Remark
| 1)Why was this study conducted? |
| This article was written because after 20 years, extreme maternal morbidity has not been used in Latin America as a tracer event for the quality of obstetric care. Efforts have focused on defining the event and unifying the criteria for the identification of the pregnant woman who has an extreme maternal morbidity. |
| 2) What were the most relevant results of the study? |
| The article offers a review of the history of the event, since it was described by Dr. Say of the WHO, the changes over time and describes the difficulties for its proper use, which allow, from its analysis, to identify actions effective aimed at reducing maternal mortality. |
| 3) What do these results contribute? |
| This publication proposes for the first time in the literature to focus the analysis of the event on the quality and safety of care, using a novel methodology for those who perform epidemiological surveillance of the event, based on the organizational model of causality of errors and adverse events. In addition, it recommends the criteria that, according to the evidence, are the most appropriate to identify a pregnant woman with extreme maternal morbidity. |
The purpose of this article is to analyze critical aspects that have had an impact on the implementation of epidemiological surveillance of extreme maternal morbidity as a quality tracer event of maternal care at population and institutional level. And to generate a proposal that optimizes the utility of this public health event for the prevention of maternal mortality in Latin America.
Extreme maternal morbidity arose more than 20 years ago. It is defined by the World Health Organization (WHO) as any condition that threatens or puts at risk the life of a pregnant woman. Therefore, those pregnant women who survive serious health complications and who had a high probability of dying are classified under this term 1. According to the criteria used for its diagnosis in low-income countries, and due to their heterogeneity, publications on this topic report different frequencies of the occurrence of the event, ranging from 0.04 to 14.9% 2,3.
Due to the relevance of this event in medical practice and its impact on health prevention at Latin American level, the Latin American Federation of Obstetrics and Gynecology (FLASOG) decided, in 2007, to take advantage of what the WHO called "maternal near miss", and adopted the term extreme maternal morbidity to include all women who have a serious complication during pregnancy, childbirth or the puerperium that are life-threatening and require immediate attention in order to avoid death. Since then, the monitoring and surveillance of the extreme maternal morbidity has been considered by international cooperation agencies as a key strategy to reduce maternal mortality 4.
Usually, maternal mortality has been monitored as the quality tracer event of obstetric care, and its analysis allows interventions to avoid maternal death 5. However, by 2015, very few countries managed to meet the goals established in the Millennium Development Goals, especially MDG 5 - improve maternal health 6. Today it is observed that the maternal mortality rate is quite heterogeneous, from 1 case per 100,000 live births in developed countries to more than 100 cases per 100,000 live births in developing countries 7. For this reason, there are required complementary strategies such as surveillance of the extreme maternal morbidity, in order to advance towards the achievement of the Sustainable Development Goals set for the year 2030, regarding the reduction of maternal mortality 8.
The importance of extreme maternal morbidity as a quality tracer event is that, unlike what is observed with maternal mortality, it is an event that occurs more frequently and is anticipatory of death, and in which the surviving pregnant woman is the primary source of information. Likewise, its analysis offers a more effective alternative to identify and implement interventions that allow us to prevent mortality and strengthen the quality of obstetric care, based on more reliable information and without expecting maternal death to occur 1,4,9.
One of the great difficulties of using maternal mortality as a quality tracer is that in health institutions where few births are attended, the probability of the occurrence of a maternal death is low. Therefore, it can generate the erroneous perception that safety conditions and clinical quality of obstetric care are optimal. Indeed, in these scenarios is that an appropriate surveillance and monitoring of the extreme maternal morbidity becomes relevant 10.
Research carried out both worldwide and in Latin America estimates that between 12 and 14 cases of extreme maternal morbidity occur for each maternal death 4. This means the event may actually occur, even in institutions with few births. This favors that from surveillance and follow-up of cases of extreme maternal morbidity, it is possible to generate comprehensive action plans and prevent maternal deaths. Additionally, one of the advantages of analyzing extreme maternal morbidity cases is that, unlike maternal deaths, where there is always the stigma and pressure of lawsuits, the event is less threatening for health service providers, because the survivor women are the primary source of information. This makes the analyses more equitable, closer to reality, and that the lessons learned be more useful in order to intervene and generate more effective actions to prevent maternal mortality 11. In contrast to the analyses based on maternal death, where the source of information is the family of those who die, generating biases due to the grief that implies the loss of a loved one. All this has made the extreme maternal morbidity one of the most important events to watch today, as a complement to the traditional monitoring that we have been doing of maternal mortality 12.
Despite the above, the implementation of the extreme maternal morbidity event in Latin America has faced three difficulties. The first one is that there is no consensus around the criteria for the identification of cases of extreme maternal morbidity; the second is that the indicators generated from the surveillance of the extreme maternal morbidity are not comparable; and the third one is related to the methodology used for the analysis of the case, which is not adequate to assess the quality and safety of obstetric care, and even less for the generation of improvement plans that seek this purpose 13.
Say, of WHO, proposed three groups of criteria for the identification of a case as extreme maternal morbidity. Then she classified those, as clinical criteria, criteria based on laboratory tests, and criteria based on the management of pregnant woman. According to this proposal, any pregnant woman who meets one or more of these criteria must be considered as maternal near miss and with an imminent risk of death. Table 1 describes the criteria proposed by Say in 2004 for identifying an maternal near miss patient 14,15.
Table 1 Criteria for identifying an event as “Maternal Near Miss” (MNM).
| Clinical criteria | Laboratory criteria | Pregnant women management criteria |
|---|---|---|
| Acute cyanosis | O2 saturation <90% for more than 60 minutes | Hysterectomy after infection or bleeding |
| Panting | Pao2/Fio2 <200 mmHg | Continuous use of vasoactive drugs |
| Respiratory rate >40 o <6 bpm | Creatinine >300 lmol/mL ó >3.5 mg/dL | Cardiopulmonary resuscitation |
| Shock | Bilirubin >100 lmol/L ó >6.0 mg/dL | Dialysis for acute kidney failure |
| Cardiac arrest | pH <7.1 | Any non-anesthetic intubation or ventilation |
| Oliguria does not respond to fluids or diuretics (<30 ml/h for 4 hours) | Lactate >5 mmol/L | Transfusion of> 5 units of blood or red blood cells |
| Any loss of consciousness for more than 12 hours | Acute Thrombocytopenia (< 50,000 platelets) | |
| Stroke | ||
| Uncontrollable epileptic status | ||
| Total paralysis | ||
| Jaundice in the presence of preeclampsia | ||
| Coagulation failure |
Source: Say et al14.
In the case of Latin America, it is considered that these identification criteria do not provide the possibility of anticipating death. A pregnant woman in an African or Latin American country who meets one or more of these criteria, probably does not have the opportunity of an intervention to prevent death. For this reason, WHO left it up to countries and regions to adopt their own criteria according to their level of development and institutional capacity to resolve emergency conditions 13.
In the framework of this recommendation, Okong et al in 2006 proposed a set of criteria to identify extreme maternal morbidity in Africa, which are not supported by criteria related to laboratory tests, due to the inability to access some technologies 16. This proposal was considered very consistent, since it was mainly based on clinical criteria of organ dysfunction or systems for the identification of pregnant women who could present with extreme maternal morbidity, as proposed in the original publication by Say 13,16. It also took into account some situations that have to do with the management provided to pregnant woman, such as an emergency hysterectomy, anesthetic accidents, and patient's admission to an Intensive Care Unit (ICU).
In 2007, during a meeting sponsored by the Latin American Federation of Obstetrics and Gynecology (FLASOG) in Santa Cruz de la Sierra (Bolivia), the WHO proposal was analyzed and the term extremely serious maternal morbidity was adopted (4.17). Likewise, a reflection was made about the inclusion criteria of greater applicability in the region; and there were agreed inclusion criteria such as the presence of eclampsia, septic shock, hypovolemic shock, failure of any organ or system, admission to an intensive care unit, surgery and acute or emergency blood transfusion. Likewise, each one of these criteria was defined based on the clinic and, unlike the proposal of a group of experts from African, it was decided to use some clinical/laboratory tests to diagnose organic failure, taking into account the resolving capacity of Latin American health institutions 16,17.
In the absence of consensus, the Pan American Health Organization (PAHO) led in 2016 a collaborative investigation in Latin America to assess the predictive value of the criteria used to classify a case as maternal near miss (18. The results of this study made it possible to establish that from the clinical parameters that were considered, the alteration of the state of consciousness, be it coma or mental confusion, and criteria such as oliguria and seizures were associated with a greater occurrence of maternal near miss. Table 2 lists the parameters with the highest predictive value from the clinical/laboratory tests point of view, clinical conditions, and the interventions required for the management of pregnant women 18.
Table 2 High predictive value criteria for the identification of a case as "Maternal Near Miss"
| Clinical Parameters | Laboratory Parameters | Conditions | Intervention |
|---|---|---|---|
| Altered state of consciousness | Creatinine ≥1.2 mg/dL | Placental accretion | Admission to ICU Laparotomy (Excluding Cesarean Section) |
| Oliguria | Platelets count <100,000/mL | Pulmonary Edema | Administration of blood products. |
| Seizures | Transaminases ≥70 U/L | HELLP Syndrome, Sepsis | Use of uterotonics |
Source: De Mucio et al18
In summary, there is no agreement in Latin America on the inclusion criteria to identify a case as an extreme maternal morbidity; therefore, the indicators generated from its surveillance are not comparable. This generates a distortion that makes it almost impossible to interpret the behavior of the event 19,20.
It is of relevant importance to standardize the criteria for identifying extreme maternal morbidity at local and regional level, in order to avoid errors in estimating the event. In Colombia, in 2015, a number of clinical conditions were included that generated an overestimation of this prevalence, which is why the criteria had to be adjusted again in 2017 19. As a lesson learned, a Latin American standard for the identification of extreme maternal morbidity must be agreed, supported by the criteria mentioned in Table 2.
We consider that this effort will not be sufficient and will not have the expected transcendence if the consensus does not include the adoption of a methodology for the analysis of the event, focused on evaluating the quality and safety of the care provided to pregnant women 21. The extreme maternal morbidity event is a tracer of quality of care that requires a different analysis methodology than the traditional one 22,24; it offers a more efficient alternative for monitoring mothers, since it provides more accurate data, which allows developing action plans to improve obstetric care, and thus prevent maternal mortality.
In 2014, the “security model for obstetric emergency care in health institutions” was published in Colombia, which develops an analysis focused on safety. In this model extreme maternal morbidity is considered an indication of insecure care that may be the consequence of an adverse event or an incident. From this perspective, the analysis is based on the organizational model of causality of errors and adverse events. This facilitates the identification of the determining factors that led to unsafe actions that compromised the quality and safety of obstetric care 21.
This model of analysis, focused on processes and not on people. This ensures the development of more effective action plans, in order to avoid unsafe actions, which, if persist, would perpetuate care failures, increasing the risk of severe morbidity and maternal death 21 (Fig. 1).
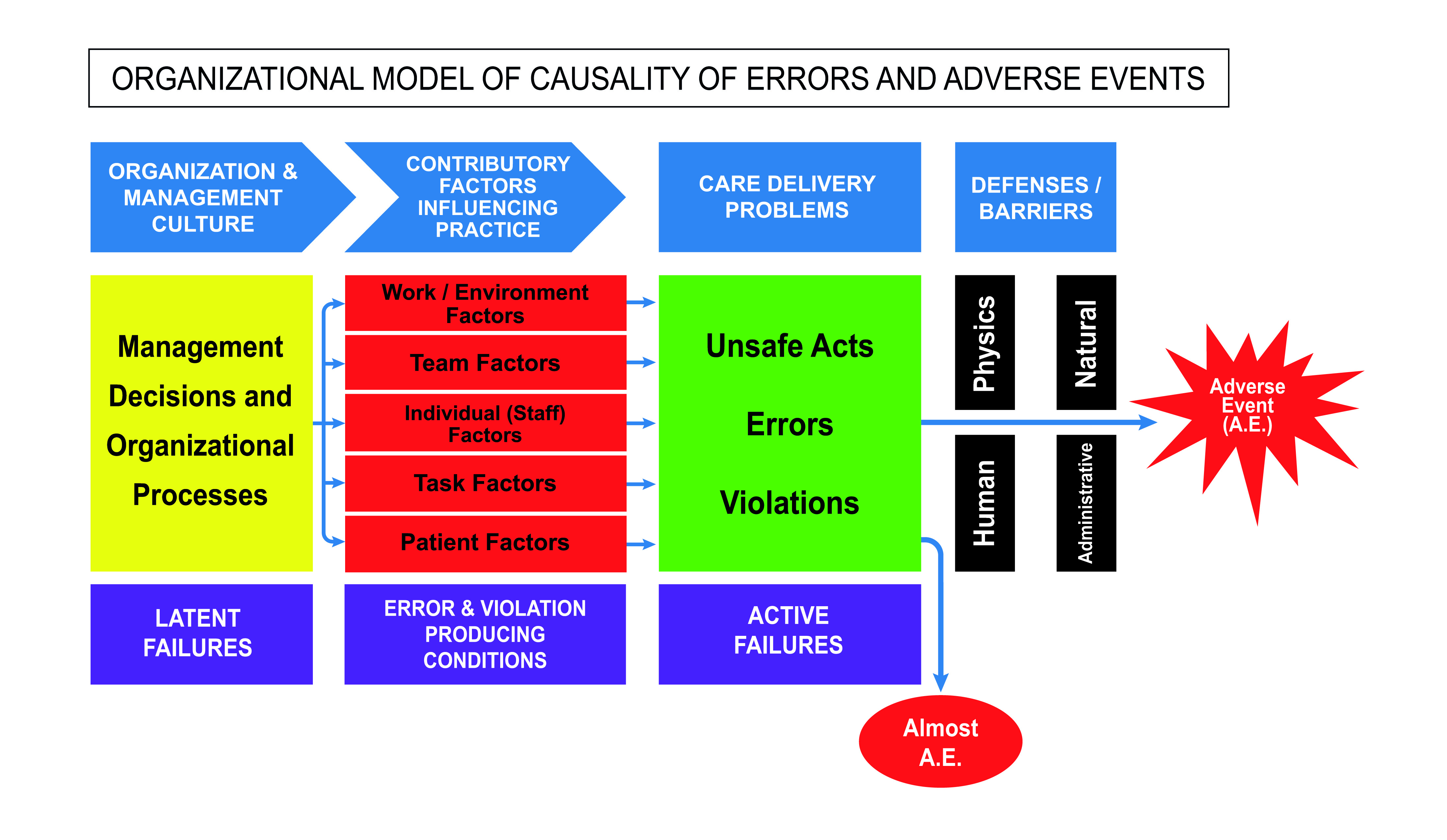
Figure 1 Organizational model of causality of clinical incidents. (Translated with modifications of the document System Analysis of clinical incidents: the London protocol16).
We hope that this reflection contributes to rescue the usefulness of extreme maternal morbidity as a tracer event of quality and patient safety. A paradigm shift is required, beyond the unification of the criteria for case identification. It implies focusing on an analysis based on clinical safety, in order to promote the development of more effective action plans for the reduction of maternal death in Latin America and the Caribbean region.











 text in
text in 



