Remark
| 1) Why was this study conducted? |
| This study was conducted given the lack of information on the distal medial striated artery in the different population groups, in order to obtain relevant biometric and anatomical information, useful for clinical and surgical management that compromise this vascular structure. |
| 2) What were the most relevant results of the study? |
| The main finding was the sinuous trajectory that was observed in 57.7% on the right side and 45.1% on the left hemisphere. Also an important alteration found in the biometric analysis was hypoplasia that could be related to the decrease in blood supply to the basal ganglia. The diameter was 0.5 ± 0.2 mm and its total length was 20.3 ± 4.1 mm. In addition, the observed collateral circulation contributes to the blood supply and the perfect functioning of the subcortical nerve structures in the event of injury. |
| 3) What do these results contribute? |
| This study, carried out on cadaveric material, provides relevant qualitative and morphometric information on the distal medial striated artery. The biometric data of its origins and qualitative characteristics of its trajectory, contrasted with previous studies carried out in other population groups, enrich the morphological concept and allow optimization of surgical interventions in order to prevent and / or reduce deficits and postoperative neurological damage, as well as the diagnosis and management of clinical events that compromise this vascular structure. |
Introduction
The distal medial striated artery has been described in the literature since the 19th century as a small, constant artery that emerges from the base of the anterior cerebral artery 1-3. Also known as Heubner's recurrent artery in memory of O. Heubner who was the first to study it. It is usually the longest of the medial lenticulostriated arteries that originate from the anterior cerebral artery 2-5.
The distal medial striated artery can originate from the anterior cerebral artery at the level of its pre-communicating, post-communicating segments up to the callosomarginal artery or from the junction of the anterior cerebral artery with the anterior communicating artery 4,5. It presents a generally posterolateral path to the pre-communicating segment of the anterior cerebral artery, likewise, it is near to the posterior region of the orbitofrontal cortex and is directed to penetrate the anterior perforated substance [6,7]. In its course, give branches to supply the olfactory region, anterior portion of the caudate nucleus, putamen, external segment of the globus pallidus, and the anterior arm of the internal capsule 4-6.
The distal medial striated artery originates between 40-50% of the post-communicating segment of the anterior cerebral artery, while between 5-30% emerges from the pre-communicating segment. Biometric data report a length of 15-46 mm and a diameter of 0.3 - 1.2 mm. The distal medial striated artery agenesis has been reported between 5% - 7% of the hemispheres 1,5,7-9. Its morphology is characterized by presenting a posterolateral relationship with the anterior cerebral artery and an oblique trajectory in 38-54% of cases. It follows a sinuous trajectory at 15-20% 5.
The lesion of the distal medial striated artery is related to the predominant weakness of the upper limbs and the contralateral face (fasciobrachiocrural hemiparesis), dysarthria, choreoathetosis, behavioral changes such as hyperactivity, due to the interruption of corticostriatal pathways, and aphasia 4,6,10-13.
Previous studies have reported anatomic variations of the distal medial striated artery related to origin, absence, duplication, diameter, orientation, and trajectory 2-5,9,10,14. The adequate knowledge of the morphology of the distal medial striated artery allows the performance of better procedures and surgical interventions, such as the management of aneurysms in the anterior communicating artery, in addition to the assessment of the clinical signs by obstructive or hemorrhagic processes that compromise this small vessel 11,13.
Given the limited information on the distal medial striated artery in the various population groups, this study evaluated its morphology in a sample of male cadaveric material of Colombian mixed-race individuals that provide relevant biometric and anatomical information, useful for clinical and surgical management that compromise this vascular structure.
Materials and Methods
A descriptive, transversal cadaveric study was designed. The distal medial striated artery of unclaimed male bodies, aged 18 -65 years, who underwent autopsy at the Institute of Legal Medicine and Forensic Sciences of Bucaramanga-Colombia were studied. The inclusion criteria of the sample evaluated were: subjects of the ethnic group with racially mixed (a mixture of white hispanics with natives) and adults with legal age. The exclusion criteria were: subjects with evidence of having died from direct trauma like a violent death with damage to brain tissue specifically, or pathologies that compromised the brain such as stroke that could disturb the morphological and morphometric study of the cerebral arteries. The excluded neurological diseases were taken into account thanks to what was reported by the clinical history of the forensic autopsy protocol of the institute of legal medicine. A time limit for the death of the subject was defined to consider the appropriate specimen for evaluation, which was less than 24 hours, once it entered the institute of legal medicine.
Each specimen was subjected to bilateral canalization of the proximal segments of the internal carotid arteries (ICA) and through these was performed washing and presetting of the brain with 3% formaldehyde. Additionally, the carotid vessels were perfused with 100 ml of semi-synthetic resin (E210® Basf 80 cc palatal mixture; 20 cc styrene) impregnated with mineral red color 16,17. Once the polymerization of the resin was obtained (30 minutes), the brain exeresis was performed. Then, the sample was subjected to 10% formaldehyde fixation for 15 days.
Subsequently, with microdissection material, the leptomeninges were released, a maneuver that allowed identifying the structures that configuring the arterial circle of the brain and each of its branches. The different morphological expressions of the distal medial striated artery were recorded, in relation to their level of origin, trajectory, duplication, diameter, and length. The length of this vessel was taken into account from its origin at the anterior cerebral artery to its entry into the anterior perforated substance.
The trajectory of the distal medial striated artery from its origin to its completion in the anterior perforated substance was classified as sinuous, oblique, inverted in L, and horizontal 10. The distal medial striated artery with a caliber of less than 0.40 mm were considered hypoplastic. To evaluate the morphometric characteristics of these vessels, a digital calibrator (Mitotuyo ®) was used; this technique has high precision type: 0.02 mm (0.001"), and its measurement is expressed in units of millimeters, hundredths and thousandths of millimeters.
The presentation of this manuscript was developed taking into account the AQUA checklist, in which guidelines are followed for study ethics in deceased research subjects, or in tissue (hard/calcified or soft) obtained from human subjects. These consensus guidelines helped standardize a reproducible and ethical study methodology 18,19.
Statistic analysis
From each specimen studied, digital photographs (supporting the recorded observations) were taken. The data obtained were typed in Excel and the statistical analyzes were performed in SIGMASTAT 4.0. Continuous variables were described with their averages and dispersions; Nominal variables with their proportions. Statistical tests of chi-square (X2) and Student's test (t) were performed accepting an alpha error of up to 5%, used to determine if there is a significant difference between the means of two groups, in this case, taking into account the laterality of the samples.
Results
The distal medial striated artery of 71 brains were studied, of which 71 (100%) were men (Table 1). Age ranged from 18-65 years, with an average of 33.8 years. Specimens were not discarded by the exclusion criteria. The distal medial striated artery was observed in 97.9% and in three specimens it was absent (2.1%) in total (1.4% and 2.8% in the right and the left side respectively (Fig. 1). In four cases (2.8%) the distal medial striated artery was doubled, 4.2% in the left hemisphere, and 1.4% on the right side were found (Fig. 2). It presented in 136 cases (95.7%) as a single trunk (Fig. 3A), while in 6 cases (4.2%) was presented with a common trunk with the orbitofrontal artery (OF).
Tabla 1 Distribution by age groups and gender.
| Age (years) | Male No(%) |
|---|---|
| 18-20 | 7 (9.9) |
| 21-29 | 16 (22.5) |
| 30-39 | 24 (33.8) |
| 40-49 | 13 (18.3) |
| 50-59 | 5 (7) |
| 60-65 | 6 (8.5) |
| Total | 71 |
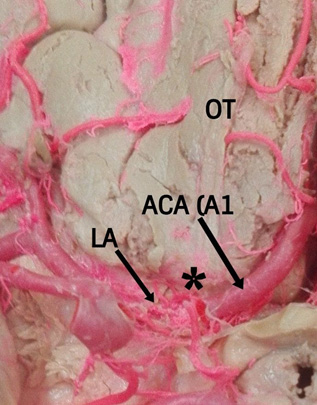
Figure 1 Agenesis of the right distal medial striate artery (DMSA). The lenticulostriated branches (LA) from the middle cerebral artery penetrated the anterior perforated substance and supplied the blood supply in this region. Identification of anterior cerebral artery A1 segment (ACA-A1). Olfactory tract (OT).
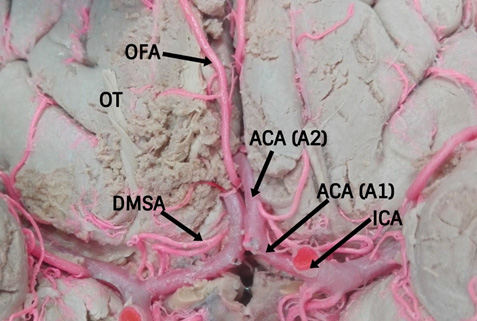
Figure 2 Doubled and L inverted trajectory of the right distal medial striate artery. Identification of origin of the distal medial striate artery (DMSA) from the anterior cerebral artery post-communicating segment (ACA- A2), identification of anterior cerebral artery pre- communicating segment (ACA-A1), olfactory tract (OT), orbitofrontal artery (OF) from ACA and internal carotid artery (ICA).
It originated in 63 samples (44.4%) from the anterior cerebral artery and anterior communicating artery, junction site, in 62 specimens (43.7%) from the anterior cerebral artery post-communicating segment (Figs. 2, 3A and 3B), in 16 cases from the anterior cerebral artery pre-communicating segment (11.3%) and in one case it originated from the orbitofrontal artery (0.7%), without significant differences according to the presentation side. (p= 0.967).
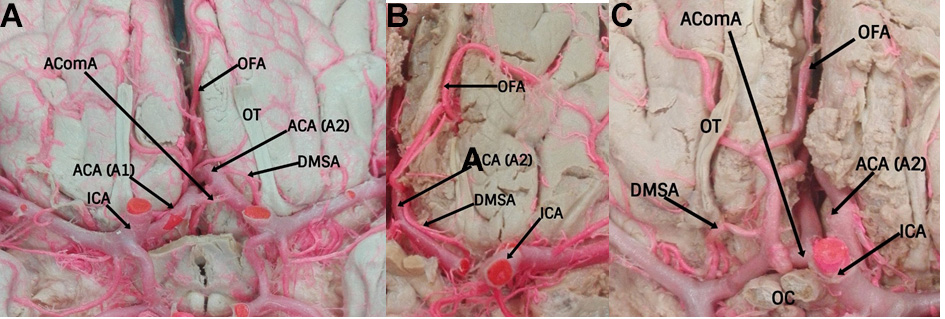
Figure 3 A. Oblique trajectory of the left distal medial striate artery. Identification of origin of the distal medial striate artery from the anterior cerebral artery post-communicating segment (ACA- A2), identification of the internal carotid artery (ICA) and orbitofrontal artery (OF) from the ACA. B. L inverted trajectory of the left distal medial striate artery and superolateral relation with the proximal segments of the anterior cerebral artery (ACA). Identification of origin of the distal medial striate artery (DMSA) from the anterior cerebral artery post-communicating segment (ACA- A2), identification of the anterior cerebral artery pre- communicating segment (ACA-A1), internal carotid artery (ICA), olfactory tract (OT), anterior communicating artery (AComA) and orbitofrontal artery (OF). C. Sinuous trajectory of the right distal medial striate artery and lateral relation with the proximal segments of the anterior cerebral artery (ACA). Identification of origin of the distal medial striate artery (DMSA) from the anterior cerebral artery post-communicating segment (ACA- A2), identification of the internal carotid artery (ICA), olfactory tract (OT), anterior communicating artery (AComA) with aneurysm, optic chiasma (OC) and orbitofrontal artery (OF).
The length of the distal medial striated artery was 20.3 ± SD 4.1mm. Likewise, the diameter was 0.5 ± SD 0.2mm and was found with a caliber less than 0.35 mm in 43 cases (30.3%) (Table 2, Fig. 3B). The distal medial striated artery followed a sinuous trajectory in 73 cases in total with 41 cases (57.7%) on the right side and 32 cases in the left one. (45.1%) (Fig. 3C), oblique only in 12 cases (16.9%) and 16 (22.5%) in the right and left side respectively (Fig. 3A), L inverted (Fig. 3B) and horizontal had less incidence, without significant differences according to the presentation side (p= 0.690) (Table 2).
Table 2 Biometric and qualitative variables of the distal medial striate artery according to the presenting side. Described in millimeters, number of cases and percentage.
| Side | Right | Left | ||||||
|---|---|---|---|---|---|---|---|---|
| IC 95% | IC 95% | |||||||
| Lenght (mm) | 20.6 | (20.39-20.81) | 20.1 | (19.44-20.76) | ||||
| Diameter (mm) | 0.5 | (0.47-0.53) | 0.5 | (0.47-0.53) | ||||
| Distance from origin of the distal medial striate artery to the anterior communicating artery (mm) | 2.57 | (2.36-2.78) | 2.77 | (2.61-2.93) | ||||
| n | % | n | % | |||||
| Trayectory | Sinuous | 41 | 57.7 | 32 | 45.1 | |||
| Oblique | 12 | 16.9 | 16 | 22.5 | ||||
| L inverted | 7 | 9.9 | 11 | 15.5 | ||||
| Horizontal | 11 | 15.5 | 12 | 16.9 | ||||
| Orientation in relation with the anterior cerebral artery | Superolateral | 38 | 53.5 | 30 | 42.3 | |||
| Superomedial | 1 | 1.4 | 2 | 2.8 | ||||
| Lateral | 27 | 38.0 | 21 | 29.6 | ||||
| Inferolateral | 2 | 2.8 | 13 | 18.3 | ||||
| Double vessel | Posterolateral | 3 | 4.2 | 5 | 7 | |||
| 1 | 1.4 | 1 | 1.4 | |||||
| Absent | 3 | 4.2 | 2 | 2.8 | ||||
IC 95%: confidence interval with a standard error of 5%
No significant differences were found in this comparison.
The distance of the distal medial striated artery which originated in the post-communicating segment until the origin of the anterior communicating artery, was 2.6 ± SD 1.12 mm while the distance of those originating in the pre-communicating segment until the anterior communicating artery, was 2.7 ± SD 1.05 mm (p= 0.973).
The relationship of the distal medial striated artery with the proximal segments of the anterior cerebral artery was superolateral in 68 cases, 38 (53.5%) and 30 (30%) for the right and left hemisphere respectively (Fig. 3B), posterolateral in 8 cases, three cases (4.2%) in the right and 5 cases (7%) in the left side. Other values are described in Table 2.
The completion of the distal medial striated artery in the previous perforated substance was given by a single trunk in 129 cases (90.9%), bifurcation in 9 cases (6.3%) (Fig.2), and trifurcation in four cases (2.8%).
Discussion
The origin of the distal medial striated artery of the anterior cerebral artery and anterior communicating artery, the junction has been reported between 30-62% 3,8,10. In this study, the incidence was found in the union of the anterior cerebral artery and anterior communicating artery in 44.6%, which is consistent with Gasca et al. (5, also found emerging from the post-communicating segment of anterior cerebral artery in 43.8%, data that differs with the findings of Loukas et al (23.3%) 11. In a lower incidence, it emerged from the pre-communicating segment of the anterior cerebral artery (10.8%), a characteristic similar to that reported by Boongird et al (7.9%) 1.
The high incidence of the origin of the distal medial striated artery at the junction of the anterior cerebral artery and the anterior communicating artery or near it, should be taken into account for the surgical planning of anterior communicating artery aneurysms that can prevent the injury of the distal medial striated artery. In this study we found a very low incidence (0.7%) of common trunk origin with the orbitofrontal artery, a finding that agrees with Kedia et al. (9, which can cause complications during surgical interventions such as obstruction or damage to the irrigation, caused by the connection with the trunk of the orbitofrontal artery and the ignorance of these variations of the origin of the distal medial striated artery, even with the presence of aneurysms at the level of the anterior communicating artery.
The agenesis observed in our series (1.4% and 2.8% for right and left hemisphere respectively) is in a medium-range with that reported in previous studies (1.4-6.6%) 2,3,9,15. Four presentations of the duplicate distal medial striated artery were observed, in two cases they were in parallel, and in the other they were arranged forming an inverted triangle between the two. The results of Dimitriu in relation to the duplication of the distal medial striated artery are considerably higher (14.3%) 2.
The caliber of the distal medial striated artery in our study was similar to that reported by Falougy et al. 3, slightly smaller than that indicated by Kipré et al., (0.7 mm) 10. It is noted that Loukas et al., reported diameter of 0.9 mm for this vascular structure 11.
The hypoplasia of the distal medial striated artery observed in our series was 43 cases (30.3%), it is considerably higher than previous reports and could be related to the decreased blood supply to the basal nuclei and anterior arm of the internal capsule, however, in these cases, it was found that the lenticulo-striated branches from the middle cerebral artery penetrated the anterior perforated substance and supplied the blood supply in this region 2,3,12. In the event of an obstructive process of the proximal segment of the middle cerebral artery concomitantly with distal medial striated artery hypoplasia, the involvement of the regions irrigated by the latter is evident 2,3,13.
The length of the distal medial striated artery (20.3 mm) was similar to that observed by Kedia et al. (9, although it differs slightly from that reported by Loukas et al 11, who reported a length of 18 mm taking into account the structures originated in the pre communicating segment of the anterior cerebral artery. In our samples, a predominant sinuous trajectory was reported, different from that reported by other authors who obtained greater oblique trajectory of the distal medial striated artery 5. This sinuous anatomical feature of the distal medial striated artery makes it vulnerable and hinders the surgical procedures performed on the anterior segment of the arterial circle of the brain.
Alterations of the distal medial striated artery include occlusions in its path, cerebral infarctions, arteriovenous malformations, and strokes. The deficit of blood supply to the structures of the core nuclei specifically in its anterior region and in addition to the anterior arm of the internal capsule result in hemiparesis with a facio-brachial predominance, which is a recognized sign in patients with stroke in adults, in addition to Paraparesis can be caused in turn by bilateral anterior cerebral artery infarction, associated with the absence or hypoplasia of some segment of the anterior cerebral artery 11,14.
Various factors such as sample size, different measurement methodologies, and phenotypic expressions of each population group evaluated can explain the qualitative and morphometric variability observed in the various studies of the distal medial striated artery.
This study, carried out in cadaveric material, provides relevant qualitative and morphometric information of the distal medial striated artery, this is the greatest advantage and may relate what is observed with what is expected, in this way neurological procedures will be carried out safely. Biometric data of its origins and qualitative characteristics of its trajectory, contrasted with previous studies carried out in other population groups, enriches the morphological concept and will allow the optimization of surgical interventions in order to prevent and/or reduce deficits and postoperative neurological damage, as well as the diagnosis and management of clinical events that compromise this structure.
The topographical knowledge of this structure determines the vulnerability of the vessel because it can complicate surgical procedures performed in the anterior segment of the arterial circle of the brain. In addition, the observed collateral circulation contributes to the blood supply and the perfect functionality of the nervous structures.
Limitations of the study
This was a direct morphological study carried out on fresh cadaveric material - which were donated by the institute of legal medicine- for this reason, the accessibility to autopsies of female bodies and likewise to obtain their samples is limited and the possibility of comparing the findings between male and female specimens is restricted.
Additionally, the lack of a complete clinical history in this type of study limits the realization of correlations between specific pathological antecedents with the morphological findings found. Likewise, despite having a sufficient sample, it is not possible to think about complying with an even larger sample, since the number of specimens supplied by forensic medicine is limited, in this way if one wanted to have an N The older one would be obliged to have a longer observation time.











 text in
text in 



