Remark
| 1) Why was this study conducted? |
| Trauma Hybrid Service is a concept that describes a vertical work scheme that begins with the activation of Trauma Code when admitting a severely injured patient, initiating a continuous resuscitation process led by the trauma surgeon who guides transfer to imaging, angiography, and surgery rooms according to the patient's condition and the need for specific interventions. |
| 2) What were the most relevant results of the study? |
| Hybrid Rooms seek to control bleeding in an operating room equipped with specialized personnel and advanced technology including angiography, tomography, eFAST, radiography, endoscopy, infusers, cell retrievers, REBOA, etc. |
| 3) What do these results contribute? |
| Hybrid rooms integrate different diagnostic and therapeutic tools in one same room, reducing the attention time and increasing all interventions effectiveness.. |
Introduction
Damage control in trauma allows the immediate management of life-threatening injuries, controlling the hemorrhage and temporally containing contamination and anatomical disruptions. The clinical evaluation and diagnostic imaging tools with cutting edge technologies, including intervention radiology, are currently being applied to achieve an early diagnosis and bleeding control. Traditionally, these interventions are performed in separated rooms and considering the patient´s clinical status 1 and the trauma and acute care surgeon´s criteria, aiming to reduce the morbidity and mortality associated with trauma and the medical interventions 2,3; however, the bleeding may not be controllable with the initial interventions, requiring additional interventions 2,4.
Hybrid rooms have been proposed for over a decade in high complexity centers, with the goal of reducing transfer and intervention times. These are operating rooms that integrates both diagnostic/therapeutic imaging technologies and the necessary surgical equipment. These special rooms require the creation of a multidisciplinary team led by the trauma surgeon, conforming the Hybrid Trauma Service. This team facilitates the opportune coordination of the diagnostic and therapeutic interventions available in the hybrid room 4,5. Currently, this concept has been implemented in level I trauma centers showing promising outcomes in the trauma patient care 2,6,7. Despite all the operational advantages, it has a few weaknesses such as the expensive infrastructure required, which has been a constant hindrance for its implementation. This article aims to provide an overview of the current literature regarding the implementation of hybrid rooms in the management of the severely injured trauma patient, as a new concept to be applied in damage control care.
This article is a consensus that synthesizes the experience earned during the past 30 years in trauma critical care management of the severely injured patient from the Trauma and Emergency Surgery Group (CTE) from Cali, Colombia, conformed by experts from the, the University Hospital del Valle “Evaristo Garcia,” University Hospital Fundación Valle del Lili, the Universidad del Valle and Universidad Icesi, the Asociacion Colombiana de Cirugia, the Pan-american Trauma Society, and with the collaboration of national and international specialists from the United States of America and Japan.
“Hybrid Operating Rooms” History
The term “hybrid operating room” was born in 2003 8, referring to a standard operating room with the required equipment to perform medical interventions from all surgical disciplines. Currently, hybrid rooms are being installed on the five continents, incorporating advanced cutting-edge technology including angiography, tomography, surgical room with complementary structural provisions and technology according to the needs of the health service provider. Yuanlin - Taiwan (Christian Hospital), Sao Paulo - Brazil (Coracao Hospital), Okayama - Japan (Okayama University Hospital), Dortmund - Germany (St. Johannes Hospital), Melborune - Australia (Valley Private Hospital), Zurich - Switzerland (University Hospital of Zurich) and Bangkok - Thailand (Royal Thai Army Hospital) are examples of cities that have hybrid rooms at their disposal, with an average opening cost of four million dollars in 2015 9.
Hybrid Emergency Rooms
The first hybrid room focused on hemorrhage control in trauma patients was denominated the RAPTOR (Resuscitation with Angiographic Percutaneous Techniques and Operative Resuscitation) suite, allowing the exsanguinating trauma patient to be admitted and treated on a single room. It consists on a resuscitation operating room with all the anesthesia and vital support equipment, capable of performing surgical interventions guided by radiological imaging techniques 2.
Angiography systems are among the most important resources in the hybrid room infrastructure, allowing the identification and location of the bleeding source, with subsequent control by endovascular techniques. Angiography often avoids an open surgery or allows the surgery to be performed in a non-bleeding setting 10. Furthermore, the most advanced equipment allows 3D visualization of selected anatomical regions such as the brain, improving the efficacy of blind procedures in scenarios where scan imaging is not available 2. Another important component is the CT scanner, which is the current gold standard imaging tool in trauma. CT imaging can guide bleeding control through angiography with a success rate between 85 and 100%, reducing the number of non-therapeutic laparotomies 3. These rooms also count with other diagnostic and therapeutic tools such as eFAST, portable radiographs, endoscopy, cell recovery and cell infusion systems (Cell SaverR y Level 1R), surgical equipment packs for trauma and Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) and Vena Cava (REBOVC) 4,10. Also, a well provisioned blood bank with immediate availability of blood products is essential for the proper reanimation process, which should be initiated simultaneously with the diagnostic and therapeutic interventions 6.
The education and integration of the personnel that is not used to share their work space on a daily basis and the elaboration of specific protocols and simulation scenarios to reduce mistakes and risks for the patient, the personnel and the infrastructure, are a hard and necessary work to manage de proper articulation of efforts leading to a better performance of the unit 2. The trauma and acute care surgeon is an irreplaceable component of this system, as the leader and coordinator of the trauma team, and the responsible person inside and outside the room, he/she must always be present at the institution.
Finally, following damage control interventions with stabilization of the patient´s hemodynamic status (first phase of damage control), he or she must be transferred to an Intensive Care Unit (ICU) to continue with the damage control resuscitation (second phase) and strict monitoring, guaranteeing an early reintervention when necessary.
The integration of human resource, infrastructure, and technology in one unique space focused on bleeding control decrease the morbidity and mortality associated to trauma. However, it requires a high monetary investment, which overcomes the capacity of healthcare systems in multiple settings 4. The maintenance using the incomes derived from trauma attention becomes unsustainable. For these reasons, adaptative strategies must be implemented, optimizing the available resources to obtain a benefit without outgrowing the bounds of sustainable investment.
Hybrid Trauma Service
If the implementation of a hybrid emergency room with the most complete and advanced technology, is not supported by a strict organizational process and trained personal, the benefits of this system could be reduced and the outcomes may not be different from the traditional approach 11, but instead carry additional costs to the healthcare system. On the other hand, a high complexity center with a well-disposed infrastructure, available technology, and an organized multidisciplinary team led by a well-trained trauma and acute care surgeon, can achieve similar outcomes to those obtained on a hybrid emergency room in the management of trauma patients, working as a high complexity hybrid trauma service.
We propose a dynamic vertical algorithm for the optimal use of available resources, supplying the horizontal approach of a hybrid room.
Based on this principle and the experience in our Level I Trauma Center in Cali, Colombia, our team has developed a hybrid functional approach adapted to our limited resources. The logistic and resources needed are shown in Tables 1 and 2.
Table 1 Basic requirements for the implementation of a hybrid trauma service
| Resuscitation Room | Personal | Emergency physician |
| General physician / Resident | ||
| Head Nurse | ||
| Nurse Aides (2) | ||
| Respiratory Therapist | ||
| Stretcher-bearers | ||
| X-Ray Technician | ||
| Equipment | Portable X-Ray | |
| Vital Signs Monitor | ||
| Ultrasound Scanner | ||
| Tourniquet | ||
| Pelvic Binder | ||
| Airway and Mechanical Ventilation Equipment | ||
| Vascular Access and Infusion Equipment | ||
| Drugs (intravenous fluids, sedation, vasoactive and hemostatic agents) | ||
| Blood Bank | Personal | Bacteriologist / technician |
| Equipment | Blood products | |
| Equipment and supplies for the preservation and cross-linking of blood products | ||
| Tomography Room | Personal | Tomography Technician |
| Radiologist | ||
| Equipment | CT Scan Machine | |
| Intravenous Contrast | ||
| Operating Room | Personal | First Attendance Personal |
| General Surgeon | ||
| Trauma Surgeon | ||
| Anesthesiologist | ||
| Surgical Aid | ||
| Head Nurse | ||
| Circulante | ||
| On-call personnel as required | ||
| Orthopedist | ||
| Obstetrician Gynecologists | ||
| Neurosurgeon | ||
| Endoscopist | ||
| Endoscopy Technician | ||
| Equipment | Anesthesia Machine | |
| Cell Saver ® | ||
| Level 1® | ||
| Operating Table | ||
| Surgical Equipment | ||
| Vascular occlusion balloons (REBOA-REBOC) | ||
| Airway Equipment | ||
| Vascular Access and Infusion Equipment | ||
| Drugs (intravenous fluids, sedation, vasoactive and hemostatic agents) | ||
| Endoscopy Equipment | ||
| Angiography Room | Personal | Endovascular Surgeon / Interventional Radiologist |
| Perfusionist | ||
| Circulante | ||
| Equipment | Angiography Equipment | |
| Contrast | ||
| Vascular Access and Infusion Equipment | ||
| Equipment and supplies for angiography | ||
| Intensive Care Unit | Personnel, equipment and procedures associated with critical care | |
Table 2 Logistics and resources for the implementation of the trauma code
| Activation Criteria | Initial Assessment and Resuscitation | Departments that can activate the Trauma Code | Selectively activated departments according to the patient's compromise | |
|---|---|---|---|---|
| Trauma Code | Patient admitted to the emergency department with evidence of penetrating or blunt trauma, with involvement of two or more body systems or severe involvement of one or more systems or associated with hemodynamic instability (Systolic Blood Pressure ≤ 90 mmHg or Heart Rate ≥ 120 bpm). | Location: Resuscitation Room. Located 5 meters from the emergency room door. | General Surgeon. On-site 24 hours a day, immediate response. | Orthopedics: On-site 12 hours a day, immediate response. Available at night, 20-minute response. |
| First responder: Emergency physician at the head of the emergency team (general/resident physician, head nurse, nursing assistants, respiratory therapist, stretcher bearer). | Trauma Surgeon. On-site 12 hours a day, immediate response. Available during the evenings, response time 20 minutes. | Neurosurgery: On-site 12 hours a day, immediate response. Available at night, 20-minute response. | ||
| Functions: Primary and secondary assessment according to ATLS guidelines (12), trauma code activation, compressible hemorrhage control, securing airway and ventilation, eFAST, pelvic binder/ tourniquet placement, vascular access (5 Fr femoral arterial access sheath and high-flow venous catheter), crystalloid resuscitation onset, massive transfusion activation, blood products transfusion, and tetanus toxoid administration. | Blood bank: Available 24 hours a day. Located 20 meters from the emergency department. They send a trauma pack containing: 4 units of red blood cells, 4 units of plasma, and 4 units of platelets (as required). | Angiography: Interventional Radiologist and standard angiography equipment, on-site 12 hours a day, immediate response. Available at night, 20-minute response. | ||
| Adjuncts: Portable chest and pelvis X-ray. Station located 10 meters away from the emergency room. It IS transferred to the Resuscitation Room with any trauma code activation. | Tomography: Available 24 hours a day. Located 10 meters from the emergency department. Multi-detector equipment with 128 slices. | Endoscopy: Gastroenterologist endoscopist and standard endoscopy equipment, on-site 12 hours a day, immediate response. Available at night, 20-minute response. | ||
| Standard operating room equipped and prioritized by a pre-established protocol. Located one floor above the emergency department and connected by direct-access elevator with priority for the trauma code. | Obstetrics: On-site 24 hours a day, immediate response. |
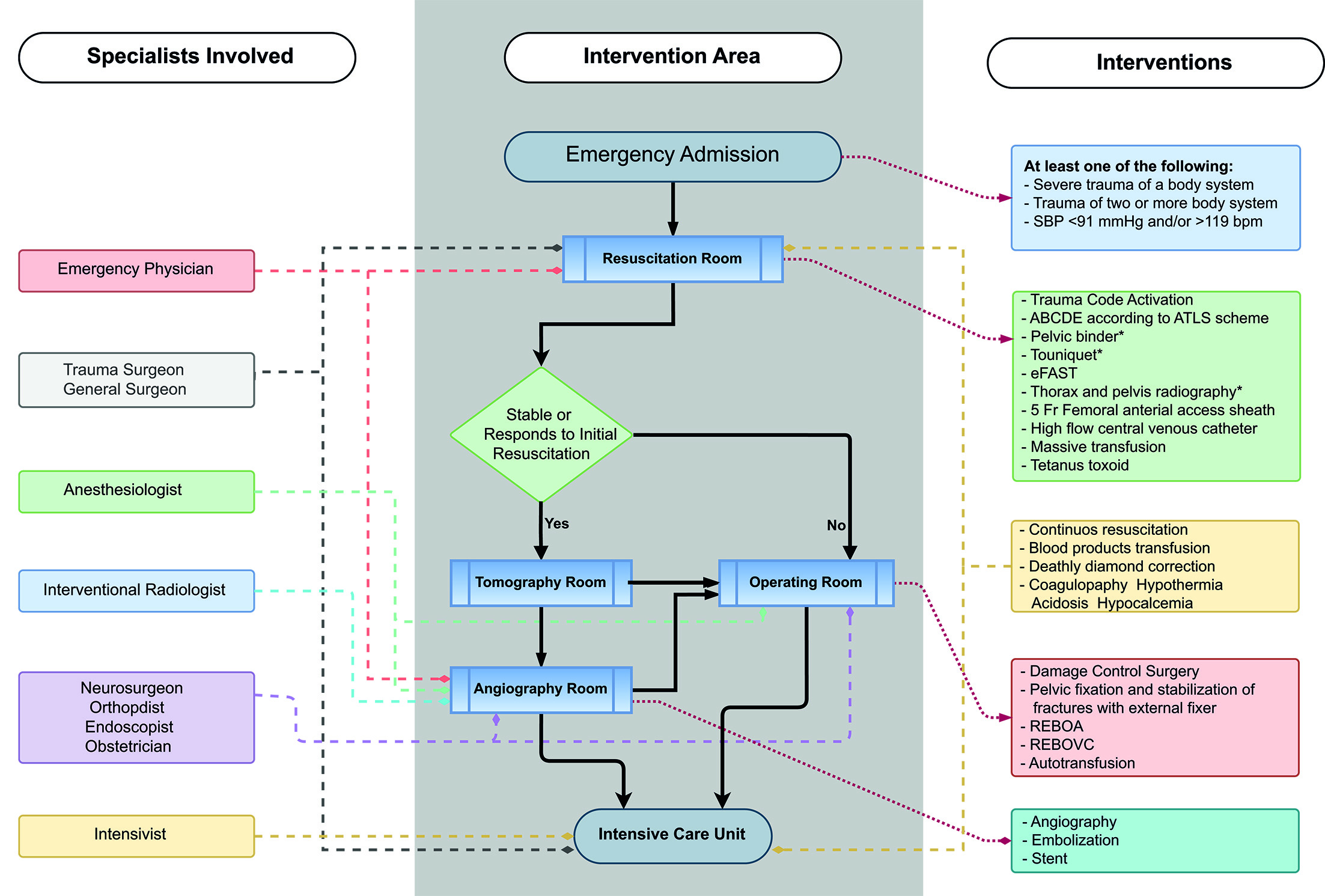
Figure 1 shows the management algorithm for the Trauma Code in a hybrid trauma service, the interventions performed in each of the dependencies and the specialists directing each intervention in every phase of the attention process.
The initial resuscitation of the patient begins at the emergency room admission and continues uninterrupted, with the trauma and acute care surgeon present in all the phases of the attention process and guiding all the diagnostic and therapeutic interventions, until the patient arrives at the intensive care unit to continue with the second phase of damage control.
Discussion
Hybrid rooms were developed to optimize the performance and precision of non-immediate surgical interventions 12,13, thus increasing the associated costs but improving the outcomes. Their use in the management of trauma patients for bleeding control was originally created and described in Japan 14, but it has been widely accepted and is currently being implemented in high complexity trauma centers around the world. It is based on a horizontal scheme that provides different therapeutic options simultaneously and in the same room, proving a benefit in survival rates and the time for bleeding control 10,15,16, increasing the technical success of advanced reanimation interventions such as the REBOA placement 17 and, in some reports, even reducing transfusion requirements, hospital stay and the number of delayed reinterventions.
The implementation of an hybrid room requires an investment that surpasses the capacity of most healthcare systems in developing countries 8. Some trauma centers with hybrid rooms have decided to include advanced angiography imaging reconstruction that can supply tomography images in some cases, avoiding the expensive cost of including a tomography equipment 18. This is the reason why very few institutions use this model in Latin America.
Nevertheless, when looking at the trauma management from a broader perspective, many of the high-level health institutions in Latin America currently have the technological tools and the human resources required for the functioning of hybrid rooms, in spite of being located in different areas or services. Therefore, it is necessary to implement a protocol that coordinates all these functions to offer the traumatized patient a continuous and uninterrupted attention, with the purpose of obtaining the benefits of a hybrid room without incurring its high construction and maintenance costs.
The adoption of this model should be made with caution, as it requires a high competence multidisciplinary team, a robust administrative base, an adequate infrastructure and the leadership of experienced trauma and acute care surgeons. The development of protocols with well-defined attention routes would guide the decision-making process for a timely management. It also requires adequate feedback mechanisms and constant pursue of mistakes in the process to decrease possible adverse events, as the management of a patient in the wrong place or moment, in the context of trauma, could lead to severe complications and even death.
Currently, Japan's experience in 15 centers has pioneered the implementation of hybrid rooms. Regarding the indicators for the implementation of hybrid rooms, it has been proposed an incidence of 150 trauma patients with an Injury Severity Score >16 per year. A cost-effectiveness study regarding the implementation of hybrid rooms was conducted in Japanese hospitals, estimating a benefit of 1.03 quality-adjusted life years (QALYs) with an incremental cost-effectiveness ratio (ICER) of US$35,552 per QALY. The analysis estimated that the implementation of an hybrid room has a probability of 79.3% of being cost-effective 19,20.
Conclusion
Hybrid emergency rooms have shown a benefit in survival rates and a decrease in trauma bleeding control times. Its implementation requires cutting-edge technology, educational programs for the personnel and infrastructure adequation and maintenance. However, the implementation of a hybrid service with a vertical approach, or a “functional hybrid service”, for the management of severe trauma patients in high complexity centers, could reach similar results to the hybrid rooms with horizontal systems, without the elevating costs.











 texto em
texto em