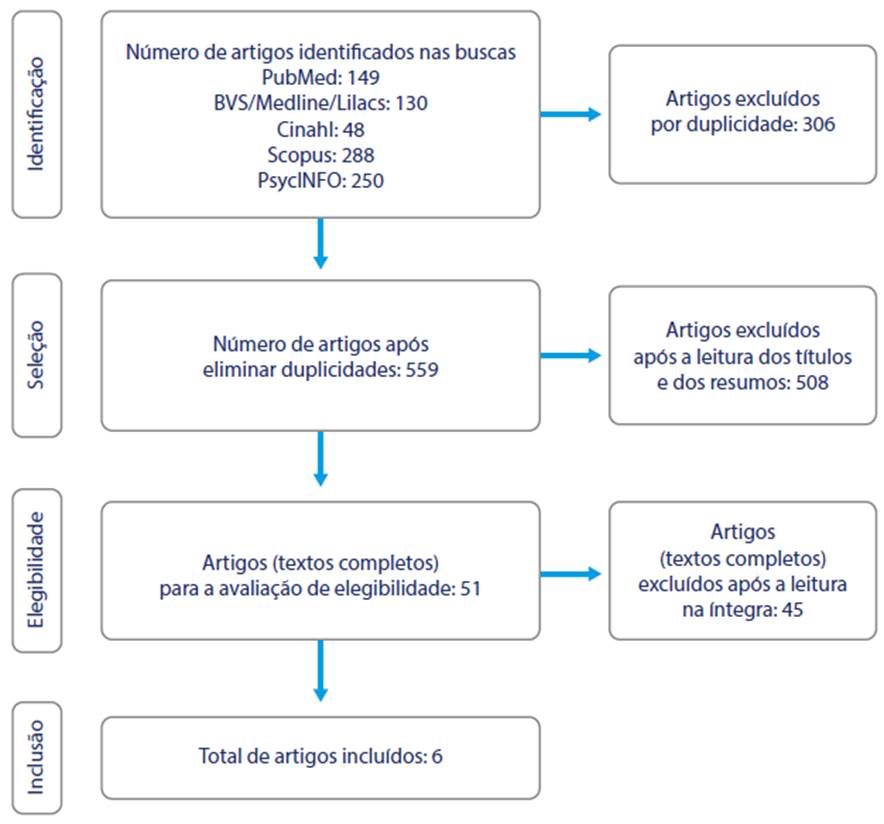
The selection of the studies that composed the sample was carried out by two researchers with experience in the theme, in two stages: a) title and abstract screening, and b) full-text screening. Both stages were carried out independently by the researchers. After the researchers had finished screening each stage, they held meetings to reach a consensus and discuss the inclusion or exclusion of the articles, and in the event of disagreements, a third researcher would be involved, but this was not necessary, as shown in the following flowchart of study selection (Figure 1).
Results
The 559 articles selected were analyzed based on the titles and abstracts to answer the guiding question. The sample was reduced to 51 studies, of which, after reading in full, 45 were excluded because they failed to address the research object (the mental health of hypertensive elderly people), or the authors failed to directly specify aspects of this population, or they only provided prevalence data. Therefore, six studies were included in the final sample of the present review, according to the flowchart adapted from Prisma 10.
For data extraction and study characterization, the instruments proposed by the JBI were used, which discuss the methodological quality of qualitative reviews. Identification data (main author and publication year), study context (country), and methodological aspects (study design, objective, sample, and level of evidence) are presented in Table 2 9.
Table 2 Identification of the selected articles. Brazil, 2023
| Author and publication year | Design, sample, and country | Objective | Level of evidence |
|---|---|---|---|
| Forjaz MJ, Rodriguez- Blazquez C, Ayala A, Rodriguez-Rodriguez V, de Pedro-Cuesta J, GarciaGutierrez S, 2015 (1) | Cohort study comprising three studies with 705, 443, and 4995 individuals respectively, aged 65 and over. Spain. | To determine the impact of chronic conditions on multimorbidity, disability, and quality of life. | 2B |
| Bogner HR, de Vries HF, 2008 (7) | Randomized controlled pilot study with 64 individuals aged 50 or over. The United States of America. | To examine whether the integration of depression treatment into hypertension treatment improved adherence to antidepressant and antihypertensive medication, depression outcomes, and blood pressure control in elderly patients in PHC. | 1B |
| Xue J, Conwell Y, Tang W, Bogner HR, Li Y, Jiang Y et al., 2018 (13) | Systematic review of a cohort study with 2362 individuals aged 60 and over. China. | To examine the effect of adherence to treatment on blood pressure control in elderly Chinese people with depression. | 2A |
| Linardakis M, Papadaki A, Smpokos E, Micheli K, Vozikaki M, Philalithis A, 2015 (14) | Descriptive, crosssectional study with 26,026 adults aged 50 and over across 11 countries. Austria, Belgium, Denmark, France, Germany, Greece, Italy, the Netherlands, Spain, Sweden, and Switzerland. | To assess the presence of multiple behavioral risk factors in adults aged 50 and over across 11 European countries, based on physical and mental health status. | 2C |
| Sass A, Gravena AAF, Pilger C, de Freitas Mathias TA, Marcon SS, 2012 (15) | Descriptive study with 100 elderly people aged from 60 to 88. Brazil. | To assess the presence of depressive symptoms in elderly people registered in the Hypertension Control Program in a city in northwestern Paraná. | 2C |
| Li LW, Xue J, Conwell Y, Yang Q, Chen S, 2020 (16) | Qualitative study with 38 participants. China. | To examine how the Depression/ Hypertension in Chinese Older Adults Collaborations in Health (COACH) instrument was implemented to identify the enablers and barriers to its wider implementation. | 2C |
Source: prepared by the authors.
Of the studies included, five 1,3,8-10 were published in international journals and one 11 in a national journal. Regarding the publication year, the studies included were published between 2008 and 2020, with the decade of 2010 representing the highest percentage of publications, with a total of four 1,8,10,11, followed by the decades of 2000 3, and 2020 9, as shown in Table 2.
Regarding research locations, Table 2 shows that the studies are global in scope, with two from China 8,9; one from Brazil 11; one from the United States 3; and two from Europe 1,10, one of which covered 11 European countries. Regarding language, five 1,3,8-10 of the publications were in English and one 11 was in Portuguese. In terms of content, based on the reading and organization of the information from the selected studies, it was possible to group the axes of care into two thematic categories: “Integrated care” and “Health-related quality of life”, as shown in Table 3.
Table 3 Categorization of the Care Highlighted in the Selected Articles. Brazil, 2023
| Categories | Care highlighted |
|---|---|
| Integrated care between the various members of the healthcare team | Integrated care management program (1). Care manager proposal (7). Bond between the team and the community through a professional present in the region with a closer bond (13, 16). Shared action and knowledge among the various healthcare professionals involved and teamwork (15). Proposal for a multidisciplinary team, promoting comprehensive care in the management of care (1, 15). |
| Health-related quality of life | Prevention programs focused on reducing the prevalence of behavioral risk factors, such as physical inactivity (14). Interventions designed to change inadequate nutritional status (15). Integrated care that includes measures to improve sleep patterns (15). Community groups used as a strategy for screening and identifying possible symptoms in the general population, enabling early measures to be taken (15). |
Source: Prepared by the authors.
Discussion
Based on the results, it was possible to identify different types of healthcare services aimed at improving the mental health of elderly hypertensive patients in PHC. The literature evidenced and emphasized that care provided by an interdisciplinary team is the adequate approach to address the challenge of a growing elderly population, i.e., shared and networked care is emphasized in the literature.
Integrated care between the various professionals working in healthcare teams improves the quality of care, quality of life, patient satisfaction, and system efficiency for patients with complex conditions 17.
The strategies for implementing this type of care varied in the studies presented, but all had a common objective: to share the knowledge of the various healthcare professionals involved in the work processes, in addition to strengthening the relationship between the patient and the healthcare team 1,7,13,15,16.
A study carried out in the United States demonstrated the unique role played by the integrated care manager, since this is the healthcare professional who mediates or establishes the link between medical doctors and the depressed elderly person with hypertension, helping them to recognize depression in the context of hypertension, providing them treatment recommendations based on guidelines, monitoring adherence to treatment and clinical status, which defines adequate follow-up 7.
The pillars of this integrated care intervention were providing an individualized program consistent with the patient’s social and cultural context, and integrating the depression treatment with hypertension control 7.
This type of intervention is related to the Brazilian context and can be compared to the role of nurses in PHC. The role of PHC nurses in Brazil has been developed based on the proposal for a care model based on the principles of the Unified Health System (SUS), which in turn is based on comprehensive care, intervention against risk factors, disease prevention, and health promotion 18.
The Brazilian Ministry of Health proposes that PHC should be the cornerstone for organizing the healthcare system and that the family health strategy should be a priority for promoting changes in health practices. For nursing, the family health strategy is a possibility to reorient its efforts toward the health needs of users, thus advancing towards its specific purpose, namely nursing care 19.
In rural China, studies have found an intervention named “Coach” 13,16. This intervention consists of establishing a care team composed of a village doctor (VD), an aging worker (AW) in each village and a consultant psychiatrist at the regional or county psychiatric hospital. The AWs are employees of the village committee, which is the body that governs local public affairs. One of their official duties is to implement family life education or to help older villagers participate in community life, which suits them well since, as residents, the AWs know the villagers well 13,16.
Coach’s core elements include a VD trained to screen and monitor blood pressure and depressive symptoms and use evidence-based guidelines and practices for the management of hypertension and depression; an AW trained to carry out systematic assessments of social stressors suffered by patients and provide support through home visits, educating patients and their families, as well as promoting adherence to treatment and the adoption of healthy behaviors by patients. The Coach intervention required VDs, AWs, and psychiatrists to work as a team, which showed that Coach participants experienced significantly greater improvements in depression and better blood pressure control 13,16.
The Coach strategy can be applied to Brazilian PHC practically in its entirety, mirroring the work of community health agents in the practice of AWs, whose duties can be summarized as activities that connect the healthcare team with the community, identifying risk situations and guiding the community 20.
The relationship between VDs and psychiatrists is also mirrored in the relationship between PHC medical doctors and nurses and the family health support centers (FHSC), which are multi-professional teams whose work aims to broaden the scope and reach of PHC measures, aiming to increase resolubility at this level of care 21.
The FHSC has an important role in Brazil, both in expanding access to healthcare measures and services, and in improving the quality of care, the integrality of care, and the resolubility of PHC. However, the way organizations have been structured, without promoting the interdisciplinary and communication model, demands co-management so that the obstacles are known, analyzed and, where possible, removed or mitigated. Co-management is also necessary among professionals, in the sense that they accept their responsibilities among the teams and under the guidance of the local manager, through constant development processes 21,22.
In Europe and Brazil, measures have been discussed in the SUS, with a focus on promoting comprehensive care, including medical doctors, mental health professionals, nurses, and other team members, and are the foundation of comprehensive care management programs 1,15.
In this context, considering that the organization of the care system for elderly patients with chronic illnesses —especially illnesses that affect the emotional and psychological aspects, such as depression— must be based on practice and shared knowledge of the various healthcare professionals involved in the work process 1,15, and expressed in the co-participation between patients and professionals who are adequately trained to recognize depressive symptoms and thus ensure that the elderly remain part of society, once again referring back to the role of FHSC and especially to continued health education —a key strategy for the transformation of work in health care so that it becomes a space for competent, committed, critical, and reflective action. Permanent health education is proposed as a response to the challenge of ensuring that the health sector meets the needs of the population, encourages adherence among workers, and establishes living processes of participatory and transformative management 23.
In Europe, a sample study discussed how sufficient levels of physical activity have generally been found to be a protective factor against the development of chronic diseases and can also protect mental health by reducing anxiety or depression. The study also showed that significant associations exist between unhealthy lifestyle behaviors and overall physical and mental health problems; thus, PHC programs should focus on identifying ways to reduce behavioral risk factors (BRFs), noting that interventions should be based on the healthcare systems of each country 14.
Such interventions can be applied at the community or home level in PHC and should include patients and healthcare professionals at all stages of development and implementation to increase the prospects of effectiveness. These programs should focus on adults with multiple BRFs and offer them individualized care and guidance according to personal motivations, abilities, and limitations for lifestyle changes, as well as supporting the use of health promotion and screening services to reduce BRFs 14.
This concern can also be noticed in Brazil, where in 2006, with the approval of the National Health Promotion Policy, the commitment to initiatives that promote physically active lifestyles was emphasized. This context led to the inclusion of physical education professionals in PHC, especially in the FHSC and in projects aligned with health promotion, protection, and rehabilitation policies. Thus, the participation of these professionals in PHC is one of the strategies to increase the practice of physical activity in the population and mitigate the risks of sedentary lifestyles in Brazil 24.
The operational groups available at the PHC also provide healthier living conditions by encouraging the practice of physical activities and stretching exercises, within the context of health promotion. Such practices favor physical improvement, self-esteem and self-image, reduce depression, and improve physical readiness for daily routine activities, even if the unit does not necessarily have the support of a physical education professional, as one study has shown 25.
Still, considering health-related quality of life, the Brazilian sample study found the incidence of depressive symptoms in patients with inadequate nutritional habits, combined with the knowledge that depression can lead to obesity due to changes in eating habits and patterns of physical inactivity and that obesity can lead to depression due to negative body image, in addition to the fact that both obesity and underweight are associated with depression, even after controlling for various sociodemographic variables. It is therefore necessary to prevent depression stemming from nutritional disorders through interventions aimed at changing the nutritional status of this population. It should also be noted that obese people are significantly more susceptible to becoming depressed when compared to underweight individuals 15.
Food and nutrition measures were established in Brazil in 1999 with the creation of the National Food and Nutrition Policy. Since its update in 2011, it has been dedicated to improving the food, nutrition, and health conditions of the Brazilian population through the promotion of adequate eating practices, through food and nutrition surveillance (FNS), in addition to the prevention and comprehensive care of diseases related to food and nutrition. It is the role of the FNS for PHC professionals to assess the nutritional status of their population and, based on the data, mobilize initiatives to prevent and control the main food and nutrition-related diseases in their areas 26.
Another aspect present in the Brazilian study sample is related to depressive symptoms, which increase the difficulty of falling asleep — due to levels of worry, stemming from factors such as increased susceptibility to health problems, financial difficulties, and emotional and social losses, for instance. These factors inherent to the elderly population increase the need for integrated care targeting these depressive aspects 15,27.
Sleep has a significant impact on health, and robust evidence shows that poor-quality sleep triggers a series of inflammatory and metabolic processes. In addition, the presence of common mental disorders has been found to increase the prevalence of poor sleep quality by 61 %. These disorders consist mainly of symptoms of depression or anxiety, and the literature has shown an association between depression, dissatisfaction with life, and impaired sleep 28. A meta-analysis that included 21 longitudinal studies confirms insomnia as a risk factor for depression 27.
It is therefore vital to monitor sleep patterns to identify the most vulnerable populations, such as the elderly, and to identify the most effective strategies to control and treat disorders along with initiatives to promote healthy sleep 28. In this context, PHC once again stands out as the best alternative, due to its emphasis on health promotion and preventive measures, as well as more effective surveillance due to the increased possibility of access by the community.
Finally, this study also reflects on the social groups run in PHC, which are strategies that can improve the early screening of possible depressive symptoms in the general population, contributing to their identification and supporting a more individualized approach aimed at promoting health for the elderly 15.
Studies have shown the potential of this strategy in PHC, such as the study that explored the perceptions of the elderly regarding social groups 29, showing benefits such as the establishment of relationships, the expression of feelings, the creation of a bond with the healthcare service, and an improvement in well-being. It demonstrated the importance of PHC as a socializing space, a place for listening, developing skills, improving relationships, establishing bonds, and an instrument for health promotion and managing aspects of mental health 29.
The plurality of aspects raised by the various articles included in the sample shows that mental healthcare for hypertensive elderly people in PHC must consider a series of principles and strategies to consolidate it.
Conclusions
The strategies used to provide mental health care for hypertensive elderly people raised in the study, including international ones, have been widely discussed in the Brazilian healthcare system, such as comprehensive care, multidisciplinarity, and the focus on promoting health and quality of life. Sharing knowledge and continued health education permeated the articles and proved to be key points for effective mental healthcare for hypertensive elderly people.
These care strategies still face some obstacles due to the lack of incentives to improve care in networks, as well as the lack of investment in professional training. However, this study highlights the importance of consolidating this form of care, which is provided in PHC and has outcomes at all levels of care.
Study limitations
The results of this review should be interpreted in the light of its limitations. The sample included studies performed worldwide, which demonstrates a wide search, but the challenges identified in certain countries may not apply to other countries due to differences in culture, beliefs, and healthcare systems. In addition, another limitation is the lack of studies highlighting the mental healthcare provided to elderly people with hypertension. However, this does not invalidate our findings, since our search included multidisciplinary databases that are acknowledged and used worldwide. Furthermore, to carry out this study, we sought to carry out a systematic and rigorous approach to the integrative review processes, especially data analysis, which implies a reduction in biases and errors.