Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombia Médica
On-line version ISSN 1657-9534
Colomb. Med. vol.42 no.4 Cali Oct./Dez. 2011
Pregnancy and health-related quality of life: A cross sectional study
Embarazo y calidad de vida relacionada con la salud: Estudio transversal
Robinson Ramírez-Vélez, PT, PhD1
1Nutrition Group, Department of Physiological Sciences, Biochemistry, Faculty of Health, Universidad del Valle, Cali, Colombia.
e-mail: robin640@hotmail.com
Received for publication July 13, 2010 Accepted for publication February 28, 2011
SUMMARY
Objective: To evaluate and identify determinants of health related quality of life (HRQoL) during pregnancy.
Methods: In this descriptive exploratory study in sixty-four nulliparous pregnant women, completed the questionnaire: HRQoL (Colombian standard version of the Medical Outcome Study Short-Form Health Survey -SF12v2-), and socio-demographic determinants (i.e., age, place of origin, education, marital status, and occupation) during the second trimester.
Results: Mean age of patients included was 19.1±2.7 years old and gestational age was 17.6 ± 3.4 weeks. The participants reported higher HRQoL scores in the vitality domain (56±11), followed by mental health (5110), and general health (50±11). Moreover, the lowest score was demonstrated in the domains of emotional role (18±5) and physical role (25±4). Having a higher household socioeconomic level was significantly correlated with higher scores in the physical role, general health, social functioning, emotional role, and mental health. Being married or cohabiting was significantly correlated with all the SF-12v2 domains, with the exception of the Bodily pain domain.
Conclusions: While we have included a comprehensive assessment of socioeconomic variables needed to assess and identify the factors determining the HRQoL during pregnancy, further studies are needed that can guide the expectations of women, their health care providers, and public policy.
Keyword: Pregnant women; Health-related quality of life; SF-12; Colombia.
RESUMEN
Objetivo: Evaluar e identificar los factores determinantes de la calidad de vida relacionada con la salud (CVRS) durante el embarazo.
Métodos: Estudio descriptivo exploratorio en 64 gestantes nulíparas. Las participantes completaron el cuestionario de CVRS SF-12v2 (versión colombiana estándar del Medical Outcome Study Short-Form Health Survey-SF12-), y encuesta de factores determinantes sociodemográficos (edad, procedencia, nivel de educación, estado civil y situación laboral) durante el segundo trimestre del embarazo.
Resultados: La edad media de las participantes fue 19.1±2.7 años y la edad gestacional 17.6 ±3.4 semanas. Las puntuaciones más altas de la CVRS se presentaron en los dominios de vitalidad (56±11), seguido de salud mental (51±10) y salud general (50±11). Por otra parte, la puntuación de CVRS más baja fue acusada en los dominios rol emocional (18±5) y rol físico (25±4). Un mayor nivel socioeconómico se correlacionó significativamente con mejor puntuación en el Cuestionario de Salud SF-12v2 en los dominios función física, salud general, función social, rol emocional y salud mental. Estar casada o en unión libre se correlacionó significativamente con todos los dominios del SF-12v2, con excepción del dominio dolor corporal.
Conclusiones: Si bien se ha incluido una evaluación exhaustiva de las variables socioeconómicas necesarias para evaluar e identificar los factores determinantes en la CVRS durante el embarazo, se necesitan más estudios que puedan guiar las expectativas de las mujeres, sus proveedores de atención de salud y políticas públicas.
Palabras claves: Gestantes; Calidad relacionada con la salud de vida; SF-12; Colombia.
Pregnancy is a time of intense physical change, and it is associated with a great deal of emotional upheaval in many women1. Evidence about the health status of women could inform policies related to leave of absence and disability around the time of pregnancy2. Even in normal pregnancies, women experience subtle changes that may alter their ability to carry out their usual roles and may detract from their overall health-related quality of life and it is a period of physical and emotional stress that can have a significant impact on the well-being of an expectant mother3. In addition to the obvious external physical changes that accompany pregnancy, significant increases in mental health problems, including depression and psychosis, occur either during pregnancy or in the immediate postpartum period4.
Physiological changes occurring during pregnancy are likely to contribute to declines in physical health status. While the goal of medical care during pregnancy remains aimed at increasing the likelihood of a favourable maternal and neonatal outcome, consideration should be given to how a woman's life can be affected by factors arising during pregnancy. The concept that health care can be aimed toward both increasing the health-related functional status and lifespan has been advanced by methods that can validly measure an individual's health-related quality of life5. Much less is known about the factors associated with greater declines in HRQoL during pregnancy. Lower income has been associated with poorer health status during pregnancy6. However, HRQoL in other patient populations has been shown to be multi-determined by contributions from demographic, medical, and psychosocial factors7. Hueston et al.1 found a negative correlation between gestational age and multiple physical HRQoL dimensions, supporting the view that physical changes during pregnancy contribute to the declines. Depressed mood during pregnancy has, in a number of studies, also been shown to negatively impact multiple HRQoL domains8,9. Interestingly, other factors such as age, marital status, educational level and occupational status, which are known to be elevated during pregnancy7,10, have yet to be examined in relation to HRQoL in this population. The objective of this study was to evaluate and identify determinants of health-related quality of life (HRQoL) during pregnancy.
METHODS
Participants. Recruitment took place in three Prenatal Hospital Care units in different regions of Cali, Colombia during ten months of 2008 and the first months of 2009. Interested women eligible for the present study were invited to a pre-test, including interview and assessments at the Cañaveralejo Hospital, Siloé Healthcare Center, Meléndez Healthcare Center, and the Biochemistry Laboratory at Universidad del Valle in Cali, Colombia11. Pregnant women were included if they were: nulliparous women who had not participated in a structured exercise program, 16-30 years of age, with live fetus at the routine ultrasound scan and a normal pregnancy and gestational age of 16 to 20 weeks. They were excluded if they had: a history of high blood pressure, chronic medical illnesses (cancer, renal, endocrinology, psychiatric, neurologic, infectious, and cardiovascular diseases), persistent bleeding after week 12 of gestation, poorly controlled thyroid disease, placenta praevia, incompetent cervix, polyhydramnios, oligohydramnios, and history of miscarriage in the last twelve months. The participants who met the inclusion criteria and agreed to participate were contacted to inform them about how the project would be carried out.
Outcome measures. All participants were assessed on the domains of their perceived health-related quality of life. Health-related quality of life was measured by a Colombian standard version of the Medical Outcome Study Short-Form Health Survey [SF-12v2]12. The questionnaire contains 12 questions grouped into eight different health domains: physical functioning, role limitation due to physical problems, bodily pain, general health perception, vitality, social function, role limitation due to emotional problems, mental health and these scales are further clustered into the physical component scale and mental component scale13.
The physical component scale includes scales to measure physical functioning, role limitations due to physical health problems (physical role), bodily pain, and general health. The mental component scale includes scales to measure vitality, social functioning, role limitations due to personal or emotional problems (emotional role), and mental health. Validity studies suggest an advantage of the physical component scale and the mental component scale over individual scales when interpreting health outcomes. Test scores were normalized according to the instructions provided in the SF-12v2 user manual14. Reliability values (Pearson's r) range from 0.89 to 0.94 for the physical component summary and from 0.84 to 0.91 for the mental component summary15,16. The secondary outcomes were measured via a structured validated interview (socio-demographic and determinants data) and a detailed physical examination. The Research Ethics Committee at Universidad del Valle approved this study (Res-022/29-UV). Informed consent was obtained from all participants before data collection began.
Data analysis. The study was performed in conjunction with a controlled, randomized clinical trial, the objective of which was to evaluate the effectiveness of a program of aerobics of moderate intensity for sedentary pregnant women with respect to the outcome of the pregnancy, physical capacity and maternal cardiorespiratory parameters during labor and childbirth. Details on the intervention and the main results of this study are already published elsewhere (Trial registration: NCT00741312)11. For this reason, we chose a sample size of at least 70 pregnant women to ensure that mean utility estimates would have a margin of error not greater than 7% at a 95% confidence interval. Data was entered directly into a customized Microsoft Excel database by an investigator at the time of the interview and baseline testing. Daily backups were performed and transferred to the master database at least once a week. Random checks of data entry were performed regularly and corrections made were possible by checking against paper records or, in rare cases, by phoning participants for confirmation by an independent investigator. An exploratory analysis using the Kolmogorov-Smirnov test was first performed to assess the normality of the score distribution for each variable. Descriptive statistics including means and standard deviations were calculated for all the variables (SF-12v2). A Pearson correlation matrix was computed with all the variables to examine the bivariate correlations between the outcome variables (SF-12v2 domains) and each potential predictor variable. The pattern of intercorrelations among the possible predictor variables was also examined to determine the extent of multi-collinearity among predictors. A series of multiple stepwise linear regression analyses were conducted to identify the independent determinants of each SF-12v2 domain. Demographic (age, marital status, educational level, occupational status) and medical (gestational weeks) factors were considered potential independent variables. Variable selection was based on theoretical relevance, pattern of univariate association with each of the SF-12v2 domain scores and other potential predictor variables, and the assumptions underlying multiple regression analysis. Data was analyzed by using SPSS v.15.0 (SPSS, Inc, Chicago, IL).
RESULTS
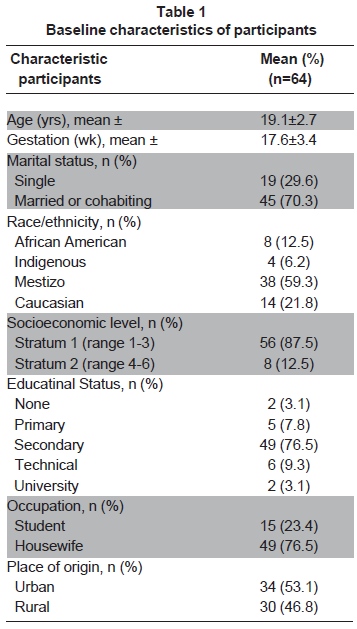
Sixty-four participants were recruited to the study. Mean age of patients included was 19.1±2.7 years old and gestational age at entry was of 17.6±3.4 weeks. Most of the participants (60%) were married or had a cohabiting status and had low socioeconomic levels [(>80% strata 1-2. National Administrative Department of Statistics classification (DANE)]. Ethnic backgrounds, status education, occupation and urban procedence are presented in Table 1.
The results of the scores on the SF-12v2 dimensions obtained in this sample of women during the second trimester of pregnancy are presented in Table 2. The participants reported higher scores in the vitality domain with 56±11, followed by mental health 51±10 and general health 50±11. Moreover, the lowest score was demonstrated in the domains of emotional role 18±5 and the physical role 25±4.
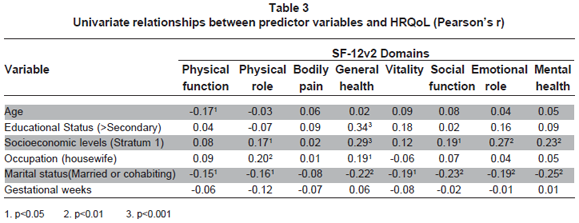
Univariate associations between predictor variables and health-related quality of life was evaluated. Among the demographic variables, the most consistent correlates of the various HRQoL dimensions were socioeconomic level and marital status (Table 3). Having a higher household socioeconomic level was significantly correlated with higher scores on physical role, general health, social functioning, emotional role, and mental health. Being married or cohabiting was significantly correlated with all the SF-12v2 domains, with the exception of bodily pain.
DISCUSSION
The findings from the current research have revealed additional insights into the factors determining HRQoL during early pregnancy. This is the first study to evaluate and identify HRQoL determinants during pregnancy in Colombia. While the pre-pregnancy health status reported by the women in this cohort was similar to or better than normative samples of women of reproductive age, limitations in physical function, restrictions in vitality, and the prevalence of depressive symptoms increased over the course of pregnancy17. For example, the median physical role and emotional role scores observed in our study of pregnant women were similar to other studies involving individuals with mental disease and healthy adult females9,10,15,18,19.
During pregnancy, symptoms are an important contributor to poor health status, while in the postpartum period a lack of social support is the most consistent predictor of poor health outcomes. Other studies have revealed that during pregnancy, symptoms were also an important contributor to poor health status, while during the postpartum period a lack of social support was the most consistent predictor of poor health outcomes1. Although the perception of vitality measuring the degree of energy, pep, or tiredness experienced is classified as a mental health component in the SF-8 and the SF-36, it has a complex construction and is moderately correlated with both mental and physical health functioning. These data suggest that relative stability of the physical and mental component scale of the SF-12v2 and the apparently predictable changes in physical functioning during pregnancy imply that the SF-12v2 can be a useful tool in evaluating functional status.
Previous attempts to improve HRQoL, prenatal or post-natal, in women at risk has taken different forms, such as offering instrumental support to women at risk, providing emotional support, improving social integration, and increasing the number of trusted individuals cannot be easily achieved20. Nevertheless, to be able to find individual solutions for pregnant women at risk, healthcare professionals need to be aware of the importance of socio-demographic factors in maternal well-being and pregnancy outcomes. These results are consistent with an earlier study by Otchet et al.9 who also showed diminished scores along the same SF-36 (standard version) dimensions including physical functioning, role limitation due to physical health, bodily pain, vitality, and social functioning during pregnancy7. Because of the changes associated with gestational age in the physical domains, researchers may wish to adjust the values of the physical domains when pregnant women are included in this study. In addition, the mean scores on physical functioning and bodily pain obtained in our sample of pregnant women were similar to other studies of patients with chronic medical conditions such as cardiovascular disease, diabetes, and cancer7,9, while the means for role limitation due to physical functioning and vitality were even lower compared to these other patient populations.
CONCLUSION
Participants reported higher scores in the vitality domain, followed by mental health and general health. Furthermore, the lowest score was demonstrated in the domains of emotional role and physical role. Having a higher household socioeconomic level was significantly correlated with higher scores on physical role, general health, social functioning, emotional role, and mental health. Being married or cohabiting was significantly correlated with all the SF-12v2 domains, with the exception of bodily pain. In general, these findings must be considered in view of several limitations. As previously mentioned, this study was cross-sectional and, therefore, no cause-effect relationships can be inferred for some of the observed relationships. A further limitation is that most of our sample was affiliated to clinics with low economic levels and; hence, may not be entirely easy to generalize. Future studies across socioeconomic class and various geographical settings are needed to untangle the relative contribution of these factors to HRQoL during pregnancy7. While a comprehensive assessment of socioeconomic variables has been included, the study did not include other potentially important variables such as exercise and pregnancy-related symptoms, which have both been previously shown to influence HRQoL7,11,13,15,21. These data should guide the expectations of women, their health care providers, and public policy.
Support. Universidad del Valle and Nutrition Group (Grant N. CI 1575).
Conflict of interest. None of the author has conflicts of interest related to this study.
ACKNOWLEDGEMENTS
This work was supported by Universidad del Valle (Grant N. CI 1575). Robinson Ramírez-Vélez received a grant from Instituto Colombiano para el Desarrollo de la Ciencia y la Tecnología 'Francisco José de Caldas' to undertake doctoral studies (Convenio Colciencias/Icetex N° 067/2002).
REFERENCIAS
1. Hueston WJ, Kasik-Miller S. Changes in functional health status during normal pregnancy. J Fam Pract. 1998; 47: 209-12. [ Links ]
2. Haas JS, Meneses V, McCormick MC. Outcomes and health status of socially disadvantaged women during pregnancy. J Womens Health Gend Based Med. 1999; 8: 547-53. [ Links ]
3. Haas JS, Jackson RA, Fuentes-Afflick E, Stewart AL, Dean ML, Brawarsky P, Escobar GJ. Changes in the health status of women during and after pregnancy. J Gen Intern Med. 2005; 20: 45-51. [ Links ]
4. Watson JP, Elliot SA, Rugg AJ, Brough DI. Psychiatric disorder in pregnancy and the first postnatal year. Br J Psychiatr. 1984; 144: 453-62. [ Links ]
5. Ramírez-Vélez R. Calidad de vida relacionada con la salud como medida de resultados en salud: Revisión sistemática de la literatura. Rev Colomb Cardiol. 2007; 14: 207-22. [ Links ]
6. Otchet F, Carey MS, Adam L. General health and psychological symptom status in pregnancy and the puerperium: what is normal? Obstet Gynecol. 1999; 94: 935-41. [ Links ]
7. Da Costa D, Dritsa M, Verreault N, Balaa C, Kudzman J, Khalifé S. Sleep problems and depressed mood negatively impact health-related quality of life during pregnancy. Arch Womens Ment Health. 2010; 13: 249-57. [ Links ]
8. Nicholson WK, Setse R, Hill-Briggs F, Cooper LA, Strobino D, Powe NR. Depressive symptoms and health-related quality of life in early pregnancy. Obstet Gynecol. 2006; 107: 798-806. [ Links ]
9. Setse R, Grogan R, Pham L, Cooper LA, Strobino D, Powe NR, Nicholson W. Longitudinal study of depressive symptoms and health-related quality of life during pregnancy and after delivery: the Health Status in Pregnancy (HIP) study. Matern Child Health J. 2009; 13: 577-87. [ Links ]
10. Da Costa D, Dritsa M, Rippen N, Lowensteyn I, Khalifé S. Health-related quality of life in postpartum depressed women. Arch Womens Ment Health. 2006; 9: 95-102. [ Links ]
11. Ramírez-Vélez R, Aguilar AC, Mosquera M, Garcia RG, Reyes LM, López-Jaramillo P. Clinical trial to assess the effect of physical exercise on endothelial function and insulin resistance in pregnant women. Trials. 2009; 10: 104. [ Links ]
12. Ramírez-Vélez R, Agredo-Zuñiga RA, Jerez-Valderrama AM. The reliability of reliminary normative values from the short form health survey (SF-12) questionnaire regarding Colombian adults. Rev Salud Publica. 2010; 12: 807-19. [ Links ]
13. Ramírez-Vélez R. Quality of life and social support for patients suffering from chronic obstructive pulmonary disease. Rev Salud Publica. 2007; 9: 568-75. [ Links ]
14. Ware JE, Kosinksi M. SF-36 Physical & Mental Health Summary Scales: A Manual for Users of Version 1. 2001, 2nd ed. Lincoln RI: QualityMetric. [ Links ]
15. Ramírez-Vélez R, Agredo RA, Jerez AM, Chapal LY. Health-related quality of life and conditions of health in non-institutionalized elderly people in Cali, Colombia. Rev Salud Publica. 2008; 10: 529-36. [ Links ]
16. Bize R, Johnson JA, Plotnikoff RC. Physical activity level and health-related quality of life in the general adult population: a systematic review. Prev Med. 2007; 45: 401-15. [ Links ]
17. Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health. 2003; 12: 373-80. [ Links ]
18. Haas JS, Jackson RA, Fuentes-Afflick E, Stewart AL, Dean ML, Brawarsky P, Escobar GJ. Changes in the health status of women during and after pregnancy. Gen Intern Med. 2005; 20: 45-51. [ Links ]
19. Chang PJ, Wu LY, Chen YC, Chuang CH, Hsieh WS, Lin SJ, Chen PC. Women's perceptions of their husband's drinking behavior as a risk factor of their health-related quality of life in the postpartum period. Qual Life Res. 2010; 19: 47-53. [ Links ]
20. Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, Klapp BF, Arck PC. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod. 2007; 22: 869-77. [ Links ]
21. Lacasse A, Rey E, Ferreira E, Morin C, Bérard A. Nausea and vomiting of pregnancy: what about quality of life? BJOG. 2008; 115: 1484-93. [ Links ]