Migration is defined as the process by which people move from one society to another with the intention of settling there (Giddens, 2006). In recent decades, South American populations have moved within the context of international migration processes, motivated by labor as well as social, political, and economic factors (Machín, 2011; Organización Mundial para las Migraciones, 2012; Pellegrino, 2003; Villa & Martínez, 2000).
However, to this type of migration must be added the migration of people who have also migrated massively from rural areas in the Highlands of the Andes to cities on the coast. In particular, Aymara individuals are composed of around two million people and have systematically migrated during the last decades (Gundermann, 2000; Köster, 1992; Núñez & Cornejo, 2012; Van Kessel, 1996a; Zapata, 2007).
Cultural, social and economic changes that this population has had to cope with often conflicts with the concept of balance and harmony of the Andean worldview. For the Aymara population, the world is ordered based on three dimensions: social relationships, relationships with "divinities," and relationships with nature. These three dimensions are closely related and Aymara understanding of the universe is based on the cyclical rhythms of nature and the ritual calendar that they adapted to these natural rhythms. (De Munter, 2010; Van Kessel, 1996b). Thus, Aymara behavior relies on the community experience that conflicts with the Western culture built on individualism and personal achievement. These intercultural dynamics have led to an identity crisis among the Aymara migrant group. Consequently, a large number of people who could be identified as Aymara by heritage or because of the use of Aymara traditions, no longer identify themselves as belonging to this ethnic group (Zapata, 2007). Actually, there is a growing body of literature interested in migration consequences on health, especially in the field of mental disorders (Patel et al., 2017). Especially, migration confers an increased risk for schizophrenia and there is an increasing interest in assessing this extremely vulnerable population (Selten, Cantor-Graae, & Kahn, 2007).
Schizophrenia, in addition to the clinical symptoms characteristic of the disorder, implies an important economic and social cost for the sufferer and their relatives, as well as a high degree of stigmatization that severely affects their quality of life (QoL) (De Toledo & Blay, 2004). Considering this, it has become necessary to contemplate the QoL as part of the evaluation of the results of the treatment administered to patients with schizophrenia (Cavieres & Valdebenito, 2005).
QoL has an essentially subjective nature, and there are a number of factors associated with this construct, including physical and emotional health, psychological and social well-being, fulfillment of personal expectations and goals, economic security, and functional capacity to develop in a standardized way the activities of daily living (Awad & Voruganti, 2008; Bobes & González, 2000; Pinikahana, Hapell, Hope, & Keks, 2002).
Patients with schizophrenia disorder have a significantly poorer standard of living than others in their community (Pinikahana et al., 2002). A number of factors negatively influence their quality of life, such as: being a man (Browne et al., 1996; Caron, Mercier, Diaz, & Martin, 2005); older (Browne et al., 1996); unemployed (Hofer et al., 2004); without a partner (Salokangas, Honkonen, Stengard, & Koivisto, 2001); with a higher number of hospitalizations (Browne et al., 1996); with low social support (Górna, Jaracz, Rybakowski, & Rybakowski, 2008); with a higher disorder severity (Rudnick, 2001); and with greater medication side effects (Awad & Hogan, 1994; Bobes, Garcia-Portilla, Bascaran, Saiz, & Bousono, 2007).
Studies lacks on the extent to which cultural factors among ethnic minorities are related to QoL (Boyer et al., 2013; Gray, Rofail, Allen & Newey, 2005; McCrone et al., 2001; Ruggeri et al., 1994; Ruiz, 1998; Zendjidjian et al., 2014). Patients with mental disorders belonging to an ethnic minority experience a double stigma: stigma attributable to illness and the one attributable to their lower socioeconomic status. Ethnic minority patients also tend to be less aware of community resources, possess less social support, face language difficulties (Kung, 2003), and are more likely to discontinue mental health treatment (Haas et al., 2008; McLafferty, 1982; Rice, 1987; Smith et al., 2007; Thompson, Carrasquill, Gameroff & Weissman, 2010; Vicente, Kohn, Rioseco, Saldivia & Torres, 2005; Williams & Collins, 2001).
The understanding of the QoL of ethnic minority patients should therefore lead to improved strategies to lower the treatment discontinuation rates (Vicente et al., 2005) and improve functional outcomes (Caqueo-Urízar et al., 2016).
This study aims to describe the QoL of outpatients with schizophrenia belonging to an Aymara ethnic group in the Andean region in Latin-America and compare that population with Non-Aymara patients receiving treatment in the same mental health system. Because this culture presents a different worldview from the Western culture and due to the disadvantages that ethnic minority patients face, we hypothesize that Aymara patients will have a lower QoL than Non-Aymara patients.
This study is based on a secondary analysis of a broader research whose main objective was addressed in a previous publication (Caqueo-Urízar, Breslau, & Gilman, 2015).
Method and materials
Study participants
The study sample included patients with schizophrenia who were receiving services from three mental health clinics in the Central-Southern Andean regions of northern Chile (Arica), southern Peru (Tacna), and central-western Bolivia (La Paz). The sample included both Aymara and Non-Aymara patients. Both Aymara and Non-Aymara patients live in the same urban areas, are served by the same mental health centers, and have roughly comparable socio-demographic characteristics, but the Aymara speak both Spanish and Aymara.
Recruitment of Aymara and Non-Aymara patients took place in three public health sector clinics in Peru, Chile, and Bolivia. We selected the largest public health clinic in each region. The first author reviewed the lists of patients who were attending each center in each country and the research team made assessments over a three-month period in each country. Aymara patients were identified by Aymara surnames as established by legislation regarding indigenous peoples in the three countries, or by Aymara self-identification. Patients were invited to participate as they came to their monthly follow-up visits. Most of the people agreed to participate.
We applied a small set of exclusion criteria to the patient groups to ensure ability to participate fully in the interviews. We excluded those in a state of psychotic crisis or having a sensory or cognitive type of disorder preventing evaluation. The final sample included 253 patients with an ICD-10 diagnosis of schizophrenia (World Health Organization [WHO], 1992), (33.6% from Chile, 33.6% from Peru, and 32.8% from Bolivia). In relation to each specific institution in this study, the three clinics shared similar characteristics in terms of size, type of treatment given to patients, professionals, and free access of care.
Interview Procedures
The study was approved by the Ethics Committee of the University of Tarapacá and the National Health Service of Chile. Two psychologists, who were part of the research team and supervised by the main researcher, conducted the patients’ evaluations under the auspices of the mental health services of each of the three countries. They evaluated the patients during 30 to 45 minutes.
Before the start of the survey, we requested and received informed consent from the patient. We explained the objectives of the study as well as the voluntary nature of participation. We offered no compensation for study participation.
Measures
Schizophrenia Quality of Life Questionnaire (S-QoL18) (Boyer et al., 2010): The S-QoL18 is a self-administered QoL questionnaire designed for people with schizophrenia that has been used extensively in Europe (Auquier et al., 2013; Baumstarck et al., 2013; Boyer et al., 2013). It has been adapted to the Spanish in Latin American countries, with α = ≥0.7 for the Total Index of QoL. Also the subscales present satisfactory Cronbach’s alpha (the reader can review the published study Caqueo-Urízar et al., 2014).
The aforementioned questionnaire is a multidimensional instrument that assesses the patient’s view of his or her current QoL. It is made of 18 items describing 8 dimensions: psychological well-being (PsW), self-esteem (SE), family relationships (RFa), relationships with friends (RFr), resilience (RE), physical well-being (PhW), autonomy (AU), and sentimental life (SL), as well as a total score (Index). Dimensions and Index scores range from 0, indicating the lowest QoL, to 100, the highest QoL.
Positive and Negative Syndrome scale for Schizophrenia (PANSS) (Kay, Fiszbein, & Opler, 1987) This is a 30-item, rating scale administered to clinicians that is developed to assess psychotic symptoms in individuals with schizophrenia and which comprises 5 different subscales: positive, negative, cognitive, depressive, and excitement scales (Fresán et al., 2005). The PANSS was translated and validated in Spain by Peralta and Cuesta (1994) and in Mexico by Fresán et al. (2005). In this study, we focused on the PANSS total score (α = 0.93), which provides a general measure of the severity of the disorder.
Drug Attitude Inventory (DAI-10) (Hogan, Awad, & Eastwood, 1983) This 10-item patient self-report scale was developed to assess attitudes, experiences, and beliefs about antipsychotic drugs. The DAI-10 is considered to be a good predictor of adherence to treatment in schizophrenia (Hogan et al., 1983; Nielsen, Lindström, Nielsen, & Levander, 2012). Scores ranged from -10 (very poor attitude) to +10 (best possible attitude). It has been adapted to Spanish by Robles García, Salazar Alvarado, Páez Agraz and Ramírez Barreto in 2004. The Cronbach's alpha coefficient of the DAI in this study was α = 0.7.
Demographic and clinical characteristics: Participant demographic characteristics included sex, age, ethnicity (Aymara and Non-Aymara), educational level (low or high), marital status (with a partner or without a partner), employment status, and family income (measure of the total salary per month for all members of the family, expressed in US dollars). Clinical characteristics covered information about duration of the disorder, number of hospitalizations, and type of treatment.
Data analysis
Data were expressed as proportions or as the means with standard deviations. The data were assessed for normal distribution using the Shapiro-Wilk test and for homogeneity of variance with the Levene test. Comparative analyses were performed to assess differences between Aymara and Non-Aymara (i.e. origin profiles) patients. Associations between patients’ origin and the qualitative variables (gender, marital status, educational level, employment status, and type of mental health treatment) were analyzed using Chi-Square tests; associations between patients’ origin and the quantitative variables (age, monthly family income, duration of disorder, number of hospitalizations, PANSS total score, S-QoL18 Index and its 8 dimensions) were calculated using Student t-tests for normally distributed data or using non-parametric Mann Whitney tests in case of non-normal distributions.
Multivariate analyses using multiple linear regressions (simultaneous model) were then performed to confirm the link between ethnicity and QoL levels. The S-QoL18 index and each of its 8 dimensions were considered as separate dependent variables. The variables relevant to the models were selected from the comparative analyses, based on a threshold p-value ≤0.2. The final models incorporated the standardized β coefficients, which represent a change in the standard deviation of the dependent variable (QoL) resulting from a one-standard-deviation change in the various independent variables. The independent variables with the higher standardized β coefficients are those with a greater relative effect on QoL.
This study was a confirmatory analysis. The hypothesis was that belonging to an ethnic group (i.e. Aymara vs Non-Aymara) was associated with QoL of schizophrenic patients, based on the results of previous analyses (Caqueo-Urízar et al., 2017a). In this last research, the aim of the study was thus to determine whether caregivers’ QoL is a determinant of patients’ QoL, while considering other important determinants such as sociodemographic and clinical characteristics.
In our study, no correction for multiple testing has been carried out, consistent with recommendations (Bender & Lange, 2001).
Findings
Sample characteristics
Two hundred and fifty-three patients with schizophrenia were enrolled in the present study. The mean age of patients was 35.6 years (SD=12.5), 164 patients (66.4%) were men and 117 patients (46.2%) were Aymara. The patients had moderately severe symptoms with a total PANSS score of 71.3 (SD=28.2). Description of the total sample characteristics are reported in Table 1.
Comparisons between Aymara and Non-Aymara patients
The differences between Aymara and Non-Aymara patients are presented in Table 1. Concerning socioeconomic characteristics, monthly family income level (US dollar) was significantly lower for Aymara patients (M=329.5, SD=277.4) than for Non-Aymara patients (M=490.2, SD=512.4), U=4352, p=0.001. Other sociodemographic characteristics were similar.
For clinical factors, Aymara patients had a significantly shorter duration of disorder (M=12, SD=9.7) compared to Non-Aymara patients (M=16.7, SD=12.9), t(240)=3.3, p=0.001. As expected, Aymara patients reported poor QoL, compared to Non-Aymara patients: Aymara patients had significantly lower QoL scores (M=52.3, SD=14.2) than Non-Aymara patients (M=56, SD=14.5) for the total QoL score (S-QoL18 Index), t(250)=2.04, p=0.042, and both for the Family relationships (RFa) dimension (M=59.8, SD=25.5 for Aymara vs M=66.2, SD=20.8 for Non-Aymara), U=6895.5 p=0.031 and for the Sentimental Life (SL) dimension (M=40.4, SD=27.1 for Aymara vs M=49.4, SD=27.4 for Non-Aymara), t(250)=2.6 p=0.01.
In the multivariate analyses (Table 2), the relationships between ethnicity and QoL remained significant even after adjusting for other confounders (including age, location, monthly family income, duration of disorder, DAI-10, and PANSS negative), for the RFa and SL dimensions (β=-0.213, p=0.003 and β=-0.175, p=0.012, respectively). The association between ethnicity and the relationships with friends (RFr) dimension became significant (β=-0.179, p=0.012). A trend was observed for the S-QoL18 Index (β=-0.117, p=0.089).
TABLE 1 Quality of Life of Aymara and Non-Aymara patients
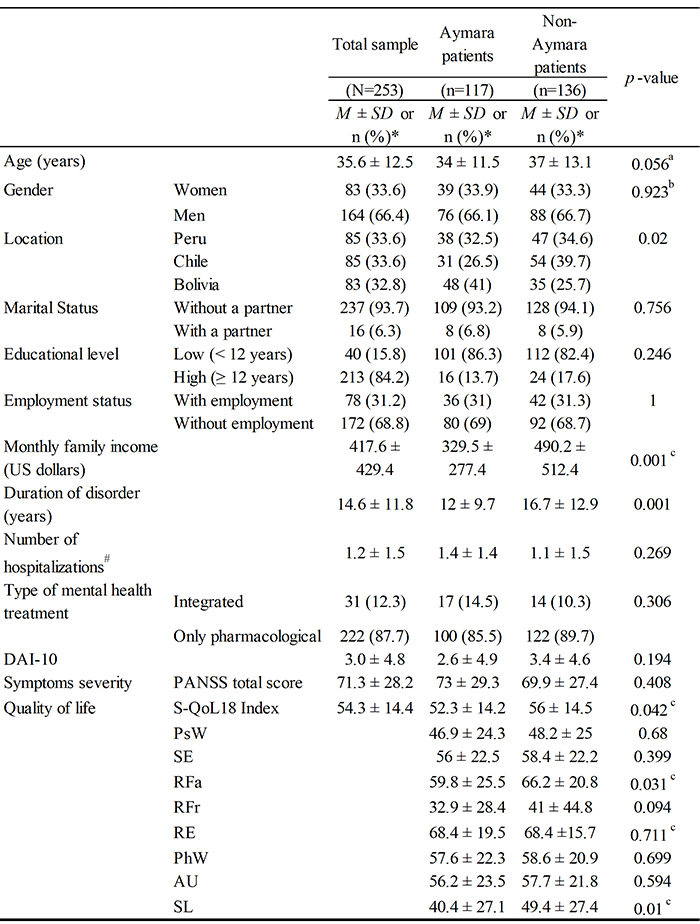
*M ± SD: mean ± standard desviation, n (%): number (percentage).
aStudent T test.
bChi-square test.
cMann-Whitney test
Significant results are in bold. at significance level p<0.05.
#(Since the last 3 years before present hospitalization)
DAI-10:Drug Attitude Inventory.
PANSS:Positive and Negative Syndrome Scale for Schizophrenia, total score and dimensions.
S-QoL18:Schizophrenia Quality of Life questionnaire: PsW: psychological well-being; SE: self esteem; RFa: family relationships; RFr: relationships with friends; RE: resilience; PhW: physical well-being; AU: autonomy; SL: sentimental life.
Source: own work.
TABLE 2 Multivariate analysis. Factors associated with S-QoL18 index and dimensions
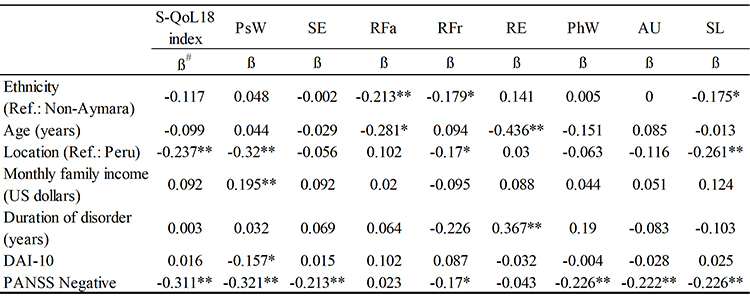
#β: standardised beta coefficient (β represents the change of the standard deviation in QoL score resulting from a change of one standard deviation in the independent variable); Significant results in bold.
*p≤0.05.
**p≤0.01.
S-QoL:Schizophrenia Quality of Life questionnaire; PsW: psychological well-being; SE: self-esteem; RFa: family relationships: RFr: relationships with friends; RE: resilience; PhW: physical well-being; Au: autonomy; SL: sentimental life.
DAI-10:Drug Attitude Inventory.
PANSS:Positive and Negative Syndrome scale of Schizophrenia.
Source: own work.
Discussion
The aim of our study was to describe the QoL of outpatients with schizophrenia belonging to an Aymara ethnic group in the Andean region in Latin-America and compare that population to Non-Aymara patients. Our results supported the hypothesis that Aymara patients had a significantly lower level of QoL than Non-Aymara patients, especially for relationships dimensions: family relationships (RFa), relationships with friends (RFr) and sentimental life (SL) QoL dimensions, even after adjusting the model for confounders. These results were consistent with literature. Indeed, previous studies reported Aymara patients to cope with psychological distress, showing the importance of subjective aspects of quality of life among this population (Caqueo-Urízar, Boyer, & Gilman, 2017b). Research from multiple societies revealed that ethnic minorities tend to be exposed to discrimination, these stressful experiences adversely affecting physical and mental health (Haas et al., 2008; Kung, 2003; Smith et al., 2007; Thompson et al., 2010; Vicente et al., 2005; Williams & Collins, 2001). For the poor RFa scores found in Aymara patients, the mass migration phenomenon and the rapid abandonment of rural settlements in the Andean foothills might have affected the family dynamics, being perhaps one of the most difficult experiences for the Aymara patients. Often the family members are separated; the elderly remain in the Highlands while other members move to the nearest towns. Some young people even migrate to the city without their parents, to continue their education. Migration is a complex phenomenon that does not necessarily involve a departure without return, as evidenced by the number of simultaneous residencies and linkages that are maintained with the native communities (Gundermann, González, & Vergara, 2007). Still, in this adaptation process, Aymara families have abandoned, to some extent, traditional cultural patterns and are slowly adopting new and increasingly intercultural lifestyles (Gavilán et al., 2006; Zapata, 2007). These intercultural dynamics may be associated with distance from relatives who stayed in rural Highlands, and might affect their QoL at family level. Furthermore, altered QoL in the family relationships dimension could also be related to higher levels of perceived burden and impaired QoL of Aymara caregivers, as reported in previous studies (Caqueo-Urízar et al., 2012). This could be partially due to scarcity of national social welfare and community rehabilitation programs for relatives of psychiatric patients in these countries (Caqueo-Urízar & Gutiérrez-Maldonado, 2006; Caqueo-Urízar et al., 2014). Families may have become a substitute when facing the scarcity of therapeutic, occupational, and residential resources. The impact of this shift on the family is high, having both an emotional and economic toll (Caqueo-Urízar et al., 2017c). These results highlight the need to better considerate the key role of family relationships in the patients’ care and well-being.
Concerning relationships with friends and sentimental life, Aymara patients reported lower QoL scores in SL dimension than Non-Ayamara patients did. This result should be considered knowing the fact that our total sample of patients with schizophrenia was in its majority alone and without any partner, as described before (Arsova & Barsova, 2016; Chou, Yang, Ma, Teng, & Cheng, 2015). However, previous studies reported that patients who do not have a partner tend to have a lower quality of life (Salokangas et al., 2001). In this case, it may be even harder for Aymara patients to get a partner and social life because of the double stigma that they experienced in discriminations, based both on their Andes phenotype and on their mental disorder (Kirberg, 2006; Urzúa, Heredia, & Caqueo-Urízar, 2016). Furthermore, family support and social support were reported to improve the ability for personal and social contacts of patients with schizophrenia (Arsova & Barsova, 2016).
Another finding shows that socio-demographic variables also have an important role, and socio-economic circumstances should be taken into account when assessing these patients. In this study, monthly family income level was significantly lower for Aymara patients than for Non-Aymara patients. These results are also consistent with previous studies indicating that a higher level of education facilitates employment, thus improving patients’ level of income and QoL (Browne & Courtney, 2005; Marwaha & Johnson, 2004; Ruggeri et al., 2005; Schomerus et al., 2007). Indeed, growing international evidence shows that mental illness and poverty interact in a negative cycle: “poverty breeds ill health and ill health keeps poor people poor” (Wagstaff, 2002, p 97). On the contrary, a recent systematic review described that mental health interventions were associated with improved economic outcomes in low-income and middle-income countries (Lund et al., 2011). Moreover, poverty worsens the health of patients with schizophrenia, and increases the burden of their caregivers (Butzlaff & Hooley, 1998; Caqueo-Urízar & Gutiérrez, 2006; Karanci, 1995), thus leading to poor QoL scores (Caqueo-Urízar et al., 2017a). This reinforces the need for comprehensive care and special attention should be paid to both objective and subjective quality of life indicators (Boyer et al., 2014).
In relation to clinical variables, these findings show that Aymara patients had a significantly shorter duration of disorder than Non-Aymara patients. The underlining assumption of this result should be taken cautiously as it could be explained by a delay in the clinical diagnosis in Aymara patients due to specific cultural beliefs. Indeed, traditionally, the Aymara family tends to first lead the patient to the healer of the community (Yatiri), who performs a series of rituals to cure the mental disorder (Leiva, 2008). However, after a period of time without major improvement, they finally decide to rely on public mental health services. Another explanation could be that Aymara patients tended to be slightly younger than Non-Aymara patients in our sample, even if comparative results were not statistically significant.
It should also be considered that ethnic minority patients tend to be less aware of community resources, possess less social support, and face language difficulties (Kung, 2003), delaying the start of the treatment.
This study had some limitations that should be noted.
First, we cannot extrapolate our findings to the whole Aymara population, and especially not to those Aymara people for whom the problem of access to care is the main problem. Many of these individuals still reside in the rural Highlands. However, our sample of Aymara patients is likely to be representative of the Aymara patients with schizophrenia in our countries, because most Aymara go to public health services and not to private physicians.
Second, our study used only one type of QoL instrument using S-QoL18. It would be interesting to determine whether our findings could be replicated with QoL instruments that use other conceptual models and dimensional constructs.
Third, this study used cross-sectional data, thus relationships between ethnicity and the different variables, including QoL scores, were not addressed according to time and were not supported to be causal. Further investigations with longitudinal studies are needed in the future.
In conclusion, our study found that Aymara patients have lower QoL than Non-Aymara patients and some of the reasons that may explain this result are the migration process experienced by the families, as well as socio-cultural and economic factors.















