Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombia Médica
On-line version ISSN 1657-9534
Colomb. Med. vol.44 no.3 Cali July/Sept. 2013
Case Report
Synthetic dural graft septoplasty in epistaxis from hereditary hemorrhagic telangiectasia
Septoplastia con injerto de dura sintética en epistaxis por telangiectasias hemorrágicas hereditarias
Wilfred Burckhardt B, Claudia Patricia Guerra
Universidad del Valle. Hospital Universitario del Valle, Colombia
*Corresponding Author.
E-mail Address: wbb1960@yahoo.es (Burckhardt W), wetclaudiaguerra@hotmail.com (Guerra CP.)
Article history: Received Nov 14 2012 Received in revised form Dec 06 2012 Accepted : Aug 08 2013
Abstract
It is an autosomal dominant vascular disorder, which has a variety of clinical manifestations, with epistaxis being one of the most common. Many treatment options exist for epistaxis, but with no consensus on which is the method of choice. We describe the case of a patient with hereditary hemorrhagic telangiectasia (HHT) secondary epistaxis with septoplasty managed with synthetic hard graft, which improved intensity and frequency of bleeding episodes. This technique is a variant of the septodermoplasty described by several authors, but the use of synthetic dura can help in obtaining better results and avoid taking skin grafts from other sites different from the surgical site.
Keywords: hereditary hemorrhagic telangiectasia, arteriovenous malformation, epistaxis, septoplasty, graft, synthetic dura.
Resumen
Esta condición es un trastorno vascular autosómico dominante, que tiene una variedad de manifestaciones clínicas; entre las más comunes, se encuentra epistaxis. Existen múltiples opciones terapéuticas para la epistaxis, pero no hay un consenso sobre cuál es el método de elección. Se describe el caso de un paciente con epistaxis secundaria a telangiectasias hemorrágicas hereditarias (THH) manejado con septoplastia con injerto de dura sintética, la cual obtuvo mejoría en la intensidad y frecuencia de los episodios de sangrados. Esta técnica es un variante de la septodermoplastia descrita por diversos autores, pero el uso de dura sintética puede ayudar a obtener mejores resultados y evita toma de injertos dérmicos de otros sitios diferentes al sitio quirúrgico.
Palabras Clave: telangiectasias hemorrágicas hereditarias, malformación arteriovenosa, epistaxis, septoplastia, injerto, dura sintética.
Introduction
A great number of topical, systemic, and surgical treatments are available for epistaxis, with variable effectiveness, among them: cauterization, nasal packing, sclerotherapy, embolization, arterial ligation, nasal humidification, laser ablation, septal dermoplasty, and nasal closure; but without consensus on the method of choice. Saunders described this technique for the first time in 1960, consisting in the elimination of the original nasal mucosa and its substitution by a skin graft normally taken from the thigh and sometimes from the oral mucosa. The technique has undergone further modifications, but it generally seems to truly eliminate epistaxis, although later minor interventions are necessary to eliminate peripheral telangiectasias. Diminished sense of smell may be noted, along with increased propensity to develop infections of the sinuses. These adverse effects can influence on the quality of life of patients, given that a secondary effect is that the perception of flavor in foods is affected1,2.
Clinical case
Patient, 38 years of age, in consultation due to a condition of recurring epistaxis since eight years of age, which appeared with a frequency of two to three episodes per day, in light to moderate amount. On multiple occasions, the patient had required nasal packing and cauterizations.
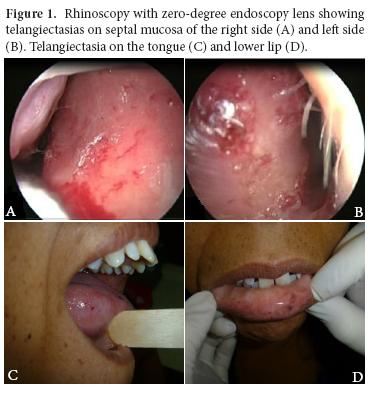
Secondary to the epistaxis, the patient presented iron-deficiency anemia, for which the patient received several blood transfusions. The patient's family group included the patient's mother and a son, both presenting a similar clinical condition. Physical exam evidenced telangiectasias in lower turbinates and bilateral nasal septum, as well as on the oral mucosa and tongue (Fig. 1). No cutaneous lesions were found. Upper GI endoscopy was performed, showing a 3-mm ruby-colored flat lesion on the lesser curvature of the stomach (gastric angiodysplasia). Through pulmonary arteriography right pulmonary arteriovenous malformation was detected.
By applying diagnostic criteria for HHT and complying with all, the definite diagnosis of this condition was considered, without the possibility of genetic tests1,3.
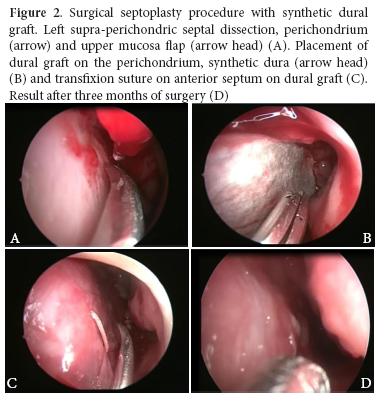
To control epistaxis episodes, the patient was taken to surgery and a modified septal dermoplasty technique was performed, consisting of a hemitransfixion incision on the caudal septal with No. 15 scalpel blade, followed by a septal dissection at supra-perichondric level with the Cottle dissector, creating an upper and lower ipsilateral tunnel.
Then, the septal mucosa was resected leaving a small upper and lower mucosa flap. Synthetic dural graft (Surgisisâ BiodesignTM –Dural Graft, REF G31092, made in the United States) was placed on the perichondrium, leaving it covered by the upper and lower mucosa flaps. Thereafter, an absorbable suture stitch was placed transfixing on the anterior and posterior septum; this was then covered with Surgicelâ®.
This procedure was carried out unilaterally. During subsequent controls, adequate epithelization of the graft was noted along with decreased episodes of bleeding. After three months, the patient was again taken to surgery to perform this same procedure on the contralateral nostril (Fig. 2). After surgery, there was no evidence of septal perforation, infection, telangiectasias on borders, loss of smell, or any other complication, completing one year of postoperative follow up.
Discussion
Penetrance shows relationship with age and its manifestations increase and develop throughout life. Epistaxis, mucocutaneous telangiectasias, and iron-deficiency anemia stand out among the most important clinical manifestations. Approximately 50% of the individuals diagnosed report epistaxis by 10 years of age and 80-90% by 21 years of age. Up to 95% eventually develop recurrent epistaxis. Epistaxis emerges spontaneously. Many patients with occasional epistaxis episodes only require treatment with iron supplements, while others who experience significant bleeding episodes may require transfusions and diverse forms of nasal interventions4.
Other manifestations that can be found in these patients are cutaneous and oral telangiectasias (50-80% of the patients), pulmonary AVM (11-30%), gastrointestinal bleeding (11-40%), hepatic AVM (30%), cerebral AVM (10-15%), and spinal AVM (1%). According to the location of these AVM, clinical findings will emerge like gastrointestinal hemorrhage, dyspnea, thoracic pain, hemothorax, hemoptysis, cyanosis, thoracic breathing, hypoxemia, polycythemia, pulmonary embolism, migraine, convulsions, cerebrovascular events, and transient ischemic accident (11-55%), subarachnoid hemorrhage, cerebral abscess, portal hypertension, among others2.
Confirmation of the diagnosis is obtained through genetic tests for endoglin mutations, ALK-1 or SMAD4 genes.
An important number of topical, systemic, and surgical treatments are available for epistaxis, with variable effectiveness, among which are: cauterization, nasal packing, sclerotherapy, embolization, arterial ligation, nasal humidification, laser ablation, radiofrequency coblation, septal dermoplasty, and nasal closure2,3,5,6.
Septal dermoplasty is a skin graft technique. The principle of this procedure is the substitution of the fragile respiratory mucosa of the nose with strong skin grafts (generally from the thigh or oral mucosa) that withstand trauma and, thus, avoid bleeding. Its effectiveness has been objectively demonstrated in reducing the mean number of transfusions required due to epistaxis. The main complications reported with this procedure are: nasal odor (78%), formation of scabs (72%), diminished sense of smell (58%), increased sinus infections (30%). A minority of patients experience worsening of asthma or allergies (8%), facial numbing or tingling (10%), increased eye infections (8%), or nasal pain (14%). Most of the patients, 88%, can breathe through the nose after surgery7.
Modification of the septal dermoplasty technique by substituting the skin graft for a synthetic dural graft can diminish the incidence of all these possible complications registered in the literature and also avoids taking skin from a second surgical field, as evidenced in the current case reported where after surgery there was no evidence of septal perforation, infection, telangiectasias on the borders, loss of smell, or any other complication, completing one year of post-operatory follow up.
Conclusion
An important number of topical, systemic, and surgical treatments are available for epistaxis, with variable effectiveness, but without consensus on the method of choice. Generally, we begin with conservative medical management and if no adequate response is found, the following step involves more invasive interventions. Unlike the septal dermoplasty described in literature, this septoplasty technique with synthetic dural graft avoids taking skin grafts from a second surgical field, with excellent results. After the septal dermoplasty, the literature reports improved quality of life, diminished bleeding episodes, and increased hemoglobin figures. According to this, the patient in the present case has shown clinical improvement, with diminished frequency, amount, and duration time of bleeding. One year after surgery there was no evidence of septal perforation, infection, telangiectasias on the borders, or loss of smell.
References
1. McDonald J, Bayrak-Toydemir P, Pyeritz RE. Hereditary hemorrhagic telangiectasia: an overview of diagnosis, management, and pathogenesis. Genet Med. 2011;13(7):607-16. [ Links ]
2. Zarrabeitia R. A review on clinical management and pharmacological therapy on hereditary haemorrhagic telangiectasia (HHT). Curr Vasc Pharmacol.2010; 8(4): 473-81. [ Links ]
3. Trojanowski P, Jargiello T, Trojanowska A, Klatka J. Epistaxis in patients with hereditary hemorrhagic telangiectasia treated with selective arterial embolization. Acta Radiol. 2011;52(8):846-9. [ Links ]
4. Dheyauldeen S, Abdelnoor M, Bachmann-Harildstad G. The natural history of epistaxis in patients with hereditary hemorrhagic telangiectasia in the Norwegian population: a cross-sectional study. Am J Rhinol Allergy. 2011;25(4):214-8. [ Links ]
5. Jørgensen G, Lange B, Wanscher JH, Kjeldsen AD. Efficiency of laser treatment in patients with hereditary hemorrhagic telangiectasia. Eur Arch Otorhinolaryngol. 2011;268(12):1765-70. [ Links ]
6. Joshi H, Woodworth BA, Carney AS. Coblation for epistaxis management in patients with hereditary haemorrhagic telangiectasia: a multicentre case series. J Laryngol Otol. 2011; 25(11):1176-80 [ Links ]
7. Levine CG, Ross DA, Henderson KJ, Leder SB, White RI Jr. Long-term complications of septal dermoplasty in patients with hereditary hemorrhagictelangiectasia. Otolaryngol Head Neck Surg. 2008; 138(6):721-4. [ Links ]