Remark
| 1)Why was this study conducted? |
| This publication arises as a response to the need to order, in a practical way, the best practices for the management of infection during pregnancy, taking into account that as it is a recent in fection, the evidence is scarce and many of the questions are not. they are completely resolved. |
| 2) What were the most relevant results of the study? |
| The proposal of a management protocol based on the available evidence, supported by a robust bibliographic review, which incorporates concepts of global acceptance. |
| 3) What do these results contribute? |
| They provide the best practices that must be taken into account to protect the health of the mother, the fetus and the newborn, during COVID 19 infection and at the same time protect the health team in charge of obstetric care, which are applicable in a low and high complexity care setting. |
Introduction
New cases of infected people by COVID-19 are being daily reported in most of the countries. Some of them have started the pandemic community stage where the number of cases without any epidemiologic link is getting higher, and an exponential increase of the infected people is expected; that means that the probability of expectant women to be infected can increase 1.
In this scenario, it is logical that a sense of panic in our community is generated because of the lack of reliable indicators, strong clinic research that enlighten the way for prevention and possible treatments in this pandemic besides the big amount of fake news that is found on social networks. This article can be taken as a resource for health care professionals in which all the given concepts are based in a combination of available evidence, good practices and experts’ opinions that look forward to contributing to public health.
The Virus
Coronavirus illness 2019 (COVID-19) is an airways infection caused by the new coronavirus (SARS-CoV-2, Coronavirus of the severe acute respiratory syndrome-related virus) that was found for the first time in Wuhan, China in December 2019. This was rapidly spread causing a declaration of pandemic by The World Health Organization (WHO) on March 11th 2020. Other coronavirus infections include the common cold (HCoV 229E, NL63, OC43 y HKU1), The Middle East Respiratory Syndrome (MERS-CoV), and the Severe Acute Respiratory Syndrome (SARS-CoV) 2.
Transmission
Most of worldwide COVID-19 cases has an evidence of transmission from human to human. According to WHO, this virus is not transmitted through the air but the contact of respiratory drops of sick people. For instance, this sickness can be spread from person to person through the droplets that come from the nose or the mouth when a person coughs or exhales. These droplets fall over surfaces that surround people, and because of this, people who touch those surfaces can catch it. For this reason, it is very important to keep more than 1 meter of distance from the person who is ill. This risk increases when someone is constantly in touch with a sick person who has symptoms or consequentially touching a surface, object or even the hand that has been infected with respiratory secretions of an infected person; Thus, this person touch his/her mouth, nose or eyes by him/herself 3.
As a result, a social isolation is proposed in most of the countries as a restraint measure, as well as frequently hand-washing and permanent disinfection of fomites that can be contaminated with COVID-19.
Social isolation can have big negative impact on women’s sexual and reproductive health who require to have a close contact to the health-care services for any special condition; hence, expectant mothers who require prenatal attention services, childbirth, postpartum period, when the access of voluntary pregnancy disruption is required, and women who need gynecological treatments either for the cancer management or reproductive medicine where the inactivity could get more devastating results than for the SARS-CoV-2 infection 4.
In this type of situations, wisdom has to be a must so that the attention to women who are in touch with the health-care system under reduction precepts of the COVID-19 transmission is guaranteed; Moreover, the allowance of secure attention to women with COVID-19 suspicion/verification infection as well as the security of the health-care workers that are in direct contact with COVID-19 infected patient.
Impact on the mother and the fetus
The evidence up to now shows that pregnant women do not seem to get the infection that population in general. The available information over the effects of the infection either for mother and newborn is limited. Pregnancy itself produces some changes in the immunity system and the response to the viral infections in general can cause more severe symptoms, especially when the infection is acquired in the third quarter of pregnancy, and this would be the same for COVID-19 5.
It can be considered as confirmed case, that symptomless pregnant woman or with a suspected clinical picture with a positive result in any of the molecular or genome tests that detect SARS CoV-2/COVID 19.
The sickness course is usually slight but 20% approximately evolves to severe forms. The SARS-CoV-2 incubation period is 5 days average (IC 95%: 4.5-5.8 days) while the development of the symptoms is 11.5 days average (IC 95%: 8.2-15.6 days) in the 98% of the cases. According to this, only 1% of the population would develop later symptoms to a 14-day isolation period. The more frequent symptomatology is fever over 38ºC (90%), cough (76%), myalgia (44%), expectoration (28%), headache (8%), diarrhea (3%), and odynophagia in a lower proportion, respiratory difficulty and tiredness.
The impressive laboratory infection findings of SARS-CoV-2 are abnormalities in thorax x-rays in severe cases (100%), leukopenia (9-25%), lymphopenia (35-70%), thrombocytopenia (5-12%), and the rising level of the RT-PCR as well as the transaminases 6.
The current data do not suggest a higher risk of abortion or premature gestational loss, and is less probable that the infection can produce congenital defects. Premature childbirth cases have been described, restraint of the intrauterine fetal growth, and the loss of intrapartum fetal wellness 7.
There are no intrauterine infection confirmed cases up to now. However, recent evidence has suggested that it is probable the virus can be transmitted vertically, although the proportion of affected pregnancies and the importance for the newborn has not been determined yet 8,9. Reports of previous cases in China suggested that the was no presence of the virus in the amniotic fluid, blood of the umbilical cord, swabs of neonatal throats, placentas sabs, genital fluid, and in the samples of maternal milk of mothers infected with COVID-19 10.
Recommendations for the attention in obstetrics attention services
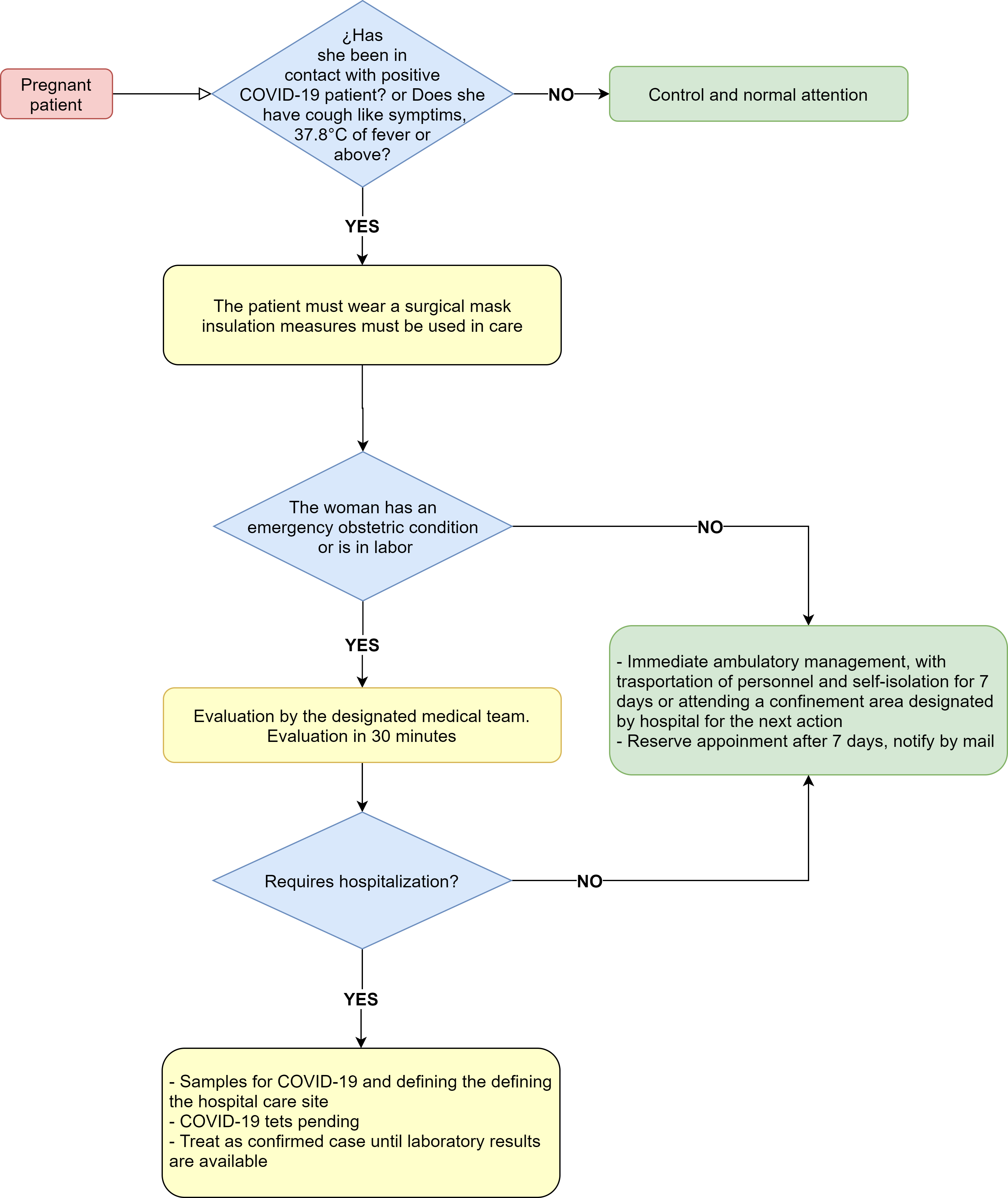
To determine the type of management of the expectant mothers (Fig. 1), it is a key factor to identify suspicious or confirmed infection at the moment of the initial evaluation the presence or not of the symptomatology, its harshness and the presence of comorbidities. At the moment of the evaluation, the use of surgical mask, eye protection, as well as gloves for the procedure practices such as echography and monitory are recommended; Moreover, hand washing bearing in mind the safety precaution of disinfecting equipment and surfaces after assisting each expectant woman. If the patient is suspected or is infected by COVID-19 and is a symptomatic one, so it is a must to use an N-95 mask.
It is mandatory to fulfill the isolation procedure of droplets by means of the use of face mask and hand wash for both Symptomless and Symptomatic patients during their stay at their corresponding medical center; this includes waiting rooms, office areas, isolation room transfers, and radiology and/or echography service if needed. These actions will help the doctor’s office to avoid infection or exposure of the other people who can be in the office or in the waiting room 11,12.
If a suspicious case or confirmed infection with minor symptomatology without the presence of comorbidities is considered after the initial evaluation, the decision of home isolation is relevant unless there could be and obstetric condition associated to the requirement of hospital management 13.
During home isolation, it is recommendable regulations such hand-washing procedures, relatives isolation and use of face masks, daily temperature control, symptomatic management with acetaminophen 500 mg every 6 hours, rest and hydration with plenty of liquid intake. Moreover, a written report must be delivered which includes alarm signs in simple and clear language, obstetric alarm signs, the presence of faster respiratory symptoms, pain and/or waist hissing, sustained spew, persisting fever of difficult control for more than 24 hours that does not get well with antipyretic, drowsiness, confusion or difficulty to wake up, seizures or convulsions, dry mouth, and urinate less or nothing.
The obstetric patients with confirmed SARS-CoV-2 must be kept under the home isolation precautions until the secondary transmission risks to other people has been considered low. The decision to disrupt the home isolation safety measures might be taking according to each particular case, consulting the medical attention providers 14.
The expectant mothers with suspected or infected symptomatic cases with COVID-19, with severity criteria, hospitalization is required and must be directed to the designated place by the medical center for their immediate attention.
Childbirth attention or cesarean
As a good practice in women in labor or who appeal an obstetric emergency, a previous diagnostic test before the admission is recommended. For the childbirth attention or cesarean, infected women with COVID-19 always have to wear face mask, and the team in charge of the attention must wear personal protection items that includes masks, headsets, N-95 face masks, gloves, and fluid-proof fabric coat; this test will be developed in an isolation area with negative pressure preferably. If facilities difficulties are presented, the procedure must be done in an assigned surgery room 11,12.
It is also considered good practices such as the flashing monitoring of the fetal heart rate during childbirth. The reduction of the second stage of labor, temperature control, breathing rate and oxygen saturation (PO2 is never less than 95), the admission of a companion, who can ideally be a person that kept in touch with the patient previously the childbirth labor, and who did not appeal any symptoms or risk factors for complications of COVID-19; The routine way of the umbilical cord clamp, and to allow (if possible) skin contact minimizing the mother/son transmission risks 15,16.
Special considerations
From the pharmacological point of view, the use of steroids for induction of fetal lung maturity is not contraindicated, nor the use of Magnesium Sulfate for the management of Preeclampsia-Eclampsia., Treatment with hydroxychloroquine or chloroquine, antivirals and antibiotics is reserved for pregnant women with severe health commitment and under institutional schemes, knowing the fact that these therapeutic. These therapeutic options are under evaluation. Thromboprophylaxis is considered a good practice for the prevention of thrombotic disease.
Attention to the newborn baby and maternal lactation
The neonatal adaptation will be done in the radiant asset table, umbilical cord sample to collect stem cells will not be arranged, and peridural analgesia is recommended before general anesthesia to diminish the risk of spray releasing at the moment of intubation and extubation 17.
The risk of intrapartum vertical transmission or through maternal lactation is less probable, according to some reports of cases that have been published until now, the risk of transmission to the newborn baby by means of droplets or by physical contact is considered as high risk as in population in general.
All the newborn babies with confirmed infected mother as well as the ones with suspected cases, COVID-19 infection must be discarded.
Mothers and newborn babies might be allowed to stay together as long as the use of face masks, continuing disinfection of surfaces and hand-washing procedures are guaranteed, keeping at least two-meter distance between the mother and the cradle especially after the childbirth and during the breastfeeding, either doctors have suspected the COVID-19 infection in mothers or babies (probable or confirmed) 18.
Isolation is suggested in a neonatal unit for those symptomatic newborns no matter the presence or not of symptoms of the suspected or confirmed mother with COVID-19 infection, until COVID-19 infection can be dismissed. In the case of the pre-term newborns, sons of symptomatic or confirmed mothers with the COVID-19 infection, they must be in quarantine in a neonatal unit 19.
In a neonatal ICU (Intensive Care Unit), all the personnel and companions must keep the protection measures against droplets and contact with others. To enter the neonatal unit, contact risks, respiratory symptoms and precedent fever in all parents and caretakers who get into the unit must be assessed 18.
It is recommended to start maternal lactation in the first hour after the birth as long as the clinic conditions of the newborn as well as his/her mother are allowed. In serious illness or medical complications, it is suggested that the mother ensures milk removal to avoid mammary congestion problems. Baby boys and girls can drink the removal milk which is why removal techniques counseling must be provided not only for the mother but also for her family, with all the storing and conservation of the maternal milk recommendations as well as the way to offer that milk to the baby either with glass or spoon.
During the maternal lactation, the following prevention measures must be always guaranteed in order to reduce the risk of transmission of the virus during the breastfeeding or milk removal: Frequent hand-washing procedures during 40 to 60 seconds before having a physical contact with the baby or before removing milk; Use permanently standard surgical face mask (total covering of nose and mouth); avoid speaking or coughing specially during the breastfeeding or milk removal; keep the routine disinfecting measures of the areas the patient have contact with 20.
It is important to bear in mind that this is a changing situation and the concepts that are delivered here can be updated as long as new information is generated, and its application will depend on the pandemic epidemiologic moment. However, it is clear that the provided evidence up to now gives us enough information to protect the expectant mother as well as to protect the health-care personnel, avoiding panic situations and assuming a good sense attitude that will be undoubtedly beneficial for all the society.











 text in
text in