Remark
| 1) Why was this study conducted? |
| It was conducted to understand the scenario of HIV prevention among men who have sex with men. |
| 2) What were the most relevant results of the study? |
| The amount of productions on the subject, the historical construction of prevention methods, the most used methods, as well as the main barriers and facilitators of access to HIV prevention strategies. |
| 3) What do these results contribute? |
| These results contribute to know that there is a great concentration of research in some strategies, and that one of the greatest barriers is still stigma. It was also possible to realize that the presence of support or care networks serves as facilitators in their presence or barriers in their absence. |
Introduction
In the history of the human immunodeficiency virus (HIV) epidemic, it is possible to observe that certain social segments were more affected than others. In particular, homosexuals and men who have sex with men (MSM), sex workers (SW), transgender people, people who inject drugs (PID) and people in prison or under seclusion of another kind. These segments have been designated by the World Health Organization (WHO) as "key population" 1, since they are strategic to achieve greater control of the epidemic in the world.
Research has shown that HIV prevalence in these populations is much higher than in the general population. For example, MSM have an HIV prevalence of between 6.1 and 6.6% in Europe and more than 25.4% in the Caribbean region 2 and 18.4% in Brazil 3. Moreover, recent data show a continuous progress of the epidemic in these populations, even in regions that had already registered a decrease in incidence rates in these social segments 1.
With the emergence of the so-called "multiple prevention strategies" or "combined prevention" 4, the current HIV prevention scenario is marked by increasing optimism 5,6 in which combined prevention represents an increase in prevention possibilities in different situations that present a potential risk of HIV infection. However, a key question has been raised for managers, health professionals and researchers: how to articulate, within the framework of prevention, the joint provision of new prevention strategies, including antiretrovirals, more traditional strategies, psychosocial and behavioural interventions, and structural interventions 4-7 (Table 1).
Table 1 Classification of prevention strategies and methods for thematic synthesis.
| Types of prevention | Strategies and methods |
|---|---|
| Use of antiretrovirals | Treatment as Prevention (TP); Pre-Exposure Prophylaxis (PrEP); Post-Exposure Prophylaxis (PEP) |
| Traditionals | Condoms; HIV Diagnostic Tests |
| Psychosocial and behavioural interventions | Conformation of Support Groups; Peers education |
| Structural interventions | Reduction of stigma and social inequalities |
Considering combined prevention, the Pan American Health Organization (PAHO) recommends several actions for key populations in Latin America and the Caribbean: diagnostic tests, counselling, diagnosis and treatment of sexually transmitted infections (STIs), pre-exposure prophylaxis (PrEP), post-exposure prophylaxis (PEP), condoms and lubricants, antiretroviral treatment (ART) for HIV-positive people, peer education and sexual information and education. Among these, pharmacological interventions have the lowest coverage in the countries of the region, where ART is offered in 45% of countries, PEP in 39% and PrEP in only 6% of them 7.
Considering the aspects that lead MSM to be more exposed to HIV infection, having greater difficulties in accessing supplies and services and being a victim of stigma and homophobia stand out. Given this, to advance policies to combat the epidemic, a better understanding of these issues is required 8-10 with the consequent incorporation and management of new prevention methods and strategies.
The literature of studies with a qualitative methodological approach has sought to understand the dynamics of the use of preventive methods and strategies in MSM in recent decades. Research has considered different contexts including affective-sexual relationships and government community interventions. They have also studied the meanings and experiences of MSM related to risk and prevention, as well as to access and use of health services 11,12.
Systematic review is an important technology for evaluation of evidence-based scientific policies and practices. Systematic review studies use rigorous and explicit methods to gather the results of primary research providing reliable answers to specific questions 13. This manuscript is part of this type of study. The thematic synthesis, chosen among other types of synthesis for qualitative studies, consists in identifying the important or recurring themes in the primary empirical studies. Each of these topics is presented in a structured way so that synthesis and interpretations of each point can be extracted and then articulated with each other. The thematic synthesis seeks to increase the transparency and reliability of the topics, by grouping the studies according to their characteristics, with the quantification of the qualitative results and, mainly, by compiling the findings according to the relevant and recurring issues 13,14.
The construction of a critical view of the scientific production on the proposed aspect provides a deeper understanding of how preventive actions have been incorporated in the MSM population during the years of the epidemic, and about the challenges to consolidate a new HIV prevention scenario that incorporates recently developed methods and strategies for this segment of the population. In this way, this article aims to make a thematic synthesis of the scientific productions that use the qualitative methodology in the field of HIV prevention methods and strategies among MSM.
Materials and Methods
Thematic synthesis 13-15 was performed using references from the ENTREQ protocol 16 and, when necessary from the PRISMA 17, Cochrane 18 and New York University protocols 19. Studies published in English, Spanish and Portuguese were included, which were found in six databases of information sources: Medline, Embase, SciELO, Scopus, Bireme and Web of Science.
Studies that used empirical material in the analysis of HIV prevention methods and strategies, and qualitative data production techniques such as narratives, in-depth interviews, focus groups, direct observations, etc, were included in the review. The participants belonged to the MSM population, and in some studies, there were participants from other populations such as transsexuals and psychoactive substances users. The documents were not excluded by geographical location or year of publication, however, studies conducted exclusively with children and adolescents or that have analyzed occupational exposure or sexual violence were excluded.
Publications were searched using search directories in the information source databases. Using the keywords or the best search terms, such as "Men who have sex with men", "Bisexual *", "Prevention and control", a specific search directory was created for each database. The asterisk symbol (*) allowed to include in the search numerous possible endings of the radicals sought and, therefore, cover the full range of possible terminations in the databases.
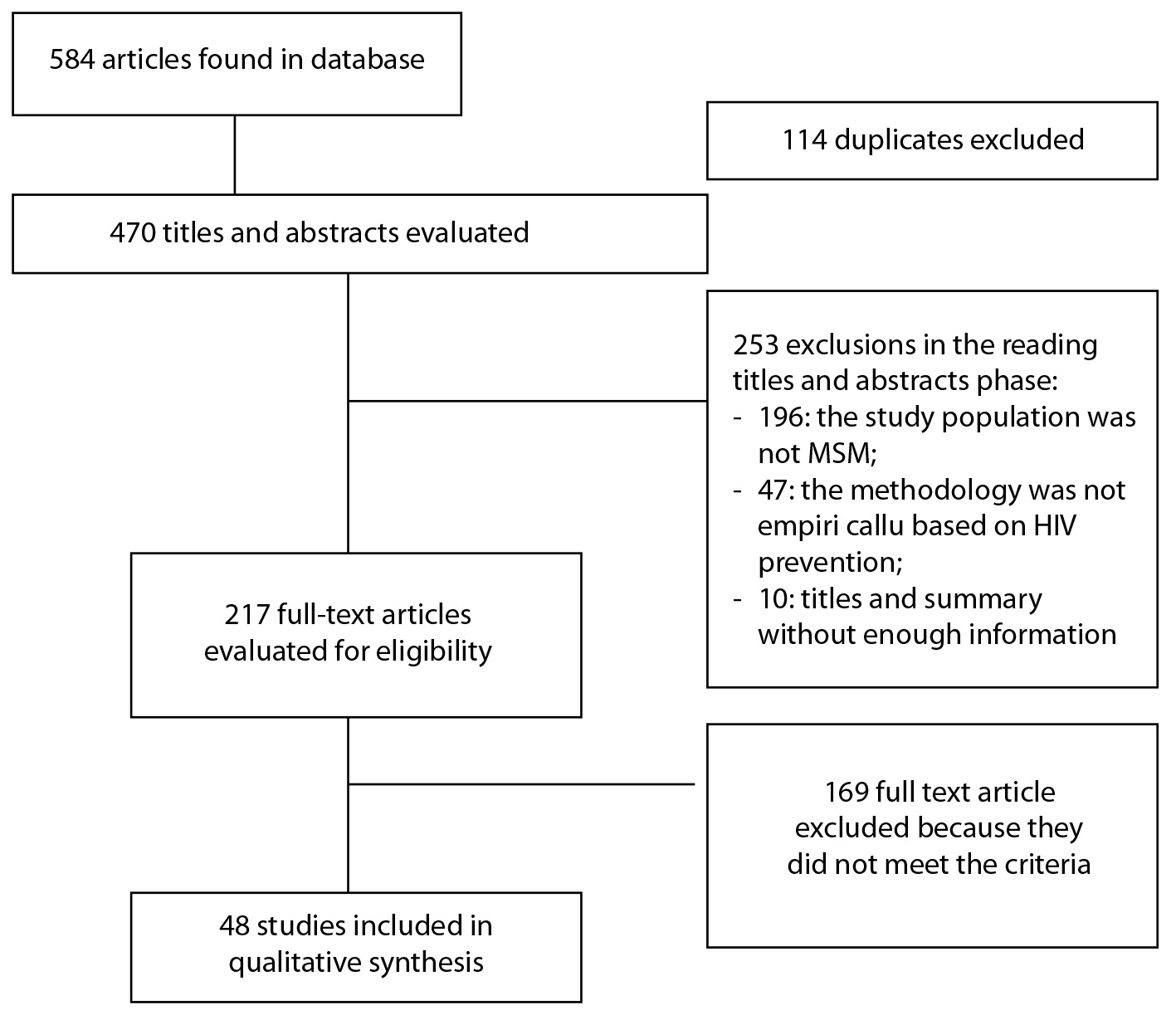
The searches in the databases were completed in January 2018 and the articles found were managed with the EndNote® reference manager and with spreadsheets. Information about authorship, year of publication, original title, study location, population studied, methodological approach used and summary in the original language were extracted from the publications. Subsequently, the works were selected using the following procedures performed sequentially: a) elimination of duplicates; b) evaluation of titles and abstracts; c) complete reading of the documents. The final selection of the studies included in the review was made in accordance with the guidelines and recommendations of the protocols mentioned above. For this selection, two independent and experienced investigators read the titles and abstracts, and when there was disagreement, and in order to decide, they used the arbitration of a third investigator.
Results
584 articles were identified, of which 114 (19.5%) were duplicated and 253 (43.3%) were discarded because they did not correspond to the MSM segment (196; 33.6%), did not use empirical data (47; 8.0%) and presented insufficient information or unclear information in the title or summary (10; 1.7%). In total, 217 (37.1%) articles were completely read and, of these, 169 (28.9%) were discarded for not complying with the inclusion criteria. Finally, 48 articles (8.2%) were selected and included for the analysis (Fig. 1).
The results are presented at two different times: the first is a demonstration of the general characteristics of the 48 selected studies and the second is the compilation of the most relevant and recurring themes of the analyzed production. Of the 48 selected studies for this synthesis, 24 (50%) were conducted in North America (mainly the United States) 20-43, eight (16.7%) in Europe 44-51, five (10.4%) in Africa 52-56, four (8.3%) in Oceania 57-60, four (8.3%) in South and Central America 61-64 and three (6.2%) in Asia 65-67 (Table 2).
Table 2 Distribution of selected articles by continent.
| Región | References |
|---|---|
| North America | Beougher et al., 201420; Bird et al., 201721; Mitchell et al., 201623, 201722; Brooks et al., 201124, Nanin et al., 200925; Storholm et al., 201726; Taylor et al., 201427; 2012 28; Campbell et al., 201429; Hojilla et al., 201630; Collins et al., 201731; Grov et al., 201332; Elwood et al., 200333; Grace et al., 201435, 201834; Mimiaga et al., 201436; Hoff et al., 201537; Holloway et al., 201738; Holmes et al., 200839; Hussen et al.., 201340; Martinez et al., 201641, 201742; Medline et al., 201743 |
| Europe | Bil et al., 201644; Boydell et al. 201745; Gredig et al., 201646; Grov, 201747; Middelthon, 200148; Sayer et al., 200949; Witzel et al., 201750; Young et al., 201651 |
| Africa | Lee et al., 201752; Maina et al., 201853; Siegler et al., 201554; Taegtmeyer et al., 201355; Wagner et al., 201256 |
| Oceania | Körner et al., 2005a57, 2005b59, 200658; Neville et al., 201660 |
| South and Central America | Blas et al., 201361; Gonzales et al., 201262; Logie et al., 201763; Reisen et al., 201464 |
| Asia | Bourne et al., 201765; Newman et al., 201366; Wei et al., 201467 |
It is worth noting that there are no studies conducted in Africa and South America that evaluate preventive methods based on the use of antiretrovirals (ARV), such as PEP, PrEP and treatment as prevention (TP), although the countries of those regions have already incorporated these methods.
Of the 48 studies previously mentioned, 38 dealt exclusively with the population of MSM without HIV, and of these, eight studies included ethnic markers 25,29,33,38,40,42,43,52 and three of them included generational markers 26,45,48. Four other studies included populations of MSM and HIV-positive people within the dynamics of serodiscordant relationships. The remaining six studies included, in addition to the MSM population, other populations, such as transgender women, drug users and heterosexual women (Table 3).
Table 3 Studies’ population.
| Population | References |
|---|---|
| MSM without HIV | Beougher et al 201420; Bird et al 201721; Grov et al 201332, 201747; Holmes et al 200839; Taylor et al 201427; Brooks et al 201228; Collins et al 201731; Grace et al 201834, 201435; Bil et al 201644; Gredig et al 201646; ; Sayer et al 200949; Witzel et al 201750; Maina et al 201853; Siegler et al 201554; Taegtmeyer et al 201355; Wagner et al 201256; Körner et al., 2005a57, 2005b59, 200658; Neville et al., 201660; Blas et al 201361; Gonzales et al 201262; Reisen et al 201464; Bourne et al 201765; Wei et al 201467; Holloway et al 201738; Hussen et al 201340; Martinez et al 201742; Medline et al 201743; Nanin et al 200925; Campbell et al 201429; Elwood et al 200333; Lee et al 201752; Storholm et al 201726; Boydell et al 201745; Middelthon et al 200148 |
| MSM and HIV-positive patients | Mitchell et al 201722, 201623; Brooks et al 201124; Hoff et al 201537 |
| MSM and transgender women | Hojilla et al 201630; Martinez et al 201641; Logie et al 201763; Newman et al 201366 |
| MSM and drug users | Mimiaga et al 201436 |
| MSM and heterosexual women | Young et al 201651 |
In the set of studies, seven methods and strategies for the prevention of HIV infection were addressed, with a predominance of PrEP, PEP, condoms, diagnostic tests, behavioural strategies, and treatments such as prevention and circumcision. Of the above, three are methods based on ARV (PEP, PrEP, treatment as prevention). An eighth group was defined as "others", which included the only article 66 that did not fall into any of the previous seven categories, related to the introduction of a microbicidal gel in a population of MSM and transsexuals in Thailand. There is a predominance of studies on PrEP (16 studies), published mainly in 2010, the period that coincides with the launch of the first results of safety and efficacy of the method 68. In four of them, PrEP is analyzed together with other strategies 37,41,47,51.
Thirteen studies addressed the HIV test strategy, one of which appears along with the TP strategy 67 and another with the condom 56. Also notable is the number of studies involving diagnostic tests in the last five years, five of them published in 2017 22,43,45,50,63.
Ten studies addressed the behavioural and psychosocial interventions approach as a prevention strategy, which includes strategies for risk reduction, such as agreements with sexual partners and social protection, in addition to the use of a prevention method. These studies have gained prominence in the last ten years, and six of them 21,38,41,42,47,53 have been published as of 2016. This suggests that, in parallel to the research focused on preventive methods, there is a concern to understand other dimensions of prevention that have more to do with different experiences and needs of the individuals.
The condom, considered the prevention method with the greatest investment in public health and in the homosexual community, has remained the researchers’ focus of attention over the years, gathering nine articles. It is noteworthy that the first study included in the analysis was published in 2001.
PEP, in turn, appears in four studies, the first being published in 2005 and the last in 2009. Although PEP is the oldest method among those using ARV and has been widely studied by quantitative approaches 69-74, qualitative research has a limited number for the MSM population.
TP appears tangentially in three studies and only one study addressed circumcision. The low interest in the issue of circumcision in the MSM population might be related to the low effectiveness of the method in male sexual intercourse or penetrating anal practices 75-77. Detailed information about the studies is found in Table 4.
Table 4 Methods and strategies for the prevention of HIV infection.
| Prevention methods | References |
|---|---|
| PrEP | Mitchell et al 201623; Brooks et al 201124, 201228; Storholm et al 201726; Taylor et al 201427; Hojilla et al 201630; Collins et al 201731; Grace et al 201834; Mimiaga et al 201436; Hoff et al 201537; Martinez et al 201742; Bil et al 201644; Gredig et al 201646; Grov 201747; Witzel et al 201750; Bourne et al 201765 |
| Diagnostic tests | Beougher et al 201420; Mitchell et al 201722; Nanin et al 200925; Hussen et al 201340; Medline et al 201743; Boydell et al 201745; Witzel et al 201750; Siegler et al 201554; Wagner et al 201256; Blas et al 201361; Logie et al 201763; Reisen et al 201464; Wei et al 201467. |
| Behavioural strategies | Bird et al 201721; Campbell et al 201429; Grace et al 201435; Holloway et al 201738; Holmes et al 201839; Martinez et al 201641; 201742; Grov 201747; Maina et al 201853; Taegtmeyer et al 201355 |
| Condoms | Campbell et al 201429; Grov et al 201332; Elwood et al 200333; Hoff et al 201537; Grov 201747; Middelthon et al 200148; Lee et al 201752; Wagner et al 201256; Neville et al 201660. |
| PEP | Sayer et al 200949; Körner et al., 2005a57, 2005b59, 200658. |
| Treatment as prevention | Grov 201747; Young et al 201651; Wei et al 201467 |
| Circumcision | Gonzales et al 201262 |
Table 5 presents the chronology of the study publications according to prevention methods. Studies published until 2006 focused on condoms 33,48 and PEP 57,59. As of this period, there is a diversification of production, which coincides with the start of studies related to diagnostic tests and PrEP 23,26,27,30,31,34,36,37,41,44,46,51,65. Furthermore, behavioural and psychosocial studies increase 21,29,35,38,39,41,42,47,53,55, which suggests a greater influence of the "combined prevention" paradigm 78.
Table 5 Chronology of publications of selected studies until January 2018.
| More than 10 years ago | 2001 | 2003 | 2005 | 2006 | |||
| Condom and Diagnostic Tests 48 | Condom 33 | PEP57,59 | PEP58 | ||||
| From 10 to 5 years ago | 2008 | 2009 | 2011 | 2012 | 2013 | ||
| Behavioral and Psychosocial 39 | Diagnostic tests 25 | PrEP24 | PrEP28 | Diagnostic tests 40,61 | |||
| PEP49 | Circumcision 62 | Condom 32 | |||||
| Condom and Diagnostic Tests 56 | Others 66 | ||||||
| Behavioral and Psychosocial 55 | |||||||
| From 5 years ago | 2014 | 2015 | 2016 | 2017 | 2018 | ||
| Diagnostic tests 20,64 | Condom and PrEP37 | PrEP23,30,44,46 | Behavioral and Psychosocial 21,42 | PrEP34 | |||
| Behavioral and Psychosocial 35 | Diagnostic tests 54 | PrEP and Behavioural and Psychosocial 41 | PrEP26,31,65 | Behavioural and Psychosocial 53 | |||
| PrEP27,36 | Condom 60 | Diagnostic tests 22,43,45,50,63 | |||||
| Diagnostic tests and TP67 | PrEP and TP51 | Condom, Behavioral and Psychosocial y PrEP 47 | |||||
| Behavioral and Psychosocial, Condom, Diagnostic tests 29 | Behavioral and Psychosocial and Others 38 | ||||||
| Condom and others 52 |
Issues related to the production of PrEP, diagnostic tests, condom and behavior strategy
For the thematic analysis of the production that was considered, we limited ourselves to the methods and strategies that stood out according to number of publications (42 out of the 48 productions analyzed), namely: PrEP, diagnostic tests, condoms and prevention strategies with behavioural and psychosocial interventions. The analysis of these issues was based on the perspective of combined prevention.
In turn, combined prevention has been recurring in numerous studies and manuals on HIV prevention published by governments or multilateral agencies 78-83. This approach has been used to reflect the possibilities that can be combined, not only in the sense of grouping, but also when referring to the notion of dialogue and agreement in order to cover the widest possible range of protection against HIV. In this model, prevention strategies based on the promotion of the use of preventive methods and behavioural and psychosocial interventions are articulated with structural interventions, in the form of public policies and legal frameworks. This approach has preferably targeted key populations 79,82,83.
The main topics discussed in the studies on the four prevention methods were: support networks, care networks and stigma, followed by the financial cost of access to PrEP and the fear of a positive HIV test result (Table 6).
Table 6 Main topics discussed in the studies.
| Main topics | References |
|---|---|
| Service networks | Mitchell et al 201722; Nanin et al 200925; Hojilla et al 201630; Elwood et al 200333; Grace et al 201435; Hussen et al 201340; Martinez et al 201742; Boydell et al 201745; Witzel et al 201750; Blas et al 201361; Logie et al 201763; Reisen et al 201464; Bourne et al 201765 |
| Support networks | Hojilla et al 201630; Elwood et al 200333; Holloway et al 201738; Martinez et al 201641; 201742; Boydell et al 201745; Grov 201747; Maina et al 201853; Taegtmeyer et al 201355; Logie et al 201763; Reisen et al 201464; Wei et al 201467 |
| Stigma | Nanin et al 200925; Storholm et al 201726; Collins et al 201731; Grace et al 201834; Mimiaga et al 201436; Hussen et al 201340; Martinez et al 201641; Medline et al 201743; Grov 201747; Young et al 201651; Maina et al 201853; Taegtmeyer et al 201355; Wagner et al 201256, Blas et al 201361; Logie et al 201763; Reisen et al 201464; Bourne et al 201765; Wei et al 201467. |
In the studies the service networks 84-86 have been defined as formalized services that provide care, guidance and education to the direct users served or their surroundings. The deficiency or absence of these networks is highlighted in the studies as an important barrier to prevention.
The highest frequency of studies that address the care network occurs in the analysis of diagnostic tests, PrEP, behavioural and psychosocial strategies and the condom. They also appear in papers that discuss the combination of two or more prevention methods 29,47,52. Among the 16 studies that address this issue, six 25,40,47,61,64,67 highlight different aspects that characterize the barriers observed within the care networks, such as: stigma, fear, insecurity regarding the use and lack of preparation, the services to attend the participants and the promotion of the methods. The studies report that the communication strategies that positively influence the adoption of certain methods are the facilitators of access to the care networks, and that is how the studies dealing with support networks use different theoretical approaches to support the topic. Regarding this specificity, the analyzed production converges by highlighting the support network as an important facilitator for the adoption of different prevention methods, being a strategy with high potential to promote the use of preventive methods 87-89.
We found 12 studies that had an approach based on the perspective of support networks. Of particular interest are the studies that addressed the combination of two or more prevention methods, behavioural and psychosocial strategies, diagnostic tests, PrEP and condoms. In half of them, barriers similar to those found in everything related to care networks were observed. As a facilitator of access to methods in support networks, social and educational information policies appeared to combat stigma and prejudice.
Stigma is addressed in a multifaceted manner in the 18 documents that investigated the issue. Most of these studies were related to the stigma of discovering HIV infection, homophobia, and especially, with studies that addressed behavioural diagnostic strategies and tests. Regarding the diagnostic tests, the lack of preparation of the health service to adequately receive the MSM population is highlighted 25,52,63,64. Another form that arises in studies that address stigma is the endogenous one 31,34,36,65, where the MSM community imposes sexual morality and rejects individuals who deviate from that morality. This discussion is linked to the use of PrEP, since some labels such as “promiscuity” are used to name the users of methods in certain MSM communities. Of these studies, only one 26 highlights a reduction in HIV-associated stigma in MSM who use PrEP.
Studies that address the financial cost of one or more prevention methods, particularly PrEP, show the excessive cost for potential users in countries where one or more methods are not offered free of charge through public health policies, hindering the continuous and consistent access and use 23,24,27,34,37,44,46,47,63,67. In turn, the fear associated with a possible diagnosis of HIV infection appears as a barrier to the access to diagnostic tests 25,40,43,56,61,63,64,67. It is important to note that the results of the studies that address the diagnostic tests and the cost of the methods vary according to the structures, care networks and free services in the different countries or places where the studies are conducted.
Final considerations
Our thematic synthesis presented a critical view of the qualitative approach studies on HIV prevention in the MSM segment, highlighting the production characteristics in terms of time and geographic distribution, according to the prevention strategies and methods incorporated in the studies. The most frequent topics that were prioritized in the studies that dealt with PrEP, diagnostic tests, condoms and behavioural and psychological prevention strategies were highlighted. Our study highlighted the relevance of the efforts being made to reduce HIV exposure among the MSM segment, in the current context of the combined prevention strategy, whose challenge is to articulate the supply and joint promotion of prevention strategies and methods.
Regarding the characteristics of the 48 productions analyzed, studies in the northern countries, particularly in the United States and Europe, predominated. Most of the research was conducted exclusively with the MSM population, and there has been a tendency to increase production as of 2011, especially studies that articulate more than one prevention method or strategy. These data seem to reflect the emergence and diffusion of the combined prevention perspective promoted by international agencies such as WHO 78,80 and PAHO 7.
Considering that we are at the end of the fourth decade of the HIV epidemic and acquired immunodeficiency syndrome (AIDS), and that studies and interventions with the MSM population have been prominent since the beginning of the epidemic, it is important to note that in the first two decades of the epidemic there was scarce research for this specific segment of the population, with emphasis on prevention and with a qualitative methodological approach. A first observation is the possibility that in the first decades of the epidemic, the MSM segment was investigated on issues related to social representations of risk and living with HIV-positive people, interaction with antiretroviral drugs, the impact of the virus and stigma of AIDS in everyday life, sociability and sexual pleasure of these individuals 90,91. Secondly, and according to the production analyzed, the growth of qualitative studies on prevention methods and strategies among MSM, corresponds, in terms of temporal and geographical distribution, to the emergence of the availability of multiple methods and strategies, and to their combined actions, as a predominant method additional to condom use. As shown in this review, ARV-based methods represent a higher production in recent years. Researchers and funding agencies are interested in investigating the decision making of MSM using such methods, the meanings of the experience of use and the subjective factors related to their effectiveness 47,52,63.
In this sense, PrEP emerges as a method with great potential for prevention among the methods that use ARV and explains the significant number of publications that address the problems and the relevant criticisms to access and use, both individually and in public health, especially as of 2012. The work of Young et al. 51, brings among its findings illustrative questions to think about the criticisms of PrEP, such as the one that argues that it has a great impact on public budgets. The highlights of the PrEP studies in recent years seem to derive from the relationship between different but related aspects, such as the studies linked to research that seek to deepen unanswered questions through clinical and epidemiological studies, such as the acceptability and the possibility of daily use, among others.
The emergence of methods based on antiretrovirals opens a wide area of interest, by changing the preventive approach and the potential impact on the epidemic, thus constituting a relevant field of study. Finally, the development and penetration of qualitative methodological designs in health studies, whether in mixed designs (qualitative and quantitative) or in studies that only produce qualitative data, is growing and consistent. Considering the initial studies on the relationship between HIV/AIDS and the MSM population, studies on combined prevention in this population have access to the experience developed in previous decades.
Observing the main issues addressed in the studies on the four most important methods in analyzed in this review (PrEP, diagnostic tests, condoms and behavioural and psychological prevention strategies), the themes of support and care networks and the stigma are highlighted. Unlike the first two, stigma remains central, constituting a broad social phenomenon in the field of HIV that manifests itself in multiple fields, from those related to private life to those related to the search for services and access to prevention strategies.
In summary, this review points out the limits and possibilities of HIV prevention among MSM as a segment immersed in social constructions and structural contexts that expand their historically known primary vulnerabilities, giving the possibility to discuss, understand, access and use different strategies. Prevention is conditioned by issues such as the access and the cost of health, family and generational problems, as well as possible actions to exclude the State, backed by institutionalized and prevalent stigma and by homophobia in societies 92.
Finally, we consider that the incorporation and development of qualitative research in the field of knowledge production and practices in the prevention of HIV infection is of great importance. As the kind of research that addresses the individualities and subjectivities of human beings and collectivities, this methodological approach can be proposed to study HIV, giving importance, for example, to the ways in which individuals assess the risk of HIV, the forms to address AIDS stigma, how new prevention technologies based on the use of ARVs influence the construction of sexual identities and sexual practices, etc. Furthermore, qualitative research is a tool to recognize the different subjectivities of people in policies to address the epidemic and thus give these individuals the status of rights subjects. Given this, and considering the growing number of qualitative studies on HIV prevention in the MSM segment, the thematic synthesis review points to the state of production technique, pointing out knowledge gaps that deserve research, especially in the current scenario of prevention, and highlighting ways of social response and policies to reduce the risk of infection in this segment of the population historically affected by the epidemic.
The main limitation to construct this thematic synthesis was the restriction of the databases of sources of health information used to select the primary studies. These bases did not necessarily include works from other areas of knowledge such as psychology, sociology and anthropology. The productions of the so-called “gray literature” published outside conventional editorial channels such as reports, thesis, conference proceedings, technical standards, among others, were not part of these databases either.











 texto en
texto en