Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Colombia Médica
versión On-line ISSN 1657-9534
Colomb. Med. vol.47 no.1 Cali ene./mar. 2016
Original Article
Self-reported vaccination in the elderly : SABE Bogotá study, Colombia
El auto reporte de vacunación en los adultos mayores: Estudio SABE Bogotá, Colombia
Carlos Cano Gutiérrez1,3, Carlos Reyes-Ortiz2, Miguel Germán Borda1,4, Antonio Arciniegas1,4
1 Instituto de Envejecimiento, Facultad de Medicina, Pontificia Universidad Javeriana, Bogotá Colombia.
2 UTHealth, The University of Texas Health Science Center at Houston, Department of Internal Medicine, Division of Geriatric and Palliative Medicine, Houston, TX, USA.
3 Unidad de Geriatría, Hospital Universitario San Ignacio. Bogotá Colombia.
4 Semillero de Neurociencias y Envejecimiento, Facultad de Medicina, Pontificia Universiadad Javeriana, Bogotá Colombia.
Cano GC, Reyes-Ortiz C, Borda MG, Arciniegas A. Self-reported vaccination in the elderly. Colomb Med (Cali). 2016; 47(1):25-30.
© 2016. Universidad del Valle. This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Article history: Received: 23 September 2015 - Revised: 04 December 2015 - Accepted: 05 January 2016
Corresponding author:
Carlos Cano Gutiérrez. Principal Researcher of SABE Bogotá Study. Address: Carrera 7 No. 40-62, Hospital San Ignacio Piso 8 Facultad de Medicina, Bogotá, Colombia.Tel: +57 1 320 8320, ext 2764; fax: +57 1 320 8320, ext 2751.
E-mail: ccano@javeriana.edu.co.
Abstract
Objectives: To determine the frequency of vaccination in older adults within the city of Bogotá and to estimate the association with sociodemographic and health factors.
Methods: This is a secondary data analysis from the SABE-Bogotá Study, a cross-sectional population-based study that included a total of 2,000 persons aged 60 years. Weighted percentages for self-reported vaccination [influenza, pneumococcal, tetanus] were determined. The association between vaccination and covariates was evaluate by logistic regression models.
Results: A total of 73.0% of respondents received influenza, 57.8% pneumococcal and 47.6% tetanus vaccine. Factors independently associated with vaccination included: 1- age (65-74 years had higher odds of receiving vaccinations, compared to 60-64 years; 2socioeconomic status (SES) (higher SES had lower odds of having influenza and pneumococcal vaccines, compared to those with lower SES); 3- health insurance (those with contributive or subsidized health insurance had higher odds (between 3 and 5 times higher) of having vaccinations, compared to those with no insurance); 4- older adults with better functional status (greater Lawton scores) had increased odds for all vaccinations; 5- older adults with higher comorbidity had increased odds for influenza and pneumococcal vaccinations.
Conclusion: Vaccination campaigns should be strengthened to increase vaccination coverage, especially in the group more reticent to vaccination or vulnerable to reach it such as the disable elder.
Keywords: Aged, vaccination, influenza, pneumococcal vaccines, tetanus, epidemiologic studies
Resumen
Objetivos: determinar la frecuencia de vacunación en la población adulta mayor de la ciudad de Bogotá, y estimar la asociación con factores sociodemográficos y de salud.
Métodos: Este es un análisis secundario de datos del estudio SABE-Bogotá, un estudio poblacional transversal que incluyó un total de 2,000 personas mayores de 60 años. Se obtuvieron porcentajes ponderados del auto-reporte de vacunación (influenza, neumococo, tétano). La asociación entre la vacunación y otras variables se evaluó mediante modelos de regresión logística.
Resultados: el 73.0% se vacunó contra la Influenza, 57.8% contra el Neumococo y el 47.6% recibió la antitetánica. Los factores que estaba independientemente asociados con la vacunación incluyen: 1-edad (6574 tenían probabilidad aumentada comparada con 60-64 años); 2- nivel socioeconómico (NSE) (mayor NSE tenían menos probabilidades de tener vacunas contra la influenza y neumococo, en comparación con aquellos con menor SES); 3- seguro de salud (con seguro contributivo o subsidiado tenían probabilidades más altas, (entre 3 y 5 veces mayor) de tener vacunación contra la influenza, neumococo y tétanos, en comparación con aquellos que no tienen seguro); 4- aquellos con estado funcional mejor (puntaje mayor Lawton) tenían probabilidades mayores para todas las vacunas; 5- aquellos con morbilidad aumentada tenían probabilidades mayores para tener vacunas de influenza y neumococo.
Conclusión: Las campañas de vacunación se deben fortalecer para incrementan la cobertura, especialmente en el grupo más reacio a la vacunación o vulnerable para alcanzarla tales como los adultos mayores con discapacidad.
Palabras clave: Años de edad, la vacunación, la gripe, las vacunas neumocócicas, tétanos, los estudios epidemiológicos
Introduction
Elderly population has increased rapidly worldwide over the last decades due to the demographic transition1. Until now life expectancy has doubled and in 2100 it is projected to triple2. Population aging has increased the demand for health services by older adults. Because of their decreased physiological reserve, they are prone to present more diseases3. Thus, creating the need for cost-effective public policies that protect older adults. Prevention using vaccines has been an effective measure in increasing survival of millions of people around the world. Immunization in older adults has just been developed during the last decade. This development has derived from a better understanding of immunosenescence, the central theory that explains the age related changes of the immune system, including the increased susceptibility to infections with longer duration and severity, atypical presentations of diseases, lower response to immunization and a higher prevalence of neoplasia3,4.
The Center for Disease Control and Prevention (CDC) of the United States, in their vaccination schedule for 2013, recommends that people over 60 should be vaccinated against influenza, Diphtheria, Pertussis, Tetanus (DPT) and, Herpes Zoster and in individuals over 65 years also against Pneumococcus 5. However, the reported CDC vaccination rates still remain low. Coverage for vaccination among individuals of 65 years and older is 59.2% for influenza, 59.9% for Pneumococcus and 55.1% for tetanus, and these rates still remain below target rates6. Despite the increase in vaccination against pneumococcus between 1997 and 2005, 25% of older adults still reported they never received this vaccine7. Studies in Latin America, reported that older adults learned about vaccination programs through ads in mass media such as television and radio, whereas only 5% received this information from a physician or healthcare provider. Additionally, 83% of those who were not vaccinated reported that the main reason for avoiding vaccination was fear of potential side effects or because they believed that it would not work8.
This is important because although the infection with influenza virus is usually self-limited, in the elderly it may have serious complications. About 90% of deaths caused by influenza occur in individuals over 65 years, often secondary to pneumonia, in which the main risk factors are increasing age and exacerbation of cardiopulmonary diseases9,10. Individuals over 85 years with influenza and pneumonia have 32 times higher risk of death, and if they have influenza and any other comorbidity the risk of death is 16 times higher10. In Colombian, respiratory diseases are the third cause of death among older adults between 65 and 75 years, and the second cause of death in those over 80 years. In most cases, these clinical complications are secondary to infection and are preventable11.
Similarly, respiratory pneumococcal disease is a major cause of death in the elderly and its main complication is pneumonia, with mortality rates of 20% in those over 65 years and 40% for those over 85 years12. There is no evidence suggesting that pneumococcal vaccine prevents pneumonia, however, evidence suggests it decreases the severity of the infection and the probability of pneumococcal bacteremia that can result in multiple diseases such as meningitis. Additionally, pneumococcal vaccination reduces the risk of pneumococcal bacteremia by 44% reduction of the risk13.
In addition, tetanus is a serious disease, which presents with mortality rates of up to 50%14,15. This is especially important in third world countries, which often have high incidence of tetanus14. Although in Colombia, we have had a significant reduction, there are still an elevated number of cases and a substantial underreport15. According to the Instituto Nacional de Salud de Colombia, however, between 2000 and 2002, 28 cases of tetanus were reported16.
In Bogotá, capital city of Colombia, there were more than 7.5 million inhabitants in 2011, of which 10.7% were persons aged 60 years and older17,18. Influenza, pneumococcal and tetanus vaccines are available free of cost for persons 60 years and older in Bogota, Colombia17,18.
The objectives of this study were to determine the frequency of vaccination and to estimate the association with sociodemographic and health factors in a sample of older adults in the city.
Materials and Methods
This report is a secondary data analysis from the Salud Bienestar y Envejecimiento (SABE) Bogotá Study, a cross-sectional survey conducted during December of 2012. The SABE Bogotá Study was designed using a probabilistic sampling scheme by clusters (housing segments) with block stratification. A total of 2,000 adults over 60 years of age were interviewed and assessed in their homes. All respondents were community dwelling, and the sample was representative of urban and rural areas of the city, 81.9% of eligible adults agreed to participate in the study. Expanding the survey sample of the SABE study Bogotá, based on population projections for 2012 adjusting by a correction factor by age and sex, the population estimate was of 779,534 older adults19.
The instrument used in the SABE Bogotá study was derived from the international instrument designed by the Pan American Health Organization for the Latin American countries including the most relevant topics to this analysis 20: 1) personal and family data (with sociodemographic data) 2) health status (with self-reported vaccination and comorbidity data) 3) functional evaluation. The instrument was modified and adapted to Colombia’s context19. The research protocol was approved by the IRB at Pontificia Universidad Javeriana. An informed consent was signed by all the study participants.
Variables
Dependent variables. Vaccination was estimated by calculating the frequencies of self-reported pneumococcal (if have ever had), influenza (in the last year) and tetanus (in the last 10 years) vaccinations.
Independent variables. Demographic characteristics were described and categorized in groups of age (60-64, 65-69, 70-74 and ≥75 years), sex, socio-economic status, health insurance, functional status, and comorbidity.
Socio-economic status in Colombia is measured using six categories from 1 the lowest, to 6 the highest. For the current study, we grouped the six strata into three groups: 1-2 (lower), 3-4 (middle) and 5-6 (upper). This was done following the methodology reported by the Departmento Administrativo Nacional de Estadistica (DANE)21. Health insurance was categorized based on the social security health system of Colombia, which offers coverage to all citizens and foreign people in Colombia. It has two affiliation systems: 1) Contributive and 2) Subsidized. And for those that are not included within these two categories, they are categorized as “linked to the system”, known as a transitory category within the system affiliation, and individuals not insured. Their health coverage is granted by “health service institutions contracts” between territorial entities and government institutions. Functional status was assessed using the Lawton Scale, which measures functionality regarding instrumental activities of daily living (IADL) such as using the telephone, taking medications, managing finances, preparing meals, shopping, housekeeping, doing laundry, using transportation22. We used binary scores for each question (capable without problems or incapable) and created a total score from 0 to 8, higher scores indicate more functionality. Comorbidity included history of seven medical conditions: hypertension, diabetes, coronary heart disease, arthritis, stroke, chronic pulmonary obstructive disease or cancer. Respondents were asked: “Has a doctor or a nurse told you that you have...?” for each of the conditions previously listed.
Statistical analyses
To adjust for sampling survey design, data were weighted by using complex survey analyses. To describe characteristics of study population, categorical variables are presented with percentages whereas continuous variables are presented with means ± standard errors. Frequencies of vaccination by sociodemographic factors or Spearman correlation coefficients by functional status or comorbidity were reported, and differences were tested by the Wald Chi-square or correlation analyses. For the multivariate analyses, weighted logistic regression models were used to test the association of independent variables with vaccination (yes= 1, no= 0), obtaining Odds Ratios (ORs) with 95% confidence intervals (CI). Data were analyzed using SAS® version 9.3 for windows (SAS Institute, Cary, North Carolina-USA). The statistical level of significance was set at p <0.05.
Results
General demographic data
Of the 2,000 individuals interviewed for our study, a total of 62.5% were women, with a mean age of 71.1 ± 0.2 years. About a third were individuals aged 75 and older. Socioeconomic status showed the highest proportion in the lower social (45.6%) and middle class (45.9%), and a lower proportion in the upper social class (8.5%). Regarding health insurance, the higher proportion were affiliated with contributive (72.5%) (Table 1).
| Category | n (%) or Mean ± SE |
|---|---|
| Sex | |
| Women | 1,249 (62.5) |
| Age (years) (range 60-100) | |
| Mean number | 71.1 ± 0.2 |
| 60-64 | 506 (26.0) |
| 65-69 | 454 (22.9) |
| 70-74 | 398 (18.8) |
| â¥75 | 642 (32.3) |
| Socio-economic status | |
| Lower class (1-2) | 1,038 (45.6) |
| Middle class (3-4) | 897 (45.9) |
| Upper class (5-6) | 65 (8.5) |
| Health insurance | |
| Contributive | 1,366 (72.5) |
| Subsidized | 571 (24.6) |
| Transitory | 17 (0.8) |
| Not insured | 44 (2.1) |
| (Functional Status Score in Lawton test, IADLs) | |
| Mean score (0-8) | 7.1 ± 0.0 |
| Comorbidity (Number of diseases) | |
| Mean score (0-7) | 1.4 ± 0.0 |
| Data are weighted SE= standard error IADLs= instrumental activities of daily living Comorbidity includes: hypertension, diabetes, coronary heart disease, arthritis, stroke, chronic pulmonary obstructive disease or cancer | |
Vaccination data
Data showed that 73.0% of the population had received vaccine for influenza during the last year, 57.8% have ever had vaccine for pneumococci, and 47.6% for the tetanus during the last 10 years.
In bivariate analyses (Table 2), individuals aged 65 to 69 and 70 to 74 years had higher percentages of influenza, pneumococcus, and tetanus vaccination, compared to those between 60-64 years. No gender differences were found. Older adults with higher SES (Upper class) had lower vaccination percentages for influenza and pneumococcus, compared to those with lower SES, (lower and middle class). Individuals covered by health insurance (contributive, subsidized, or transitory) had higher vaccination percentages. There were significant positive correlations between Lawton scores and all three vaccinations. There were significant positive correlations of comorbidity with influenza and pneumococcal vaccinations.
| Characteristics | Influenza | Pneumococci | Tetanus |
|---|---|---|---|
| (%) | (%) | (%) | |
| Vaccinated individuals, n=2,000 | 73.0 | 57.8 | 47.6 |
| Age (years) | |||
| 60-64 | 62.9 | 48.1 | 40.6 |
| 65-69 | 76.1 | 64.5 | 53.9 |
| 70-74 | 80.5 | 69.0 | 52.4 |
| 75+ | 74.6 | 54.6 | 45.9 |
| p-value | <0.001 | <0.001 | 0.008 |
| Sex | |||
| Women | 73.6 | 58.1 | 45.9 |
| Men | 71.9 | 57.5 | 50.4 |
| p-value | 0.565 | 0.840 | 0.144 |
| Socio-economic strata | |||
| Lower class (1-2) | 76.6 | 58.6 | 49.4 |
| Middle class (3-4) | 76.1 | 63.3 | 47.9 |
| Upper class (5-6) | 36.9 | 24.3 | 35.6 |
| p-value | <0.001 | <0.001 | 0.211 |
| Health insurance | |||
| Contributive | 72.9 | 59.5 | 49.1 |
| Subsidized | 75.3 | 55.4 | 46.1 |
| Transitory | 78.8 | 63.1 | 42.1 |
| Not insured | 44.7 | 23.8 | 17.9 |
| p-value | 0.046 | 0.004 | 0.007 |
| Functional Status. Lawton test (IADLs) | |||
| Continuous score (0-8) | 0.06* | 0.09* | 0.13* |
| p-value | 0.003 | <.001 | <.001 |
| Comorbidity. Number of diseases (0-7) | 0.09 * | 0.07 * | 0.02 * |
| p-value | <0.001 | 0.001 | 0.454 |
| Percentages are weighted Differences are tested by the Wald-Chi-square and correlation analyses IADLs= instrumental activities of daily living Comorbidity includes: hypertension, diabetes, coronary heart disease, arthritis, stroke, chronic pulmonary obstructive disease or cancer *Speraman r | |||
In multivariate analyses (Table 3), individuals aged 65 to 69 and 70 to 74 years had higher odds for influenza, pneumococcus, and tetanus vaccination, compared to those between 60-64 years. Older adults with upper class had lower odds for influenza and pneumococcus vaccination, compared to those with lower class. Individuals covered by health insurance (contributive or subsidized) had higher odds (between 3 and 5 times higher) for influenza, pneumococcus and tetanus vaccination, compared to those with no insurance. Older adults with better functional status (higher Lawton scores) had higher odds for influenza, pneumococcus and tetanus vaccinations. Those with higher number of medical conditions (comorbidity) had higher odds for influenza, and pneumococcus vaccinations.
| Characteristics | Influenza | Pneumococci | Tetanus | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||
| Age (years) | ||||||
| 60-64 | 1.00 | 1.00 | 1.00 | |||
| 65-69 | 1.77 (1.22-2.56) | 0.002 | 1.88 (1.34-2.64) | <0.001 | 1.68 (1.17-2.39) | 0.004 |
| 70-74 | 2.04 (1.35-3.07) | <0.001 | 2.10 (1.43-3.08) | <0.001 | 1.63 (1.12-2.36) | 0.009 |
| 75+ | 1.74 (1.15-2.62) | 0.007 | 1.33 (0.95-1.86) | 0.096 | 1.48 (1.03-2.12) | 0.032 |
| Sex | ||||||
| Men | 1.00 | 1.00 | 1.00 | |||
| Women | 1.14 (0.86-1.53) | 0.354 | 1.06 (0.82-1.36) | 0.653 | 0.85 (0.66-1.09) | 0.217 |
| Socio-economic strata | ||||||
| Lower class (1-2) | 1.00 | 1.00 | 1.00 | |||
| Middle class (3-4) | 0.89 (0.67-1.18) | 0.426 | 1.10 (0.85-1.42) | 0.463 | 0.87 (0.67-1.11) | 0.269 |
| Upper class (5-6) | 0.16 (0.08-0.30) | <0.001 | 0.20 (0.10-0.38) | <0.001 | 0.50 (0.24-1.03) | 0.060 |
| Health insurance | ||||||
| Not insured | 1.00 | 1.00 | 1.00 | |||
| Contributive | 3.47 (1.65-7.32) | <0.001 | 4.84 (2.18-10.74) | <0.001 | 4.55 (2.11-9.83) | <0.001 |
| Subsidized | 3.00 (1.39-6.45) | 0.005 | 3.58 (1.60-8.01) | 0.002 | 3.70 (1.69-8.07) | 0.001 |
| Transitory | 3.76 (0.93-15.25) | 0.063 | 5.11 (1.22-21.37) | 0.025 | 3.32 (0.77-14.25) | 0.105 |
| Functional Status. Lawton test (IADLs) | ||||||
| Continuous score (0-8) | 1.13 (1.03-1.23) | 0.010 | 1.08 (1.00-1.17) | 0.048 | 1.11 (1.02-1.20) | 0.012 |
| Comorbidity. Number of diseases (0-7) | 1.23 (1.08-1.39) | 0.002 | 1.16 (1.04-1.30) | 0.007 | 1.02 (0.91-1.14) | 0.691 |
| OR= odds ratios CI= confidence intervals IADLs= instrumental activities of daily living Comorbidity includes: hypertension, diabetes, coronary heart disease, arthritis, stroke, chronic pulmonary obstructive disease or cancer | ||||||
Discussion
Having assessed the coverage of vaccinations in elders living in the city of Bogota and having identified factors that influenced the likelihood of being vaccinated are the most important results of this report.
In the current report the vaccination weighted percentages were 73.0% for influenza, 57.8% for Pneumococci, and 47.6% for tetanus which corresponds, respectively, to a) 569,060, b) 450,571 and c) 371,058 persons aged 60 years and older, living in the city of Bogotá in 2012. Our result on influenza vaccination is comparable to one study in Sao Paulo, Brazil, in 2010, where adults aged 60 and older had a self-reported vaccination of 74.2%23.
Our results could be also comparable, in part, with data from another secondary analysis of a study with similar design to the SABE Bogota, the Latin American SABE Study in 1999-2000, including persons 60 years and older from 6 cities: Bridgetown (Barbados), Montevideo (Uruguay), Buenos Aires (Argentina), Mexico City (Mexico), Sao Paulo (Brazil), and Santiago (Chile). The weighted percentages of influenza vaccine during the previous year and the weighted percentages of tetanus vaccine during the previous 10 years are depicted in Figure 1. Herein, Bogota has higher percentage for influenza vaccine than those cities, except Santiago. However, Bogota has lower percentages for tetanus vaccine compared to Santiago, Sao Paulo and Mexico City 24.
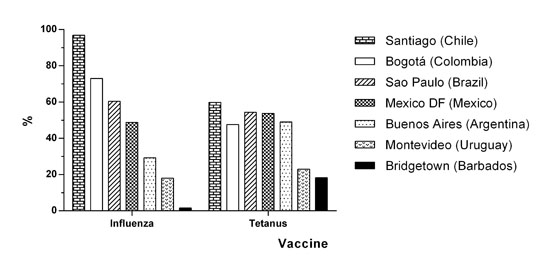
Figure 1. Vaccination for Influenza and Tetanus in Bogota and other cities in Latin America, persons aged 60 years and older. Data are weighted percentages of influenza vaccine during the previous year and tetanus vaccine during the previous 10 years, from the SABE Study in Latin American cities and the SABE Bogota Study.
One study designed to determine vaccination coverage among persons aged 60 and older, done in Mexico by Trejo-Valdivia et al., in 2008, showed that national vaccination coverage for influenza was 56.5%, for pneumococci was 44.3% and for tetanus was 61.8%25. However, that study differs from our study in the following: First, it was designed to specifically determine vaccination coverage (our report is a secondary analysis of the SABE Bogota study which covers multiple health problems and diagnoses), and in addition to self-report they compared the information provided by the elderly with vaccination health records or carnets. Second, the tetanus vaccine question asked if a person had it at 60 years or older (not during the previous 10 years as it was in our study)25.
Our finding that older adults with functional impairments are less likely to have a vaccine is in agreement with a previous report on influenza and tetanus vaccines24. Disabled individuals may have barriers to go on time to the health care settings or to be involved in vaccination campaigns. Thus, disable older adults are important health promotion targets to increase vaccination coverage in Bogota and other cities in Colombia.
In our study, older adults with more comorbidity have greater vaccination for influenza and pneumococci. This finding is in line with previous reports26,27. Indeed, older adults with chronic conditions are more likely to have attended health care settings where additional advice for vaccination may have been provided; especially the direct recommendation by a healthcare provider plays a decisive role in the decision to have a vaccine26,27.
It could be argued that the efforts made by health centers (after the pandemic outbreak of H1N1 in 09), for raising awareness about the importance of vaccination have been successful. However, it would be fair to acknowledge that it also was the result from a long-time work carried out by different academic and social organizations that have historically pursued the same target28. Although the results have been good, they are not sufficient and we are still far from universal coverage for this population. On the other hand, tetanus vaccination has not been sufficiently publicized as compared to the other two vaccines, which could explain the lower coverage of the tetanus vaccine.
Women usually have greater acceptance and better adherence towards preventive programs, but in our study we did not find sex differences29. As expected, individuals with health insurance affiliation had higher coverage of all vaccines, both in the contributive and subsidized category compared to those that reported no affiliation. Interestingly enough, the transition group had the highest prevalence of pneumococcal vaccination, which is not the case for the other vaccines. This finding maybe explained by the extensive free vaccination campaigns for older adults, carried out in the city during the last decade, but still not reaching people without insurance. It is surprising the poor acceptance of these preventive programs in the upper social classes, which would suggest that prevention campaigns have reached more impact in the lower and middle social class. It should be taken into account that the questions related to the pneumococcal vaccine, did not ask about the specific time period of the shot.
Our study has some limitations. First, this is a cross-sectional study. Therefore, causality cannot be determined. Second, selfreported vaccinations are used as the outcome variables, and we did not corroborate the self-report with medical or administrative records, or vaccination carnets. This is not exempt of recall bias (e.g., over reporting), which may lead to analytical bias. Nevertheless, our study has some strength. The design of this study was planned to allow statistical inference for the population aged 60 years and older. Thus, we are reporting weighted frequencies for self-reported vaccination in a representative sample of older adults in the capital city of Colombia, Bogota.
Individuals 65 to 74 years had the highest percentages of vaccination compared with the younger group between 60 to 64 years. Thus, improving public health policies within this younger group of age is a priority, as they showed the lower percentages in vaccination and may have a better response to immunization30.
It is required to combine efforts for educating health personnel, managers responsible for making public health decisions and the general public about the advantages and benefits of immunization of the elderly, especially with the arrival of the herpes zoster vaccine. Public health programs for vaccination are overdue for integrally including older adults in their main goals, with the same benefits currently implemented for the pediatric population, in order to obtain significant consequences of prevention.
Finally, it is necessary to conduct studies aiming at measuring the impact of prevention at the clinical, economic and social level.
Conclusion
Vaccination campaigns should be strengthened to increase vaccination coverage, especially in the group more reticent to vaccination or vulnerable to reach it such as the disable elder.
Acknowledgements:
The authors thank Dr. Rafael Samper-Ternent for his suggestions and valuable discussions on this Project.
Founding:
This study was supported by grants from the Administrative Department of Science, Technology and Innovation - Colciencias, Code 120354531692 and the Pontificia Universidad Javeriana, Code 00005005.
Conflict of Interest:
The authors declare no conflicts of interest.
References
1. Canning D. The causes and consequences of demographic transition. Population studies. 2011; 65(3): 353-61. [ Links ]
2. Lee R. The demographic transition: Three centuries of fundamental change. J Economic Perspectives. 2003; 17(4): 167-90. [ Links ]
3. Burns EA, Goodwin JS. Immunodeficiency of aging. Drugs Aging. 1997; 11(5): 374-97. [ Links ]
4. Cano C. Programas de vacunación en el adulto mayor. Prevención en geriatría II Curso de la Academía Latinoamericana de Medicina del Adulto Mayor. ALMA: CIEDESS; 2011. [ Links ]
5. CDC Recommended adult immunization schedule-United States, 2013. J Midwifery Women’s Health. 2013; 58(2): 215-20. [ Links ]
6. CDC. National early season Flu vaccination coverage. 2012 Available from: http://www.cdc.gov/flu/fluvaxview/nifs-estimatesnov2012.htm. Accessed: 12 June 2014. [ Links ]
7. Bader MS. Immunization for the elderly. Am J Med Sci. 2007; 334(6): 481-6. [ Links ]
8. Constenla DO. Economic impact of pneumococcal conjugate vaccination in Brazil, Chile, and Uruguay. Rev Panam Salud Publica. 2008; 24(2): 101-12. [ Links ]
9. Vinogradova Y, Hippisley-Cox J, Coupland C. Identification of new risk factors for pneumonia: population-based case-control study. Br J Gen Pract. 2009; 59(567): e329-38. [ Links ]
10. Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003; 289(2): 179-86. [ Links ]
11. Ministerio De La Protección Social Colombia. Análisis de la situación de salud en Colombia (2002-2007), Morbilidad y Mortalidad. Universidad de Antioquia, 2007. [ Links ]
12. CDC. Pneumococcal disease. In: W. Atkinson, Hamborsky J, Wolfe S. (Eds.) Epidemiology and Prevention of Vaccine-Preventable Diseases. 12th ed. 2012: 233-48. [ Links ]
13. Jackson LA, Neuzil KM, Yu O, Benson P, Barlow WE, Adams AL, et al. Effectiveness of pneumococcal polysaccharide vaccine in older adults. New Engl J Med. 2003; 348(18): 1747-55. [ Links ]
14. Kretsinger K, Broder KR, Cortese MM, Joyce MP, Ortega-Sanchez I, Lee GM, et al. Preventing tetanus, diphtheria, and pertussis among adultsuse of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine recommendations of the Advisory Committee on Immunization Practices (ACIP) and recommendation of ACIP, supported by the Healthcare Infection Control Practices Advisory Committee (HICPAC), for use of Tdap among health-care personnel. MMWR Recomm Rep. 2006; 55(RR-17): 1-37. [ Links ]
15. Arango D. Tétanos ¡Todavía un Problema de Salud Pùblica!. Iatreia. 2008; 21(2): 186-98. [ Links ]
16. Velandia M. Instituto Nacional de Salud. Comunicación personal. 2003. [ Links ]
17. DANE. Population projections of Bogotá and the major demographic indicators 2005-2020. Based on data from the 2005 National Population Census. 2005. [ Links ]
18. DANE. En el día de las personas de edad, entrega balance de población mayor Bogotá: Alcaldía Mayor de Bogotá. 2011. http://www.bogota.gov.co/article/planeacion/en%20el%20dia%20internacional%20de%20las%20personas%20de%20edad,%20bogota%20entrega%20balance%20de%20poblacion%20mayor. [ Links ]
19. Chavarro-Carvajal D, Reyes-Ortiz C, Samper-Ternent R, Arciniegas AJ, Cano-Gutierrez C. Nutritional assessment and factors associated to malnutrition in older adults: A cross-sectional study in Bogota, Colombia. J Aging Health. 2015; 27(2): 304-19. [ Links ]
20. Peláez M, Palloni A, Albala C, Alfonso J, Ham-Chande R, Hennis A. SABE - Encuesta Salud, Bienestar y Envejecimiento. 2004. Available from: http://www.ssc.wisc.edu/sabe/docs/informeFinal%20EspaNol%20noviembre%202004.pdf. [ Links ]
21. Congreso Republica de Colombia. Ley 142. Por la cual se establece el régimen de los servicios públicos domiciliarios y se dictan otras disposiciones, Artículo 102. Estratos y Metodologia. 1994. [ Links ]
22. Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist, 1969; 9: 179-86. [ Links ]
23. Sato AP, Antunes JL, Moura RF, de Andrade FB, Duarte YA, Lebrao ML. Factors associated to vaccination against influenza among elderly in a large Brazilian metropolis. PloS One. 2015; 10(4): e0123840. [ Links ]
24. Reyes-Ortiz CA, Davalos DM, Montoya MF, Escobar D. Access to vaccines for Latin American and Caribbean older adults with disability In: Angel JL, Torres-Gil F, Markides K (Eds); Aging, Health and Longevity in the Mexican-Origin Population. New York: Springer. 2012;159-171. [ Links ]
25. Trejo-Valdivia B, Mendoza-Alvarado LR, Palma-Coca O, Hernández-Ávila M, Téllez-Rojo Solís MM. Encuesta Nacional de Cobertura de Vacunación (influenza, neumococo y tétanos) en adultos mayores de 60 años en México. Salud Pública Méx. 2012; 54: 39-46. [ Links ]
26. Andrew MK, McNeil S, Merry H, Rockwood K. Rates of influenza vaccination in older adults and factors associated with vaccine use: a secondary analysis of the Canadian Study of Health and Aging. BMC Public Health. 2004; 4(36): 24-37. [ Links ]
27. Kohlhammer Y, Schnoor M, Schwartz M, Raspe H, Schäfer T. Determinants of influenza and pneumococcal vaccination in elderly people: a systematic review. Public Health. 2007; 121(10): 742-51. [ Links ]
28. Teitelbaum MA, Edmunds M. Immunization and vaccine-preventable illness, United States, 1992 to 1997. Stat Bull Metrop Insur Co. 1999; 80(2): 13-20. [ Links ]
29. Leslie LA, Swider SM. Changing factors and changing needs in women’s health care. Nurs Clin North Am. 1986; 21(1): 111-23. [ Links ]
30. Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006; 333(7581): 1241. [ Links ]














