Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombia Médica
On-line version ISSN 1657-9534
Colomb. Med. vol.44 no.3 Cali July/Sept. 2013
Original Article
Prediction of prolonged mechanical ventilation for intensive care unit patients: A cohort study
Predicción de la ventilación mecánica prolongada en pacientes de la unidad de cuidado intensivo: Estudio de cohorte
Alvaro Sanabria1,2,3, Ximena Gómez1, Valentín Vega2, Luis Carlos Domínguez2, Camilo Osorio2
1 Head and Neck Service. Department of Surgery. Fundación Abood Shaio. Bogota. Colombia
2 Department of Surgery. Universidad de La Sabana. Chía, Colombia.
3 Unit of Cancerology. Hospital Pablo Tobón Uribe. Departament of Surgery. Universidad de Antioquia. Medellin, Colombia.
*Corresponding Author.
E-mail Address: alvaro.sanabria@unisabana.edu.co (Sanabria A), ximegs@hotmail.com (Gómez X), neil.vega@unisabana.edu.co (Vega V), luis.dominguez@unisabana.edu.co (Dominguez LC), camilo.osorio@unisabana.edu.co (Osorio C)
Article history: Received Oct 30 2012 Received in revised form Nov 25 2012 Accepted Sep 09 2013
Abstract
Introduction: There are no established guidelines for selecting patients for early tracheostomy. The aim was to determine the factors that could predict the possibility of intubation longer than 7 days in critically ill adult patients.
Methods: This is cohort study made at a general intensive care unit. Patients who required at least 48 hours of mechanical ventilation were included. Data on the clinical and physiologic features were collected for every intubated patient on the third day. Uni- and multivariate statistical analyses were conducted to determine the variables associated with extubation.
Results: 163 (62%) were male, and the median age was 59±17 years. Almost one-third (36%) of patients required mechanical ventilation longer than 7 days. The variables strongly associated with prolonged mechanical ventilation were: age (HR 0.97 (95% CI 0.96-0.99); diagnosis of surgical emergency in a patient with a medical condition (HR 3.68 (95% CI 1.62-8.35), diagnosis of surgical condition-non emergency (HR 8.17 (95% CI 2.12-31.3); diagnosis of non-surgical-medical condition (HR 5.26 (95% CI 1.85-14.9); APACHE II (HR 0.91 (95% CI 0.85-0.97) and SAPS II score (HR 1.04 (95% CI 1.00-1.09) The area under ROC curve used for prediction was 0.52. 16% of patients were extubated after day 8 of intubation.
Conclusions: It was not possible to predict early extubation in critically ill adult patients with invasive mechanical ventilation with common clinical scales used at the ICU. However, the probability of successfully weaning patients from mechanical ventilation without a tracheostomy is low after the eighth day of intubation.
Keywords: tracheostomy, artificial respiration, intensive care units, ventilator weaning, intratracheal intubation, risk factors.
Resumen
Introducción: No existen guías establecidas para seleccionar los pacientes para traqueostomía precoz. El objetivo del estudio fue determinar los factores que pueden predecir la posibilidad de intubación mayor a 7 días en pacientes adultos en la UCI.
Métodos: Este es un estudio de cohorte realizado en la UCI. Los pacientes en ventilación mecánica mayor a 48 horas fueron incluidos. Se recogieron los datos clínicos y fisiológicos de cada paciente al tercer día de intubación. Se realizaron análisis uní y multivariado para determinar las variables asociadas a intubación prolongada.
Resultados: 163 (62%) fueron hombres y la edad media fue de 59±17 años. Aproximadamente un tercio de los pacientes (36%) requirieron ventilación mecánica mayor a 7 días. Las variables asociadas con ventilación mecánica prolongada fueron: edad (HR 0.97 (95% CI 0.96-0.99); diagnóstico de urgencia quirúrgica en un paciente con enfermedad médica (HR 3.68 (95% CI 1.62-8.35),diagnostico de necesidad de cirugía no urgente (HR 8.17 (95% CI 2.12-31.3); diagnóstico de enfermedad medica no quirúrgica (HR 5.26 (95% CI 1.85-14.9); APACHE II (HR 0.91 (95% CI 0.85-0.97) y puntaje SAPS II (HR 1.04 (95% CI 1.00-1.09). El área bajo la curva ROC para predicción fue de 0.52. 16% de los pacientes fueron extubados después de 8 días de intubación.
Conclusiones: No fue posible predecir la extubation precoz en pacientes de la unidad de cuidado intensivo en ventilación mecánica con las variables comúnmente usadas. La probabilidad de destete de ventilación mecánica después de 8 días de intubación sin realizar traqueostomía es baja.
Palabras Clave: Traqueostomía, respiración artificial, unidad de cuidado intensivo, destete del ventilador, intubación intratraqueal, factores de riesgo.
Introduction
Tracheostomy is the most common elective surgical procedure performed by surgeons on intensive care patients. Nearly 24% of patients in the intensive care unit (ICU) need a tracheostomy1.Tracheostomy is recommended because of its potential advantages over tracheal intubation, which include: a lower frequency of laryngeal ulcers, less resistance in the airway, less dead space and better tolerance by patients2 Currently, the main indications for a tracheostomy are: prolonged mechanical ventilation (because of the possibility of reduced mechanical ventilation time), length of stay in the ICU, and associated mortality3.
However, the prediction of prolonged mechanical ventilation is challenging. Currently, there is not a validated instrument that predicts which patients in the ICU will require prolonged ventilation and which are candidates for early tracheostomy. Most decisions are based on clinical criteria, which are often found to be late, subjective and unreliable4.
Some randomized controlled trials have shown that an early tracheostomy2 (made before the seventh day of tracheal intubation) has benefits for the patient, but the challenge is in determining which patients will be eligible for an early surgical procedure. The objective of this study was to identify and assess the factors that could help to predict prolonged mechanical ventilation, which is defined as longer than 7 days (the time limit set for defininge an early vs. late tracheostomy), in patients during the first three days of their ICU stay. These factors once identified could be used in clinical decision-making. We consider that three days is sufficient time to control major clinical conditions and to define the next steps in the mechanical ventilation plan, including extubation or long-term maintenance of mechanical ventilation.
Materials and Methods
This study was a cohort study and was approved by the Ethics in Research Committee. We reviewed the medical charts for adult patients who were admitted to a general ICU at the Fundacion Abood Shaio Clinic in Bogota, Colombia, between January 1, 2007 and December 31, 2008 and who required at least 48 hours of mechanical ventilation with tracheal intubation. The decision to perform a tracheostomy or to wean from mechanical ventilation was made exclusively by the ICU physician. This decision was based on their clinical judgment at the time of the extubation, and considered classical hemodynamic and pulmonary factors, sepsis control, etc.
Patients with neck conditions and non-invasive ventilation who were intubated at an external institution for acute airway compression, patients transferred to other ICUs, and patients that survived less than seven days after intubation were all excluded from the study to reduce the risk of selection bias. Data were collected from the medical records by an independent reviewer using a specifically designed form at the third day of intubation. The form included demographic data (age, sex, weight, height), clinical data (diagnosis prior to ICU admission, indications for mechanical ventilation, SOFA score, APACHE II score, SAPS II score, Glasgow Coma Score, vital signs, laboratory and imaging data) and therapeutic variables (vasoactive drugs, antibiotics, immunosuppressant's and bronchodilators) commonly used at the ICU. The main outcome was the period of time to extubation, measured in days. The scores selected (SOFA, APACHE II and SAPS II) were used as variables to adjust the final outcome in order to avoid selection bias.
A sample size calculation of 350 patients was made using the Carley nomogram, assuming that the classical variables were the best predictors of mechanical ventilation discontinuation. We selected a rate of prolonged mechanical ventilation (longer than 7 days) of 20% with a sensitivity of 90%, a specificity of 90% and a precision of 7% for any prediction variable. The information derived from the special forms drawn up was entered into a database (Excel ®2007, Microsoft Corp).
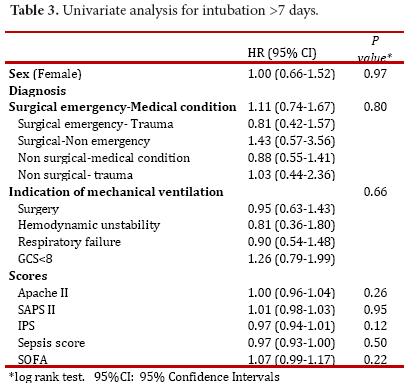
For statistical analysis, commercially available software was used (Stata ® 9.0, Stata Corporation, College Station, Texas). Descriptive statistics were used to show the distribution of variables (mean ± sd, median and range for continuous variables and frequency for discrete variables). As mechanical ventilation was a time-to-event outcome, we calculated the time from the date of intubation until the thirtieth day after admission. A univariate analysis using the Kaplan-Meier method was used to explore the relationship between the baseline variables and the outcome events. The results were reported using a Mantel-Cox Hazard Ratio (HR) with a 95% confidence interval. The log-rank test was used to define statistical significance. A Cox proportional hazard regression analysis was used to assess the independent effect of the variables on mechanical ventilation. For ordinal variables, an indicator variable was created for each level in the logistical and the Cox proportional hazard regression analyses. As many clinical variables are used with different scores, we decided to include only scores in the regression analysis in order to avoid co-linearity. The predictive capability of the model was assessed with an area under the ROC curve analysis. For all statistical tests, p <0.05 was considered statistically significant.
Results
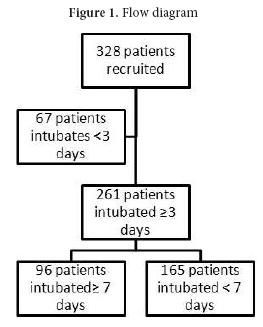
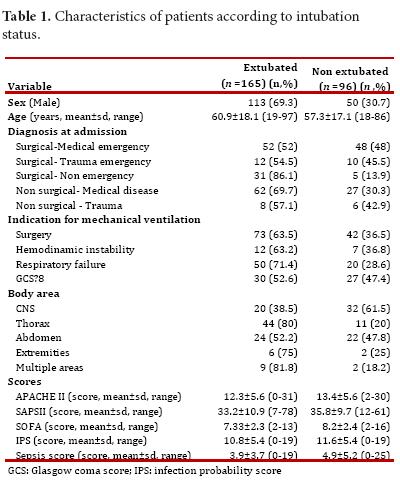
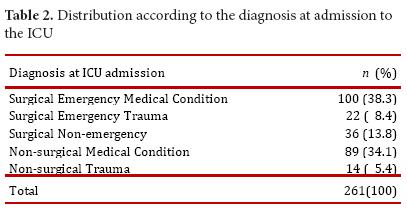
The clinical charts of 328 patients met the inclusion and exclusion criteria. From these, 261 patients were still intubated after the third day, which constituted the population studied (Fig. 1). The mean age was 59.6 ± 17.8 years (range 18–97 years; median of 64 years), and 163 patients were men (62.4%) (Table 1). The admission diagnoses at the ICU are shown in Table 2. They were classified as surgical or non-surgical, emergent or non-emergent, and the presence of medical, surgical or trauma conditions were also noted. The indications for ventilatory support were: surgery in 115 patients (44.1%), hemodynamic instability in 19 patients (7.3%), respiratory failure in 70 patients (26.8%) and Glasgow coma score <8 in 57 patients (21.8%)
The mean score and standard deviation at admission for the SOFA was found to be 7.9 ± 2.3 (range 2-15); for the APACHE II it was found to be 15.1 ± 5.7 (4-31); for the SAPS it was 37.9 ± 10.6 (9-87) and for the GCS it was 12.3 ±3.7 (3-15).
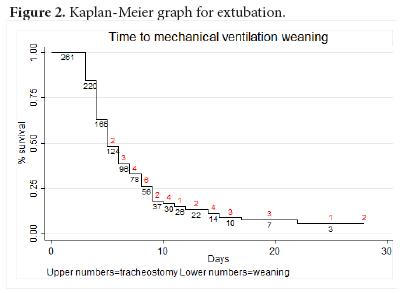
The mean time of mechanical ventilation was 6.6± 4.2 days (3-28, median 5 days). Ninety-six patients (36.8%) were intubated for more than 6 days, and 37 patients (14.2%) underwent tracheostomy at a mean time of 9.5 ± 4 days (4-20), with 75.7% of them completed after day 7. Figure 2 shows a Kaplan-Meier graph with the weaning of mechanical ventilation as the main outcome and tracheostomy as a lost event. The univariate analysis results are shown in Table 3.
The multivariable Cox model included gender, age, diagnosis at admission, and indication of mechanical ventilation, as well as APACHE II, SAPS and SOFA scores. The final model contained the following clinical and statistically significant variables: age (HR 0.97 (95% CI 0.96-0.99)); diagnosis of surgical emergency in a patient with a medical condition (HR 3.68 (95% CI 1.62-8.35)), diagnosis of a non- emergency surgical condition (HR 8.17 (95% CI 2.12-31.3)); diagnosis of a non-surgical medical condition (HR 5.26 (95% CI 1.85-14.9)); APACHE II (HR 0.91 (95% CI 0.85-0.97)) and SAPS II (HR 1.04 (95% CI 1.00-1.09)). The prediction based on these variables had an area under the ROC curve of 0.52, which is considered poor.
The life table derived from the Kaplan-Meier analysis provides clinicians with data that could assist in decision making for a tracheostomy. At 8 and 10 days, the probability of being extubated was 25.7% and 16.2%, respectively.
Discussion
Tracheostomy has been performed since 1500 BC.5Today, tracheostomy is performed in nearly 25% of all patients admitted to the ICU. Itis commonly indicated for prolonged mechanical ventilation1,6 because it is associated with fewer larynx and oral ulcers, less ventilator resistance and dead space, increased comfort and secretions management, reduced sedative requirement, ease of communication and oral feeding7. Currently, some studies have shown that there are significant benefits for early tracheostomy (less than 7 days of intubation) in intubated patients. In 1989, the American College of Chest Physicians published a consensus document that recommended early tracheostomy in patients with an estimated intubation time longer than 21 days8. Later, in a prospective trial with 90 patients, Brook et al.9, found that patients with an early tracheostomy had lower hospital costs. Hsu et al.1, showed that patients who underwent a tracheostomy after three weeks of mechanical ventilation had a higher frequency of re-intubation and increased mortality. A meta-analysis of tracheostomy patients conducted in 2005 reported a decreased length of stay in the ICU (15.3 days (CI 95%: 6.1 – 24.6)) and less time on mechanical ventilation (8.5 days (CI 95%: 1.7- 15.3))2. Also, Freeman et al.10, confirmed these results in an administrative data study. Therefore, patients with a predicted prolonged intubation would benefit from a tracheostomy made within the first week of intubation. Recent studies from Germany11,12, USA13, Spain14 and Italy15, have shown an improvement in secondary outcomes as a function of the length of stay in the ICU, days of mechanical ventilation, and ventilator associated pneumonia, but not for mortality.
However, it is difficult to predict prolonged intubation. In 1990, Heffner et al.4, found that a PEEP less than or equal to 10 cm H2O, a PaO2/PAO2 ratio higher than 0.4 and a quick improvement in radiological findings from a thorax x-ray were associated with a mechanical ventilation time of less than 14 days. Troche et al.16, showed that the serum albumin levels, indications for intubation (respiratory failure), the sepsis scale score, the number of organs in failure and the lung injury scale score were all predictors of prolonged mechanical ventilation. However, the validation of these factors had a low predictive value (24%). Similarly, Sellers et al.17, found that age and a PaO2/FiO2 on the third day of intubation were predictors of prolonged intubation. On the other hand, Kollef et al.18, found that nosocomial pneumonia, aerosolized medication administration, re-intubation and lung aspiration increased the necessity for a tracheostomy. Other authors have reported that bilateral blunt thoracic trauma, age, brain trauma, a previous diagnosis of COPD, a high APACHE-II score, a high SAPS scores, a high Glasgow Coma Scores, BMI>20 kg/m2, levels of CRP>10 mg/L are also predictors of prolonged ventilation19,20.
Although many predictive factors have been identified, the research has been very disparate and heterogeneous in relation to the study populations (surgical, trauma) such that the results cannot be extrapolated to other populations; a different scale is required for each type of patient. Currently, there is not a simple scale that predicts time of mechanical ventilation in patients admitted to a general ICU. Therefore, the indications for an early tracheostomy remain subjective.
This study demonstrated that the factors analyzed that have shown good reliability for other outcomes and which are currently being used at ICU´s around the world are poor predictors of prolonged mechanical ventilation. Furthermore, the predictive power of the factors identified by multivariate analysis is so poor that it is impossible to predict prolonged intubation.
This finding can be explained by the dynamic nature of ICU patients where significant clinical changes could occur within a few hours, thus making the initial factors irrelevant as time passes. On the other hand, the variability of treatments and clinical criteria between physicians could obscure the identification of predictive factors, and the interaction between the known and unknown factors could hide the real predictive factors.
However, this study also offers information on the time of tracheostomy based on the use of a survival analysis. As shown, the probability for extubation is approximately 25% after day 8 and less than 18% after day 9. Despite the variability, it is reasonable to suggest that patients who reach these limitis are good candidates for tracheostomy based on their low realistic probability of being extubated. Furthermore, if patients who have been intubated for six days are likely to be extubated within the next two days, physicians may simply choose to observe the patients. On the other hand, if the estimated time of mechanical ventilation is longer, a tracheostomy can be performed earlier.
Finally, some weaknesses of this study should be addressed. First, the observational design is intrinsically prone to bias. Second, the variability of decisions by physicians impedes the use of standard and reliable criteria for uniform decision-making. Although we tried to control for these weaknesses using objective criteria, they could affect the final results and should be analyzed carefully.
In conclusion, based upon this study, it was not possible to identify predictive factors for prolonged mechanical ventilation. Therefore, decisions concerning the need for a tracheostomy cannot be made at this time based on these factors. However, an intubation time of more than 8 days is associated with a low probability of extubation and can be used as a reference point in the decision to perform a tracheostomy.
References
1. Hsu CL, Chen KY, Chang CH, Jerng JS, Yu CJ, Yang PC. Timing of tracheostomy as a determinant of weaning success in critically ill patients: a retrospective study. Crit Care. 2005; 9(1): R46-R52. [ Links ]
2. Griffiths J, Barber VS, Morgan L, Young JD. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005; 330(7502): 1243. [ Links ]
3. De LP, Bedert L, Delcroix M, Depuydt P, Lauwers G, Sokolov Y, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007; 32(3): 412-21. [ Links ]
4. Heffner JE, Zamora CA. Clinical predictors of prolonged translaryngeal intubation in patients with the adult respiratory distress syndrome. Chest. 1990; 97(2): 447-52. [ Links ]
5. Schauer JM, Engle LL, Maugher DT, Cherry RA. Does acuity matter?. Optimal timing of tracheostomy stratified by injury severity. J Trauma. 2009; 66(1): 220-5. [ Links ]
6. Arabi YM, Alhashemi JA, Tamim HM, Esteban A, Haddad SH, Dawood A, et al. The impact of time to tracheostomy on mechanical ventilation duration, length of stay, and mortality in intensive care unit patients. J Crit Care. 2009; 24(3): 435-40. [ Links ]
7. Shirawi N, Arabi Y. Bench-to-bedside review: early tracheostomy in critically ill trauma patients. Crit Care. 2006; 10(1): 201. [ Links ]
8. Plummer AL, Gracey DR. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest. 1989; 96(1): 178-80. [ Links ]
9. Brook AD, Sherman G, Malen J, Kollef MH. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care. 2000; 9(5): 352-9. [ Links ]
10. Freeman BD, Borecki IB, Coopersmith CM, Buchman TG. Relationship between tracheostomy timing and duration of mechanical ventilation in critically ill patients. Crit Care Med. 2005; 33(11): 2513-20. [ Links ]
11. Koch T, Hecker B, Hecker A, Brenck F, Preuss M, Schmelzer T, et al. Early tracheostomy decreases ventilation time but has no impact on mortality of intensive care patients: a randomized study. Langenbecks Arch Surg. 2012; 397(6): 1001-8. [ Links ]
12. Bickenbach J, Fries M, Offermanns V, von SR, Rossaint R, Marx G, et al. Impact of early vs. late tracheostomy on weaning: a retrospective analysis. Minerva Anestesiol. 2011; 77(12): 1176-83. [ Links ]
13. Devarajan J, Vydyanathan A, Xu M, Murthy SM, McCurry KR, Sessler DI, et al. Early tracheostomy is associated with improved outcomes in patients who require prolonged mechanical ventilation after cardiac surgery. J Am Coll Surg. 2012; 214(6): 1008-16. [ Links ]
14. Gandia-Martinez F, Martinez-Gil I, Andaluz-Ojeda D, Bobillo de LF, Parra-Morais L, Diez-Gutierrez F. [Analysis of early tracheostomy and its impact on development of pneumonia, use of resources and mortality in neurocritically ill patients]. Neurocirugia (Astur). 2010; 21(3): 211-21. [ Links ]
15. Terragni PP, Antonelli M, Fumagalli R, Faggiano C, Berardino M, Pallavicini FB, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: a randomized controlled trial. JAMA. 2010; 303(15): 1483-9. [ Links ]
16. Troche G, Moine P. Is the duration of mechanical ventilation predictable?. Chest. 1997; 112(3): 745-51. [ Links ]
17. Sellers BJ, Davis BL, Larkin PW, Morris SE, Saffle JR. Early prediction of prolonged ventilator dependence in thermally injured patients. J Trauma. 1997; 43(6): 899-903. [ Links ]
18. Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999; 27(9): 1714-20. [ Links ]
19. Dimopoulou I, Anthi A, Lignos M, Boukouvalas E, Evangelou E, Routsi C, et al. Prediction of prolonged ventilatory support in blunt thoracic trauma patients. Intensive Care Med. 2003; 29(7): 1101-5. [ Links ]
20. Gursel G. Determinants of the length of mechanical ventilation in patients with COPD in the intensive care unit. Respiration. 2005; 72(1): 61-7. [ Links ]